Abstract
The aim of the current study was to identify cytogenetic risk factors as detected by iFISH in light chain (AL) amyloidosis. We analyzed a cohort of 91 consecutive patients receiving first-line chemotherapy according to the melphalan / dexamethasone protocol (M-Dex) (Palladini et al., Blood 2004, Dietrich et al., Blood 2010). Our study population consisted of patients not eligible for high dose chemotherapy due to age, reduced general health and the severity of heart involvement. Accordingly, the median age was 67 years (range 40 – 77 years), the median Karnofsky index 80% (50% – 90%), the median number of involved organs 2 (range: 1 – 6). 71/91 (78%) patients had cardiac involvement, among them 45 with NYHA stage III/IV. The median NTproBNP values were 4004 ng/l (range 71–48.292) ng/l, the median dFLC – designating the differential between the involved minus the uninvolved serum free light chain – was 204 mg/l (range 1 – 3.888 mg/l). The estimated median follow-up since start of M-Dex was 38 months.
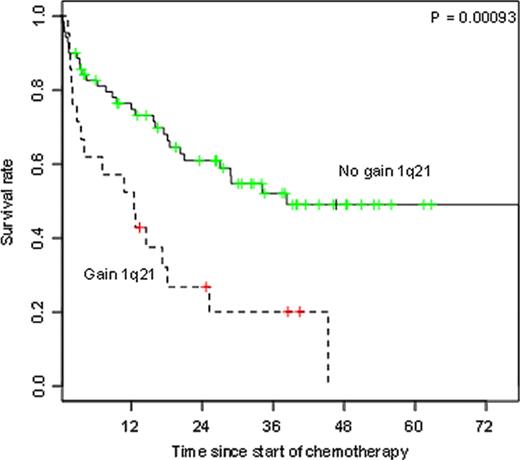
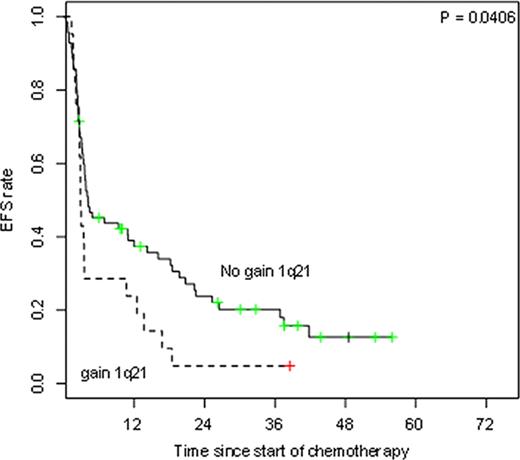
Translocation t(4;14) and deletion del17p13, which have been established as indicators of poor prognosis in multiple myeloma, are very rarely detected in AL amyloidosis (Bochtler et al., Blood 2008). In this study cohort we could only detect 4 out of 91 patients (4%) with at least one of these two cytogenetic aberrations. We therefore focused on gain of 1q21, which has also been described as an adverse prognostic factor in multiple myeloma and is more prevalent in AL amyloidosis (Bochtler et al., Blood 2011). Accordingly, 21/91 patients (23%) in our study cohort tested positive for gain of 1q21. The patient groups with and without gain of 1q21 were comparable regarding age, Karnofsky index, number of involved organs and the NTproBNP values to account for cardiac involvement. However, dFLC was higher in gain of 1q21 positive patients (table 1 ).
| Factor (median) . | Gain 1q21 . | No gain 1q21 . | p . |
|---|---|---|---|
| Age | 69 | 66 | 0.17 |
| Karnofsky Index | 75 | 80 | 0.70 |
| Number of involved organs | 2 | 3 | 0.30 |
| NT-proBNP | 4251 | 4004 | 0.81 |
| dFLC | 280 | 154 | 0.01 |
| Factor (median) . | Gain 1q21 . | No gain 1q21 . | p . |
|---|---|---|---|
| Age | 69 | 66 | 0.17 |
| Karnofsky Index | 75 | 80 | 0.70 |
| Number of involved organs | 2 | 3 | 0.30 |
| NT-proBNP | 4251 | 4004 | 0.81 |
| dFLC | 280 | 154 | 0.01 |
In multivariate analysis we tested the prognostic significance of gain of 1q21 in comparison with established hematologic and clinical parameters including age, gender, kappa versus lambda light chain restriction, the detection of an intact immunoglobulin, dFLC values, Karnofsky index, number of involved organs and NTproBNP values using the proportional hazards model of Cox. Markedly, gain of 1q21 was confirmed as a strong predictor of poor outcome for OS (p<0.001), along with Karnofsky index, NTproBNP and age (p=0.03, p<0.001 and p=0.05, respectively). Again, statistical significance for gain of 1q21 and NTproBNP was also observed for EFS (p=0.04 and p=0.03, resp.).
In conclusion, we have identified gain of 1q21 for the first time as an independent adverse risk factor in AL amyloidosis in a patient cohort with advanced disease uniformly treated with the standard therapy M-Dex. The poor outcome in these patients seems to be attributable to a worse responsiveness of the plasma cell clone to M-Dex. Further studies are required to test whether the poor prognosis conferred by gain of 1q21 is inherent with this cytogenetic aberration irrespective of the chosen therapy regimen or whether the poor prognosis can be overcome by alternative treatment strategies in these high risk patients.
No relevant conflicts of interest to declare.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal