Abstract
Although 70-80% of Acute Myeloid Leukemia (AML) patients achieve complete remission with the induction therapy consisting of a combination of Cytarabine (Ara-C) and Daunorubicin (Dnr), the overall survival is dismal with disease relapse, drug resistance and toxicities as the major causes of treatment failure. Single agent arsenic trioxide (ATO) used in acute promyelocytic leukemia (APL or AML-M3) is associated with relatively less toxicities which suggest the possibility of extending its use to elderly non M3-AML patients. But ATO trials in non-M3 AML were not encouraging enough to devise ATO as a better treatment option. NF-E2 related factor 2 (NRF2) has been recognised as one of the key molecules associated with resistance towards chemotherapeutic agents in cancer. Leukemic cells owing to their genomic instability and altered metabolism are known to maintain high reactive oxygen species (ROS) levels. NRF2 as a redox dependent transcription factor drives the expression of several antioxidant genes like NAD(P)H quinone oxidoreductase1 (NQO1), heme oxygenase1 (HMOX1), glutamate-cysteine ligase (GCL) and glutathione-S-transferases (GSTs) which coordinate to scavenge ROS. Although the role of NRF2 in resistance to cytarabine and daunorubicin has been reported previously, its role in ATO resistance in non M3-AML has not been addressed before. Also, the role of pharmacological inhibition of NRF2 in modulating resistance to ATO and other conventional therapeutic agents in AML has not been tested.
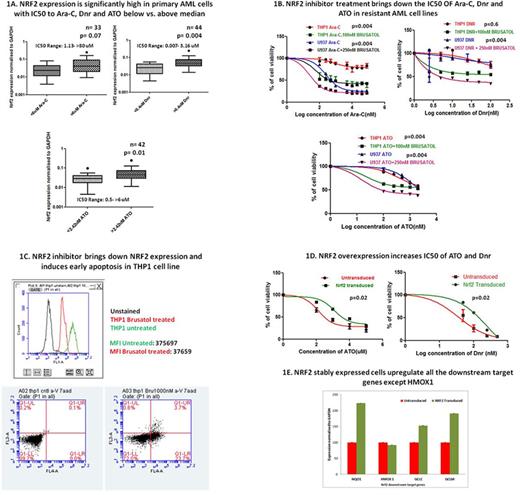
To investigate whether NRF2 expression is associated with in-vitro sensitivity to chemotherapeutic drugs, NRF2 RNA expression in primary AML samples grouped according to their median Ara-C, Dnr and ATO IC50 (median IC50 6uM for Ara-C, 0.4µM for Dnr and 2.42µM for ATO) were compared. Primary AML samples with Ara-C, Dnr or ATO IC50 below median had significantly low NRF2 RNA expression compared to those above median (p=0.07, 0.004 and 0.01, respectively) (Fig1-A). Comparison of NRF2 expression in a subset of samples that were above median IC50 to both ATO and Dnr with those below median also showed similar trend. Flow cytometric evaluation of NRF2 expression in Ara-C, Dnr and ATO resistant AML cell lines (THP1 and U937) showed higher intracellular NRF2 levels (MFI=37.18 and 46.56) compared to sensitive cell lines (HL60 and MOLM13) (MFI=6.25 and 28.9). Treatment of resistant AML cell lines expressing high levels of NRF2 (THP1 and U937) with pharmacological inhibitor of NRF2 {Brusatol} followed by ATO (0.1-6uM), Ara-C (0.1uM-80uM) and Dnr (25nM-2000nM) improved their sensitivity to these drugs (Fig1-B) The effect of Brusatol in inhibiting NRF2 protein levels and its role in inducing apoptosis were also demonstrated by flow cytometry (Fig1-C). To further confirm the role of NRF2 in drug resistance, AML cell lines (MOLM13 and HL60) stably over expressing NRF2 was established. Overexpression was done using lentiviral expression system followed by blasticidin selection, further confirmed by immunoblot and quantitative real time PCR. The overexpressed cell lines showed increased resistance to ATO/ Dnr and Ara-C (Fig1-D) and up-regulation of NRF2 downstream targets compared to un-transduced cells (Fig1-E).
Our results suggest that NRF2 plays a pivotal role in drug resistance and hence could be an ideal druggable target in AML, more so to the drugs that functions through ROS. Our data as well growing evidence from other malignancies suggest the possibility of using NRF2 inhibitors in combination with chemotherapeutic agents to combat drug resistance.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal