Abstract
Abstract 4835
Sickle cell anemia (SCA) is characterized by a chronic inflammatory state in which oxidative stress, particularly in the endothelium, exerts a strong influence on the pathogenesis of vaso-occlusion and may be implicated in patients' clinical heterogeneity and survival. It has been suggested that the cytokine production profile of cells involved in the immune response may vary among patients with SCA. Leg ulcers (LU) represent a severe complication in these patients, and this condition has been associated with specific end-organ damage and an increase in morbidity and mortality. Recent studies have shown that venous obstruction, endothelial dysfunction, coagulopathy and infections are implicated in the complex pathogenesis of LU.
To determine IL-1β, IL-6 and IL-8 plasma levels and gene expression rates as well as hematological and coagulation parameters and correlate these with the history of LU in adult SCA patients followed up at HEMOPE, in the state of Pernambuco, northeastern Brazil.
Peripheral blood samples from 92 patients (median age 27 years; 42 female; 52 male; all Afro-descendants) in the steady state who had been diagnosed with SCA (HbSS), had not received a transfusion and were not using hydroxyurea were analyzed. Plasma levels of cytokines were determined by ELISA, and the gene expression rates by qRT-PCR. The patients' clinical and laboratorial characteristics were obtained from their medical charts. Statistical analysis was performed using the SAS System for Windows version 9.2.
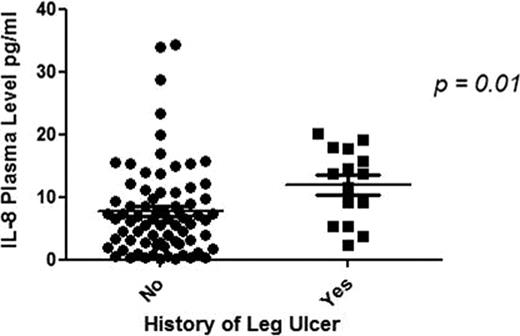
Median age was higher in patients with a history of LU than in those without a history (33.1 vs. 28.4; p = 0.04). Although no statistically significant (p = 0.5) differences in IL-8 gene expression rates were observed, IL-8 plasma levels were significantly higher in patients with a history of LU than in patients without a history (23.8 vs. 7.7; p = 0.01) (Figure 1). Thus, patients with high levels of IL-8 had an increased risk for the occurrence of leg ulcers (OR = 1.01; 95% CI = 1.00–1.02). The ROC curve showed that IL-8 levels higher than 8.55 pg/mL could indicate the presence of LU (accuracy = 71.6%; sensitivity = 73.7%; specificity = 68.5%). The laboratory tests revealed reticulocyte counts and activated partial thromboplastin time (aPTT) ratios (R) that were significantly higher in patients with a history of LU than in those without a history (11.8 vs. 8.4, p = 0.01; 1.1 vs. 0.9, p = 0.04, respectively). Both the higher reticulocyte counts and R values were associated with increased risk for the occurrence of leg ulcers in these patients (OR = 1.12, 95% CI = 1.02 – 1.20; OR = 24.28, 95% CI = 1.20 – 486.09, respectively).
In this study, patients who had had LU at some time in their lives showed significantly higher IL-8 levels, reticulocyte counts and R values than patients who had never had LU. Our results therefore suggest a relationship between the parameters described above and LU in patients with SCA. These parameters could perhaps be used, in association with different genetic modulators that may contribute to different clinical phenotypes observed in this disease, as markers of this clinical manifestation of SCA or of a propensity to develop it.
IL-8 plasma levels in two groups of patients with sickle cell anemia. The levels on the left are for patients who had never had leg ulcers while those on the right are for patients who had had leg ulcers at some time in the past. Data are represented as means ± SEM.
IL-8 plasma levels in two groups of patients with sickle cell anemia. The levels on the left are for patients who had never had leg ulcers while those on the right are for patients who had had leg ulcers at some time in the past. Data are represented as means ± SEM.
Financial Support: CAPES (Brazil)/FAPESP/CNPq/INCTS
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal