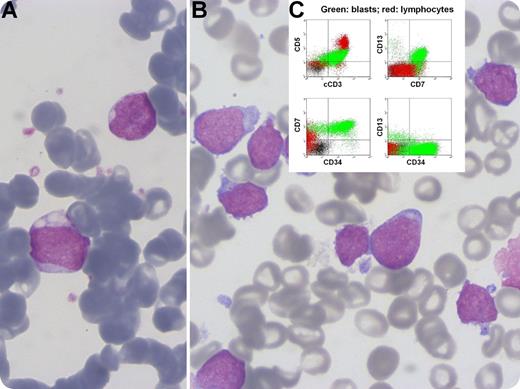
A 63-year-old man presented with an enlarged left cervical lymph node. Complete blood count showed hemoglobin 14.3 g/L, mean corpuscular volume 101 fL, white blood cells 3.26 × 109/L, absolute neutrophil count 1.87 × 109/L, and platelets 90 × 109/L. Ten years ago, he was diagnosed with acute myeloid leukemia subtype M1 with a normal karyotype. At that time, blasts had a medium to high nuclear:cytoplasmic (N:C) ratio, irregular nuclei, and sporadic vacuolation (panel A). He initially achieved complete response (CR) with cytarabine plus idarubicin (7 + 3 regimen), relapsed at 6 months, and reattained CR with salvage regimens plus gemtuzumab ozogamicin. Marrow aspirate now revealed small and medium-size blasts with a high N:C ratio, cytoplasmic blebs, and round nuclei with conspicuous nucleoli and frequent hand-mirror configuration (panel B). Immunophenotypically blasts were CD34+, CD7+, cytoplasmic CD3+, CD5+, CD13+, and CD1a– (panel C), and lymph node biopsy demonstrated complete architectural effacement by a diffuse infiltrate of large and medium-size blasts expressing CD3, CD10, CD7, and CD99, which established the diagnosis of precursor T-cell acute lymphoblastic leukemia/lymphoma. Two distinct clones were identified by conventional karyotyping, one bearing the interstitial deletion del(11)(q14q22) and the other bearing trisomy 21.
This very rare case of leukemia reemergence after a 10-year remission illustrates the complex pathobiology of leukemogenesis and underscores the importance of immunophenotyping when morphology is not unambiguous.
A 63-year-old man presented with an enlarged left cervical lymph node. Complete blood count showed hemoglobin 14.3 g/L, mean corpuscular volume 101 fL, white blood cells 3.26 × 109/L, absolute neutrophil count 1.87 × 109/L, and platelets 90 × 109/L. Ten years ago, he was diagnosed with acute myeloid leukemia subtype M1 with a normal karyotype. At that time, blasts had a medium to high nuclear:cytoplasmic (N:C) ratio, irregular nuclei, and sporadic vacuolation (panel A). He initially achieved complete response (CR) with cytarabine plus idarubicin (7 + 3 regimen), relapsed at 6 months, and reattained CR with salvage regimens plus gemtuzumab ozogamicin. Marrow aspirate now revealed small and medium-size blasts with a high N:C ratio, cytoplasmic blebs, and round nuclei with conspicuous nucleoli and frequent hand-mirror configuration (panel B). Immunophenotypically blasts were CD34+, CD7+, cytoplasmic CD3+, CD5+, CD13+, and CD1a– (panel C), and lymph node biopsy demonstrated complete architectural effacement by a diffuse infiltrate of large and medium-size blasts expressing CD3, CD10, CD7, and CD99, which established the diagnosis of precursor T-cell acute lymphoblastic leukemia/lymphoma. Two distinct clones were identified by conventional karyotyping, one bearing the interstitial deletion del(11)(q14q22) and the other bearing trisomy 21.
This very rare case of leukemia reemergence after a 10-year remission illustrates the complex pathobiology of leukemogenesis and underscores the importance of immunophenotyping when morphology is not unambiguous.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal