Abstract
Although the effects of type II-IFN (IFN-γ) on GVHD and leukemia relapse are well studied, the effects of type I-interferon (type I-IFN, IFN-α/β) remain unclear. We investigated this using type I-IFN receptor-deficient mice and exogenous IFN-α administration in established models of GVHD and GVL. Type I-IFN signaling in host tissue prevented severe colon-targeted GVHD in CD4-dependent models of GVHD directed toward either major histocompatibility antigens or multiple minor histocompatibility antigens. This protection was the result of suppression of donor CD4+ T-cell proliferation and differentiation. Studies in chimeric recipients demonstrated this was due to type I-IFN signaling in hematopoietic tissue. Consistent with this finding, administration of IFN-α during conditioning inhibited donor CD4+ proliferation and differentiation. In contrast, CD8-dependent GVHD and GVL effects were enhanced when type I-IFN signaling was intact in the host or donor, respectively. This finding reflected the ability of type I-IFN to both sensitize host target tissue/leukemia to cell-mediated cytotoxicity and augment donor CTL function. These data confirm that type I-IFN plays an important role in defining the balance of GVHD and GVL responses and suggests that administration of the cytokine after BM transplantation could be studied prospectively in patients at high risk of relapse.
Introduction
Although allogeneic BM transplantation is curative therapy for a majority of hematologic malignancies, its application has been limited by the development of GVHD. GVHD is the result of immunologic damage to the host tissue by alloreactive T cells from the incoming donor graft. Unfortunately, the development of detrimental GVHD is closely intertwined with therapeutic GVL responses. GVL responses are important for eradication of residual host malignancy and are primarily mediated by alloreactive donor T and natural killer (NK) cells. Therapeutic approaches to separate these phenomena are urgently needed.
The IFNs were first discovered as a result of their capacity to confer cell resistance to viral infection.1 There are 2 distinct IFN types, type I and type II, and although both groups induce antiviral defense mechanisms in cells, primarily by limiting replication, they exhibit distinct immunologic properties. After allograft rejection, it is well established that the type II-IFN, IFN-γ, is a dominant Th1 cytokine, exerting pleotropic effects on both hematopoietic and nonhematopoietic cells. Importantly, IFN-γ has differential effects on both donor and host tissue, with a protective role dominating within GVHD of the lung and pathogenic effects dominating in the gastrointestinal tract.2-4 In addition, the cellular subsets producing IFNγ and the timing of production may also impact the effect of the cytokine after BM transplantation.5 In contrast, the role of type I-IFN after BM transplantation remains largely unknown.
All type I-IFNs act through the same receptor, which is composed of 2 subunits, IFNAR1 and IFNAR2,6 and is expressed on essentially all cells.7 The type I-IFNs encompass a large family of cytokines that include a single IFN-β isotype, > 13 IFN-α isotypes, and multiple other less-described subtypes.8 It has been demonstrated that some IFN subtypes show greater activity than others, with a good correlation between antiviral activities and antiproliferative effects. However, given that they signal through the same receptor complex, it is not understood how this might occur.9 To address the question of the role of type I-IFNs after BM transplantation, we used mice deficient in the IFNAR1 component of the type I-IFN receptor as donors or recipients after myeloablative conditioning. We demonstrate that type I-IFN signaling in recipients protects from CD4-dependent GVHD, whereas donor signaling augments protective GVL responses. These studies suggest that carefully timed administration of this cytokine in the clinical BM transplantation setting may be beneficial.
Methods
Mice
Female C57Bl/6j (B6.WT, H-2b, CD45.2+), B6.Ptprca (H-2b, CD45.1+), B6D2F1 (H-2b/d), and BALB/c (H-2d, CD45.2+ or CD45.1+ for engraftment studies) mice were purchased from the Animal Resources Center. C3H.SW (H-2b) mice were purchased from The Jackson Laboratory. B6.C-H2bm1 (bm1, CD45.2+) mice were supplied by the Walter and Elisa Hall Institute. B6luc+ and BALB/cluc+ mice were provided by Robert Negrin10 and Remi Creusot,11 respectively (Stanford University). B6.IFNAR1−/− and B6.IL-17A−/− mice were generated by Paul Hertzog (Monash University) and Yoichiro Iwakura (University of Tokyo), respectively.12,13 The age of mice used ranged between 8 and 14 weeks. Mice were housed in microisolator cages and received acidified autoclaved water (pH 2.5) after transplantation. All mouse experiments were performed under the approval of the Queensland Institute of Medical Research Animal Ethics Committee.
BM transplantation
On day −1, mice received 1100 cGy (B6D2F1) or 1000 cGy (B6) total body irradiation (137Cs source at 108 cGy/min) split into 2 doses separated by 3 hours. On day 0, B6D2F1 recipients underwent transplantation with BM with or without T cells (purified by magnetic bead depletion as previously described2 ) from B6 (107 BM; 2 × 106 T) donors, and B6 recipients underwent transplantation with grafts from C3H.SW (107 BM; unseparated T cells containing 2 × 106 CD8+T), bm1 (5 × 106 BM; 5 × 106 T), or BALB/c (107 BM; 5 × 106 T) donors. The C3H.SW donors only were immunized with 2 × 107 B6 splenocytes 2 weeks before harvest for the GVHD studies to allow the generation of significant disease.4 Mice were monitored daily, and those with GVHD clinical scores2 ≥ 6 were killed, with the date of death recorded as the next day in accordance with institutional animal ethics guidelines. To generate BM chimeras, we transplanted 5 × 106 T-cell depleted (TCD: performed as previously described2 ) BM into lethally irradiated (1000 cGy) mice and allowed them to reconstitute over the course of 3-4 months.
Histopathology of GVHD target organs
At day 7 after transplantation, GVHD target tissues were harvested, formalin-preserved, embedded in paraffin, and processed to generate 5-μm-thick sections. H&E-stained sections of colon, small intestine, lung, and liver were examined in a blinded fashion (by A.D.C.) with the use of a semiquantitative scoring system for GVHD as previously published.14 Images were acquired with a Leica DFC295 camera and Leica Application Suite Version 3.3.0 software (Leica Micro-systems) and viewed with an Olympus BX51 microscope (Olympus).
MLC for conventional dendritic cell functional analysis
B6.WT and B6.IFNAR1−/− mice were irradiated and CD11c+ cells sort purified (MoFlo; Beckman Coulter) 24 hours later. 105 BALB/c CD4+ T cells (sort purified) were cultured with 104 CD11c stimulators for 120 hours. T-cell proliferation was assessed by adding 3H-thymidine for the final 12-18 hours of culture.
IFN-α treatment
Recombinant murine IFN-α1 that was produced in Pichia pastoris and purified by reverse phase HPLC was kindly provided by P. Hertzog. For analysis of the effects of IFNα treatment on host tissue, recipients were treated on day −1, after the second irradiation, with 100,000 U delivered subcutaneously. For analysis of the effects of IFNα treatment on GVL responses, mice were monitored until there were low levels of detectable tumor (< 106 p/s/cm2/sr) and then treated every other day with 100 000 U delivered subcutaneously.
mAbs
The following mAbs were purchased from BioLegend: PE-conjugated CD45.1 (A20) and CD11c (N418), allophycocyanin (APC)–conjugated anti–IL-17A (TC11-18H10.1) and IgG2b isotype, APC-conjugated anti–IFN-γ (XMG1.2) and IgG2b isotype, PE-Cy5–conjugated CD8 (53-6.7) and IgG2b isotype control, and APC-conjugated IFNAR1 (MAR1-SA3). Granzyme B mAb (MHGB05) was purchased from Invitrogen. FITC-conjugated I-A/I-E (2G9) was purchased from BD Biosciences. Biotin-conjugated Thy1 (HO-13-4) and FITC-conjugated CD3 (KT3) and CD4 (GK1.5) were produced in-house.
CFSE labeling
CFSE was purchased from Sigma-Aldrich. Purified T cells were suspended at 30 × 106 cells/mL in serum-free media and CFSE added at 1μM final concentration. Cells were incubated at 37°C for 10 minutes and washed in media containing 2% FCS. Cells were analyzed by FACSCanto (BD Biosciences) and proliferation indices determined by the use of ModFit LT 3.2 cell cycle analysis software (Verity Software House).
In vivo cytotoxicity assays
In vivo cytotoxicity assays were performed as previously described.15 In brief, at 12 days after transplantation mice received (1) 2 × 107 congenic donor type PTPrca (CD45.1+)–unlabeled splenocytes and 2 × 107 host type B6D2F1 CFSE-labeled splenocytes or (2) 2 × 107 congenic B6.Ptprca (CD45.1+)–unlabeled splenocytes and 2 × 107 IFNAR1−/− (CD45.2+) CFSE-labeled splenocytes. Eighteen hours later, splenocytes were stained with PE-conjugated CD45.1. The proportion of CD45.1+ cells to CFSE+ cells was determined by FACS and the in vivo cytotoxicity index defined as percentage of CD45.1+ cells compared with remaining CFSE+ cells.
In vitro CTL: chromium release assay
Target tumor cells (EL4) were labeled with 51Cr and cultured with donor sort purified CD8+ effectors for 5 hours at 37°C and 5% CO2. Chromium release into supernatants was measured with a γ counter. Spontaneous release was determined from wells containing targets only and total release from those wells containing targets and 1% SDS. Percentage cytotoxicity was defined as percent cytotoxicity = (experimental release − spontaneous release) / (total release − spontaneous release) × 100.
Tumor challenge
The tumor lines P815 (H-2Dd, DBA/2), EL4 (H-2Db, B6), P210 (H-2Dk, C3H), A20 (H-2Db, Balb/c), and 5GTM1 (H-2Dd, C57BL/KaLwRij) were used for experiments. The luciferase-transfected mastocytoma cell line P815 or EL4 was injected intravenously into B6D2F1 or B6 recipients, respectively, on the day of transplantation. Survival and clinical scores were monitored. Mice were imaged weekly by use of the Xenogen imaging system (Xenogen IVIS 100; Caliper Life Sciences) to determine the level of tumor burden. Leukemic death was defined as a significant tumor burden assessed by imaging (> 106 photons/s/cm2/sr) and/or the development of hind-limb paralysis (because of P815 chloromas within vertebrae). GVHD death was defined as low tumor burden (< 106 photons/s/cm2/sr) and significant GVHD scores (> 5).
Intracellular cytokine analysis
Cells were stimulated for 4 hours with phorbol-12-myristate-13-acetate (50 ng/mL) and ionomycin (500 ng/mL), with brefeldin added for the final 2 hours. The cells were then surface-labeled with CD8 Pe-Cy5 and Thy1 bio-SAPe-Cy7 and processed for intracellular staining of IL-17 and IFN-γ by use of the BD Cytofix/cytoperm kit (BD Biosciences) as per the manufacturer's instructions. Labeled cells were analyzed by flow cytometry (FACSCanto; BD Biosciences).
Serum cytokine analysis
Serum cytokine levels were analyzed by the use of BD cytometric bead array flex set (BD Pharmingen). All assays were performed according to the manufacturer's instructions.
Statistical analysis
Column graphs shown represent mean, with error bars demonstrating SEM. Statistical significance was determined by the use of 2-tailed Mann-Whitney U tests or Wilcoxon matched pairs test with a P < .05. Survival curves were generated as Kaplan-Meier estimates and compared by log-rank analysis. All statistical analyses were performed with GraphPad Prism Version 5.0b (GraphPad Software).
Results
Type I-IFN signaling in BM transplantation recipients increases survival after MHC-mismatched BM transplantation
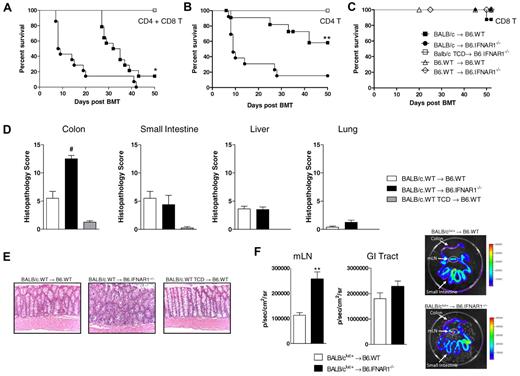
To identify the role of type I-IFN signaling in recipients after BM transplantation, we transplanted BM and T cells from BALB/c.WT donors into lethally irradiated B6.WT or B6.IFNAR1−/− recipients. GVHD was significantly increased in recipients unable to respond to type I-IFN relative to B6.WT recipients (Figure 1A). This early increase in GVHD in IFNAR1−/− recipients was CD4 dependent, as demonstrated by the transplantation of CD4+ T cells only within the donor graft (Figure 1B). Importantly, at the time of GVHD mortality, WT and IFNAR1−/− recipients had equivalent levels of donor engraftment (donor CD4+: 98.7% ± 0.5% vs 96.7% ± 1.6% respectively, P = .3). After transplantation of CD8+ T cells only in the donor graft there was development of low-grade GVHD, and no difference was observed between WT or IFNAR1−/− recipients when assessed by survival (Figure 1C) or clinical scores (day 50 = 0.7 ± 0.7 vs 0 ± 0, respectively, P = NS).
Type I-IFN signaling inhibits colon-targeted GVHD in a MHC-mismatched model of BM transplantation. Survival of lethally irradiated B6.WT or B6.IFNAR1−/− mice undergoing transplantation at day 0 with 107 BM and either (A) 5 × 106 CD3+ T cells (*P < .05 B6.WT vs B6.IFNAR1−/−), (B) 3 × 106 CD4+ T cells only (**P < .01, B6.WT vs B6.IFNAR1−/−), or (C) 2 × 106 CD8+ T cells only from BALB/c.WT donors. In panel C, syngeneic groups received 107 BM and 5 × 106 CD3+ T cells from B6.WT donors. Combined data from 2 experiments; n = 13-14 in BM + T groups, n = 4-6 in TCD or syngeneic control groups. (D) After transplantation as in panel A, histology samples were taken at day 7 and GVHD histopathology quantified in the target organs, colon (#P < .005, B6.WT vs B6.IFNAR1−/−), small intestine, liver, and lung. Scores are 0 in TCD, where no bars are seen. (E) Representative images of colon histology (×250 magnification). (F) Lethally irradiated B6.WT or B6.IFNAR1−/− recipients received BALB/c.WT BM (107) + BALB/cluc+ T cells (5 × 106). Luminescence was quantified at day 7 after transplantation in mLN and GI tract as shown (**P < .01, n = 5 per group).
Type I-IFN signaling inhibits colon-targeted GVHD in a MHC-mismatched model of BM transplantation. Survival of lethally irradiated B6.WT or B6.IFNAR1−/− mice undergoing transplantation at day 0 with 107 BM and either (A) 5 × 106 CD3+ T cells (*P < .05 B6.WT vs B6.IFNAR1−/−), (B) 3 × 106 CD4+ T cells only (**P < .01, B6.WT vs B6.IFNAR1−/−), or (C) 2 × 106 CD8+ T cells only from BALB/c.WT donors. In panel C, syngeneic groups received 107 BM and 5 × 106 CD3+ T cells from B6.WT donors. Combined data from 2 experiments; n = 13-14 in BM + T groups, n = 4-6 in TCD or syngeneic control groups. (D) After transplantation as in panel A, histology samples were taken at day 7 and GVHD histopathology quantified in the target organs, colon (#P < .005, B6.WT vs B6.IFNAR1−/−), small intestine, liver, and lung. Scores are 0 in TCD, where no bars are seen. (E) Representative images of colon histology (×250 magnification). (F) Lethally irradiated B6.WT or B6.IFNAR1−/− recipients received BALB/c.WT BM (107) + BALB/cluc+ T cells (5 × 106). Luminescence was quantified at day 7 after transplantation in mLN and GI tract as shown (**P < .01, n = 5 per group).
To confirm these effects were not a result of differential susceptibility to irradiation, we included both B6.WT and B6.IFNAR1−/− recipients of syngeneic grafts as controls, which all survived long term after BM transplantation (Figure 1C). When GVHD histopathology was quantified in target organs, the accelerated mortality in B6.IFNAR1−/− recipients was shown to be because of a selective induction of severe GVHD within the colon (Figure 1D-E). To determine whether this was associated with an increase in donor T-cell infiltration within the gastrointestinal tract, we performed transplants with T cells from BALB/cluc+ donors. When we imaged recipients at day 7 after transplantation, there was increased T-cell expansion within the mesenteric lymph node (mLN) in B6.IFNAR1−/− recipients (Figure 1F). Although no difference in T-cell infiltration into the whole GI tract was observed (Figure 1F), the predominant signal was from the small intestine and thus the assay was unable to detect differences in T-cell infiltrate selectively within the colon.
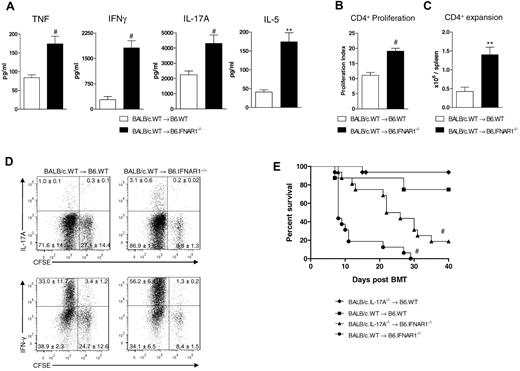
We next evaluated inflammatory cytokine levels in B6.IFNAR1−/− recipients during GVHD. This demonstrated significant increases in IFN-γ, TNF, IL-17A, and IL-5 in serum in the first week after transplant (Figure 2A). When assessed by CFSE dilution 4 days after transplantation, donor CD4+ T cells from B6.IFNAR1−/− recipients were shown to undergo enhanced proliferation (Figure 2B), were present at significantly greater numbers in the spleen (Figure 2C), and produced more IFN-γ and IL-17A (Figure 2D). In contrast, donor Treg numbers in the spleen were increased in B6.IFNAR1−/− recipients (4.5 × 104 ± 0.3 × 104 vs 3.1 × 104 ± 0.2 × 104, P = .03), suggesting that type I-IFN was not accelerating acute GVHD by inhibiting expansion of this regulatory population. Thus, the IFNAR1−/− recipients of allogeneic grafts die within the first 10 days after BM transplantation with histologic confirmation of severe GVHD within the colon concurrent with high levels of inflammatory cytokines, consistent with the effector pathway known to be critical for gut GVHD.16 To assess the contribution of increased IL-17A production by donor CD4+ T cells to the development of GVHD, we performed transplantations in which the donor graft was unable to produce IL-17A. This attenuated much of the enhanced GVHD in the absence of type I-IFN signaling; however, survival was still not equivalent to that in B6.WT recipients, indicating other factors, likely the high concurrent levels of Th1 cytokines also contributed to the enhanced GVHD (Figure 2E).
Type I-IFN signaling prevents donor T-cell proliferation and differentiation after transplantation. Lethally irradiated B6.WT or B6.IFNAR1−/− mice were transplanted with WT.BALB/c BM and CD3+ T cells. (A) Sera were taken from mice at day 4 (IFN-γ) and day 7 (TNF, IL-17A, and IL-5) and cytokine levels quantified by cytometric bead array (IFN-γ, TNF, and IL-5) or ELISA (IL-17) 4 days after transplantation with BALB/c.WT BM and BALB/c.CD45.1+ CFSE-labeled donor cells. (B) Proliferation indices of donor CD4+ T cells in the spleen were calculated with ModFit Version LT3.2 software (combined data from 2 experiments; #P < .005; n = 8 per group). (C) Donor CD4+ T cells were enumerated in the spleen (combined data from 2 experiments; **P < .01; n = 8 per group), and (D) stimulated for 5 hours ex vivo and stained for IFNγ and IL-17A (plots representative of 2 experiments and displayed as mean ± SEM, n = 8 per group). (E) Survival of lethally irradiated B6.WT or B6.IFNAR1−/− mice undergoing transplantation with 107 BM and 5 × 106 CD3+ T cells from either BALB/c.WT or BALB/c.IL-17A−/− donors (#P < .001, BALB/c.IL-17A−/−→B6.IFNAR1−/− vs both BALB/c.WT → B6.IFNAR1−/− and BALB/c.IL-17A−/− → B6.WT; survival curves are Kaplan-Meier estimates from 2 experiments; n = 8-16 per group).
Type I-IFN signaling prevents donor T-cell proliferation and differentiation after transplantation. Lethally irradiated B6.WT or B6.IFNAR1−/− mice were transplanted with WT.BALB/c BM and CD3+ T cells. (A) Sera were taken from mice at day 4 (IFN-γ) and day 7 (TNF, IL-17A, and IL-5) and cytokine levels quantified by cytometric bead array (IFN-γ, TNF, and IL-5) or ELISA (IL-17) 4 days after transplantation with BALB/c.WT BM and BALB/c.CD45.1+ CFSE-labeled donor cells. (B) Proliferation indices of donor CD4+ T cells in the spleen were calculated with ModFit Version LT3.2 software (combined data from 2 experiments; #P < .005; n = 8 per group). (C) Donor CD4+ T cells were enumerated in the spleen (combined data from 2 experiments; **P < .01; n = 8 per group), and (D) stimulated for 5 hours ex vivo and stained for IFNγ and IL-17A (plots representative of 2 experiments and displayed as mean ± SEM, n = 8 per group). (E) Survival of lethally irradiated B6.WT or B6.IFNAR1−/− mice undergoing transplantation with 107 BM and 5 × 106 CD3+ T cells from either BALB/c.WT or BALB/c.IL-17A−/− donors (#P < .001, BALB/c.IL-17A−/−→B6.IFNAR1−/− vs both BALB/c.WT → B6.IFNAR1−/− and BALB/c.IL-17A−/− → B6.WT; survival curves are Kaplan-Meier estimates from 2 experiments; n = 8-16 per group).
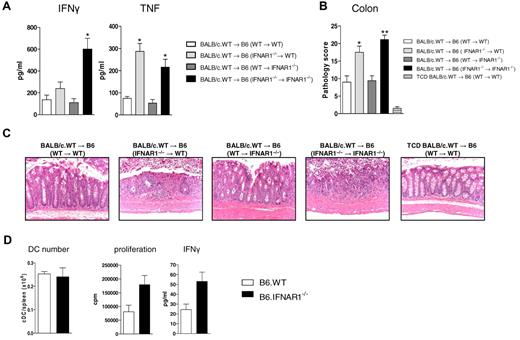
Type I-IFN signaling in the hematopoietic compartment of BM transplantation recipients is responsible for protection from GVHD
To determine whether type I-IFN signaling in the hematopoietic or parenchymal compartment of BM transplantation recipients was responsible for protection from GVHD, BM chimeras were used as secondary recipients. When serum cytokine levels were assessed at day 4 (IFN-γ) and day 7 (TNF) after transplantation, increased levels were found in recipient chimeras in which both the hematopoietic and parenchymal system lacked IFNAR1 and in which the hematopoietic system only lacked IFNAR1, respectively (Figure 3A). Histopathology supported this finding, with increased GVHD found in the colon of mice lacking type I-IFN signaling in the hematopoietic compartment (Figure 3B-C). To further investigate differences in APC after transplantation, we isolated conventional dendritic cells (cDC) in B6.WT versus B6.IFNAR1−/− recipients and compared numbers and function. These studies indicated that although cDC numbers were not different in the spleen 24 hours after irradiation, cDCs unable to respond to type I-IFN were more efficient at stimulating allodisparate CD4+ T-cell proliferation and IFNγ production (Figure 3D). Combined, these data demonstrate that type I-IFN signaling in the hematopoietic system of BM transplantation recipients protects against CD4-dependent GVHD.
Type I-IFN signaling in the hematopoietic compartment of recipients of BM transplantation protects from GVHD. B6 chimeras were generated as described in “BM transplantation” and underwent transplantation 4 months later with 107 BM and 5 × 106 T cells from BALB/c.WT donors. (A) Serum cytokine levels were assessed at day 4 (IFNγ): *P < .05, B6 (WT→WT) vs B6 (IFNAR1−/−→IFNAR1−/−), n = 6 per group, combined from 2 experiments) or day 7 (TNF: *P < .05, B6 (WT→WT) vs B6 (IFNAR1−/−→WT) and B6 (IFNAR1−/−→IFNAR1−/−), n = 4-7 per group) after transplantation. (B) Semiquantitative colon histopathology at day 7 after BM transplantation (*P < .05, B6 (WT→WT) vs B6 (IFNAR1−/−→WT) and **P < .01, B6 (WT→WT) vs B6 (IFNAR1−/−→IFNAR1−/−), n = 4-7 per T cell–replete group). (C) Representative images are shown (× 250). (D) B6.WT or B6.IFNAR1−/− mice were lethally irradiated and 24 hours later, cDC enumerated, sorted, and cultured with BALB/c CD4+ T cells at 1:10 ratio for 5 days. Tissue culture supernatant was harvested (for IFNγ) and proliferation quantified by tritiated thymidine uptake during the final 18 hours. Representative plots from 2 duplicate experiments and displayed as mean ± SEM of triplicate wells.
Type I-IFN signaling in the hematopoietic compartment of recipients of BM transplantation protects from GVHD. B6 chimeras were generated as described in “BM transplantation” and underwent transplantation 4 months later with 107 BM and 5 × 106 T cells from BALB/c.WT donors. (A) Serum cytokine levels were assessed at day 4 (IFNγ): *P < .05, B6 (WT→WT) vs B6 (IFNAR1−/−→IFNAR1−/−), n = 6 per group, combined from 2 experiments) or day 7 (TNF: *P < .05, B6 (WT→WT) vs B6 (IFNAR1−/−→WT) and B6 (IFNAR1−/−→IFNAR1−/−), n = 4-7 per group) after transplantation. (B) Semiquantitative colon histopathology at day 7 after BM transplantation (*P < .05, B6 (WT→WT) vs B6 (IFNAR1−/−→WT) and **P < .01, B6 (WT→WT) vs B6 (IFNAR1−/−→IFNAR1−/−), n = 4-7 per T cell–replete group). (C) Representative images are shown (× 250). (D) B6.WT or B6.IFNAR1−/− mice were lethally irradiated and 24 hours later, cDC enumerated, sorted, and cultured with BALB/c CD4+ T cells at 1:10 ratio for 5 days. Tissue culture supernatant was harvested (for IFNγ) and proliferation quantified by tritiated thymidine uptake during the final 18 hours. Representative plots from 2 duplicate experiments and displayed as mean ± SEM of triplicate wells.
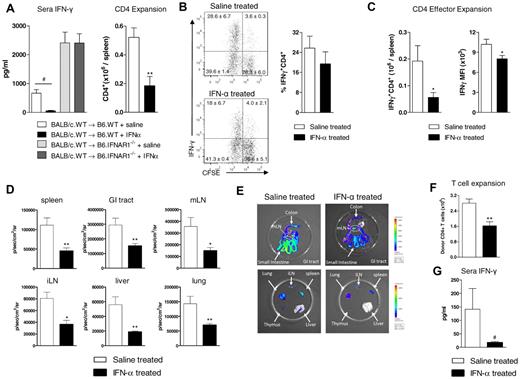
Treatment with IFN-α alleviates GVHD via a reduction in donor T-cell proliferation and differentiation
Because physiologic type I-IFN signaling attenuates donor T-cell function, we investigated whether this could be further suppressed by the administration of exogenous recombinant murine IFNα. We used the BALB/c→B6 model and treated recipients at day −1 so that regulatory effects were induced only in recipient tissue and the cytokine would be cleared before any potential inhibitory effects could be exerted directly on the donor graft. Treatment with IFN-α resulted in a significant suppression of IFN-γ levels in the sera and donor CD4+ T-cell expansion in the spleen (Figure 4A). To confirm that IFNα was only acting on host tissue, we included controls in which IFNα was also administered to IFNAR1−/− recipients and demonstrated no effect on IFNγ in the sera compared with saline-treated recipients (Figure 4A). When IFNγ production by CD4+ T cells was assessed, the percentage of CD4+ T cells producing IFNγ was not significantly different (Figure 4B). However, the absolute number of CD4+ T cells producing IFNγ in the spleen and the amount that they were producing as assessed by mean fluorescence intensity was significantly lower after IFNα treatment (Figure 4C).
Treatment with IFN-α before transplantation inhibits Th1 differentiation and protects from GVHD. Recipient B6.WT or B6.IFNAR1−/− mice received either IFN-α or saline immediately after total-body irradiation and were transplanted the following day with BM + T cells from BALB/c.CD45.1+ donors. (A) Serum cytokine levels of IFN-γ were assessed (pooled data from 2 experiments; #P < .005, saline vs IFN-α, n = 11, 11, 7, 7) and donor CD4+ T cells were enumerated in the spleen 4 days later (pooled data from 2 experiments; **P < .01, saline vs IFN-α; n = 6 per group). (B) IFN-γ production from CD4+ T cells stimulated ex vivo for 5 hours was determined by intracellular cytokine staining. Plots shown are representative of 3 experiments and displayed as mean ± SEM, n = 9 per group. (C) CD4+IFN-γ–producing cells were enumerated in the spleen and MFI determined. Plots shown are representative of 3 experiments and displayed as mean ± SEM, n = 9 per group. Lethally irradiated B6D2F1 recipients received B6.WT BM (107) + B6luc+ T cells (2 × 106). (D) Luminescence was quantified at day 7 after transplant (*P < .05, saline vs IFN-α treatment in mLN and iLN; **P < .01, saline vs IFN-α treatment in spleen, gastrointestinal tract, liver and lung, n = 5 per group). (E) Representative biophotonic images are shown as labeled. (F) Donor CD4+ T-cell expansion was quantified on day 4 (**P < .01, saline vs IFN-α treatment, n = 10 per group) and (G) serum IFN-γ analyzed at day 3 after transplantation (#P < .005, saline vs IFN-α, n = 10 per group).
Treatment with IFN-α before transplantation inhibits Th1 differentiation and protects from GVHD. Recipient B6.WT or B6.IFNAR1−/− mice received either IFN-α or saline immediately after total-body irradiation and were transplanted the following day with BM + T cells from BALB/c.CD45.1+ donors. (A) Serum cytokine levels of IFN-γ were assessed (pooled data from 2 experiments; #P < .005, saline vs IFN-α, n = 11, 11, 7, 7) and donor CD4+ T cells were enumerated in the spleen 4 days later (pooled data from 2 experiments; **P < .01, saline vs IFN-α; n = 6 per group). (B) IFN-γ production from CD4+ T cells stimulated ex vivo for 5 hours was determined by intracellular cytokine staining. Plots shown are representative of 3 experiments and displayed as mean ± SEM, n = 9 per group. (C) CD4+IFN-γ–producing cells were enumerated in the spleen and MFI determined. Plots shown are representative of 3 experiments and displayed as mean ± SEM, n = 9 per group. Lethally irradiated B6D2F1 recipients received B6.WT BM (107) + B6luc+ T cells (2 × 106). (D) Luminescence was quantified at day 7 after transplant (*P < .05, saline vs IFN-α treatment in mLN and iLN; **P < .01, saline vs IFN-α treatment in spleen, gastrointestinal tract, liver and lung, n = 5 per group). (E) Representative biophotonic images are shown as labeled. (F) Donor CD4+ T-cell expansion was quantified on day 4 (**P < .01, saline vs IFN-α treatment, n = 10 per group) and (G) serum IFN-γ analyzed at day 3 after transplantation (#P < .005, saline vs IFN-α, n = 10 per group).
Because it is possible that IFN-α may have simply enhanced graft rejection in this MHC disparate system, we repeated these studies in the B6→B6D2F1 model, a parental system in which recipients are also treated with NK1.1 to deplete NK cells and eliminate the possibility of graft rejection. We used luciferase-expressing transgenic donor T cells in these studies to monitor expansion after BM transplantation. As shown, the treatment of recipients with IFNα before BM transplantation significantly reduced donor T-cell expansion in lymphoid and GVHD target organs (Figure 4D-E). Donor CD4+ T-cell expansion in the spleen (Figure 4F) and systemic IFN-γ generation (Figure 4G) were again also suppressed. These results confirm that IFN-α signaling within host tissue during conditioning inhibits subsequent donor CD4+ T-cell priming.
Type I-IFN signaling differentially regulates CD4+ and CD8+ T-cell activation after MHC-matched BM transplantation
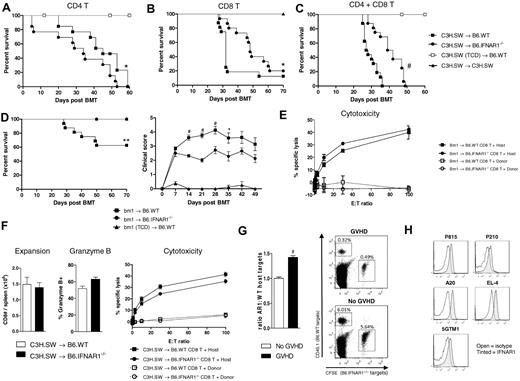
Having established an important role for type I-IFN in reducing donor T-cell responses after MHC-mismatched transplantation, we next investigated their role in BM transplantation systems that were MHC matched but where GVHD is induced to multiple minor HA mismatches and CD8+ T cells significantly contribute to pathology. Using the C3H.SW→B6 model we found that the presence of Type I-IFN signaling in the recipient again inhibited CD4-dependent GVHD (Figure 5A). However, when CD8+ T cells alone were transplanted, type I-IFN signaling within the host paradoxically resulted in accelerated GVHD (Figure 5B), and this effect dominated in this system when both CD4+ and CD8+ T cells were present (Figure 5C). To confirm this enhancement of CD8-dependent GVHD by type I-IFN signaling in the recipient, we undertook further transplantations in the bm1→B6 model where CD8-dependent GVHD is directed toward an isolated MHC class I mismatch. These results again demonstrated enhanced CD8-dependent GVHD in the presence of type I-IFN signaling within host tissue (Figure 5D).
Type I-IFN signaling differentially regulates CD4+ and CD8+ T-cell GVHD in a minor histocompatibility antigen-mismatched model of BM transplantation. Survival of lethally irradiated B6.WT or B6.IFNAR1−/− mice transplanted with 107 BM and either (A) 3 × 106 CD4+ T cells only (*P < .05, B6.IFNAR1−/− vs B6.WT recipients; n = 13 in BM + T, n = 6 in TCD controls), (B) 2 × 106 CD8+ T cells only (*P < .05, B6.IFNAR1−/− vs B6.WT recipients, n = 16 in BM + T, n = 4 in syngenic controls), or (C) CD3+ T cells containing 2 × 106 CD8+ T cells (#P < .005, B6.IFNAR1−/− vs B6.WT recipients, n = 16 in BM + T, n = 8 in TCD controls) from immunized C3HSW mice. (D) Clinical scores of lethally irradiated B6.WT or B6.IFNAR1−/− mice who underwent transplantation with 5 × 106 BM and 5 × 106 CD3+ T cells from bm1 donors (*P < .05, **P < .01, #P < .005, B6.IFNAR1−/− vs B6.WT recipients, n = 16 in BM + T, n = 8 in TCD controls, data combined from 2 experiments). (E) At day 12 after transplantation with CD3+ T cells in the bm1 → B6 system, CD8+ T cells were sort purified and used as effectors in chromium release assays against host type EL4 or donor bm1 blasts as targets. (F) At day 21 after transplantation with CD3+ T cells in the C3H.SW → B6 system, CD8+ T cells were enumerated (data combined from 2 experiments, mean ± SEM; n = 8 per group), stained for Granzyme B (mean ± SEM; n = 4 per group), or sort purified then used as effectors in chromium release assays against host type EL4 or donor C3H.SW blasts as targets (data combined from 2 experiments). (G) In vivo CTL function against B6.CD45.1+ and CFSE-labeled B6.IFNAR1−/− (CD45.2+) host targets at day 12 after transplantation in the C3H.SW → B6 system (GVHD recipients received BM and CD3+ T cells, and non-GVHD recipients received T cell–depleted BM only). The ratio of remaining B6.IFNAR1−/− to B6.CD45.1+ targets in spleen is shown with representative plots (#P = .005, no GVHD vs GVHD; data combined from 2 experiments, mean ± SEM; n = 7-10 per group). (H) IFNAR1 expression on the P815, P210, A20, EL4, and 5GTM1 tumor cell lines.
Type I-IFN signaling differentially regulates CD4+ and CD8+ T-cell GVHD in a minor histocompatibility antigen-mismatched model of BM transplantation. Survival of lethally irradiated B6.WT or B6.IFNAR1−/− mice transplanted with 107 BM and either (A) 3 × 106 CD4+ T cells only (*P < .05, B6.IFNAR1−/− vs B6.WT recipients; n = 13 in BM + T, n = 6 in TCD controls), (B) 2 × 106 CD8+ T cells only (*P < .05, B6.IFNAR1−/− vs B6.WT recipients, n = 16 in BM + T, n = 4 in syngenic controls), or (C) CD3+ T cells containing 2 × 106 CD8+ T cells (#P < .005, B6.IFNAR1−/− vs B6.WT recipients, n = 16 in BM + T, n = 8 in TCD controls) from immunized C3HSW mice. (D) Clinical scores of lethally irradiated B6.WT or B6.IFNAR1−/− mice who underwent transplantation with 5 × 106 BM and 5 × 106 CD3+ T cells from bm1 donors (*P < .05, **P < .01, #P < .005, B6.IFNAR1−/− vs B6.WT recipients, n = 16 in BM + T, n = 8 in TCD controls, data combined from 2 experiments). (E) At day 12 after transplantation with CD3+ T cells in the bm1 → B6 system, CD8+ T cells were sort purified and used as effectors in chromium release assays against host type EL4 or donor bm1 blasts as targets. (F) At day 21 after transplantation with CD3+ T cells in the C3H.SW → B6 system, CD8+ T cells were enumerated (data combined from 2 experiments, mean ± SEM; n = 8 per group), stained for Granzyme B (mean ± SEM; n = 4 per group), or sort purified then used as effectors in chromium release assays against host type EL4 or donor C3H.SW blasts as targets (data combined from 2 experiments). (G) In vivo CTL function against B6.CD45.1+ and CFSE-labeled B6.IFNAR1−/− (CD45.2+) host targets at day 12 after transplantation in the C3H.SW → B6 system (GVHD recipients received BM and CD3+ T cells, and non-GVHD recipients received T cell–depleted BM only). The ratio of remaining B6.IFNAR1−/− to B6.CD45.1+ targets in spleen is shown with representative plots (#P = .005, no GVHD vs GVHD; data combined from 2 experiments, mean ± SEM; n = 7-10 per group). (H) IFNAR1 expression on the P815, P210, A20, EL4, and 5GTM1 tumor cell lines.
To study the mechanism of this type I-IFN enhancement of CD8-dependent GVHD we investigated CD8+ T-cell function after transplantation when differential clinical scores became apparent (Figure 5D, data not shown for C3H.SW→B6 system). Surprisingly, donor CD8+ T-cell cytotoxicity was similar in the bm1→B6 system, regardless of whether the recipient was B6.WT or B6.IFNAR1−/− (Figure 5E). In the C3H.SW→B6 model, donor CD8+ T-cell numbers, Granzyme B expression and levels of cytotoxicity against host were also similar in B6.WT and B6.IFNAR1−/− recipients (Figure 5F). We therefore investigated the possibility that type I-IFN signaling in recipient tissue was rendering it more susceptible to donor CD8+ T-cell–mediated cytotoxicity, by studying the ability of alloreactive T cells to differentially kill WT and IFNAR1−/− targets in vivo. As shown in Figure 5G, this was indeed the case with host type IFNAR1−/− targets preferentially surviving relative to WT targets in the presence of an alloreactive T-cell response. This result was also confirmed in the bm1→B6 system where IFNAR1−/− targets were 2.26 times more resistant to cytolysis than WT targets (data not shown). Thus, type I-IFN signaling within recipient tissue enhances CD8-dependent GVHD independent of effects on the donor CD8+ T-cell effector response and instead increases the susceptibility of host target tissue to cytolytic damage. To determine whether type I-IFN signaling could also act directly on tumor to make it more susceptible to killing, we analyzed myeloid (P815, P210), T and B lymphoid (EL-4, A20), and plasma cell (5GTM1) tumor lines for IFNAR1 expression and found that this was indeed the case (Figure 5H). Therefore, treatment with type I-IFN could potentially result in increased susceptibility of tumor to CD8+ T cell–mediated killing.
Type I-IFN signaling in donor T cells enhances GVHD and GVL responses
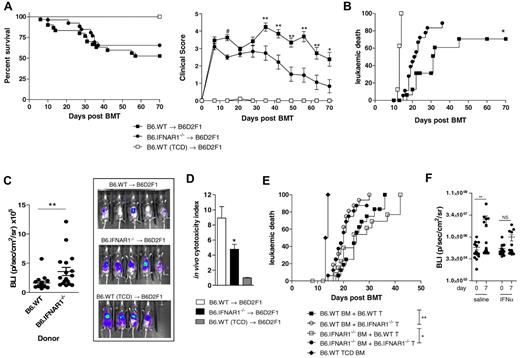
To investigate the role of type I-IFN signaling through donor cells, we used B6.WT or B6.IFNAR1−/− donors in the B6→B6D2F1 model of GVHD. These studies demonstrated that although survival was similar with either donor, there was a significant decrease in clinical scores in recipients of B6.IFNAR1−/− grafts after day 30 (Figure 6A). Before this, GVHD occurred with similar penetrance in both groups such that individual animals developed severe GVHD (clinical scores of 6 or greater). Because improving GVL responses is highly desirable after transplantation, we then went on to study the growth of host-derived luciferase-transfected P815 mastocytoma cells in this model. Recipients of B6.IFNAR1−/− grafts had reduced GVL compared with those who received B6.WT grafts, as demonstrated by survival and biophotonic imaging at day 12 (Figure 6B-C). In vivo cytotoxicity assays indicated that there was a significant reduction in the killing of host targets in recipients of B6.IFNAR1−/− grafts compared with B6.WT grafts, consistent with the decreased GVL in this group (Figure 6D).
GVHD and GVL responses are enhanced by type I-IFN signaling in donor grafts. (A) Survival and clinical scores in lethally irradiated B6D2F1 mice transplanted with 5 × 106 BM and 2 × 106 T cells from either B6.WT or B6.IFNAR1−/− donors (#P < .005, **P < .01, *P < .05; combined data from 3 experiments, n = 26-30 in BM + T groups, n = 13 in TCD controls). (B) Leukemic death after administration of host derived P815luc+ tumor (5 × 103) with the donor graft (*P < .05, B6.WT vs B6.IFNAR1−/− donors; combined data from 2 experiments, n = 18 in BM + T groups, n = 8 in TCD control groups). (C) Bioluminescence at day 12 after transplantation with P815luc+ tumor (**P < .01, B6.WT vs B6.IFNAR1−/− donors; combined data from 2 experiments, n = 18 per gp) with representative images shown. (D) In vivo cytotoxicity index at day 12 after BM transplantation (data combined from 2 experiments and expressed as mean ± SEM; *P < .05, B6.WT vs B6.IFNAR1−/− donors, n = 7-11 per group). (E) Leukemic death after transplantation of lethally irradiated B6D2F1 mice with a combination of either B6.WT or B6.IFNAR1−/− BM with B6.WT or B6.IFNAR1−/− T cells and P815luc+ tumor (**P < .01, *P < .05, combined data from 2 experiments, n = 16 in BM + T groups, n = 8 in TCD). (F) B6.WT recipients were lethally irradiated and 24 hours later 107 BM and 106 CD8+ T cells from C3H.SW donors transplanted with 2.5 × 104 EL-4luc+ tumor. After the establishment of low-level tumor as determined by bioluminescence, recombinant IFNα or saline was administered every other day and tumor burden assessed 1 week later (data combined from 2 experiments and expressed as mean ± SEM; **P < .01 saline day 0 vs day 7).
GVHD and GVL responses are enhanced by type I-IFN signaling in donor grafts. (A) Survival and clinical scores in lethally irradiated B6D2F1 mice transplanted with 5 × 106 BM and 2 × 106 T cells from either B6.WT or B6.IFNAR1−/− donors (#P < .005, **P < .01, *P < .05; combined data from 3 experiments, n = 26-30 in BM + T groups, n = 13 in TCD controls). (B) Leukemic death after administration of host derived P815luc+ tumor (5 × 103) with the donor graft (*P < .05, B6.WT vs B6.IFNAR1−/− donors; combined data from 2 experiments, n = 18 in BM + T groups, n = 8 in TCD control groups). (C) Bioluminescence at day 12 after transplantation with P815luc+ tumor (**P < .01, B6.WT vs B6.IFNAR1−/− donors; combined data from 2 experiments, n = 18 per gp) with representative images shown. (D) In vivo cytotoxicity index at day 12 after BM transplantation (data combined from 2 experiments and expressed as mean ± SEM; *P < .05, B6.WT vs B6.IFNAR1−/− donors, n = 7-11 per group). (E) Leukemic death after transplantation of lethally irradiated B6D2F1 mice with a combination of either B6.WT or B6.IFNAR1−/− BM with B6.WT or B6.IFNAR1−/− T cells and P815luc+ tumor (**P < .01, *P < .05, combined data from 2 experiments, n = 16 in BM + T groups, n = 8 in TCD). (F) B6.WT recipients were lethally irradiated and 24 hours later 107 BM and 106 CD8+ T cells from C3H.SW donors transplanted with 2.5 × 104 EL-4luc+ tumor. After the establishment of low-level tumor as determined by bioluminescence, recombinant IFNα or saline was administered every other day and tumor burden assessed 1 week later (data combined from 2 experiments and expressed as mean ± SEM; **P < .01 saline day 0 vs day 7).
Because the BM and T-cell compartments contribute to antigen presentation and subsequent killing of host tumor after BM transplantation, respectively, we next investigated which donor cell types type I-IFN was acting on to enhance GVL responses. We performed mixing experiments with combinations of either B6.WT or B6.IFNAR1−/− BM and B6.WT or B6.IFNAR1−/− T-cell grafts. This finding confirmed that type I-IFN signaling directly through the donor T cells was responsible for enhancing GVL responses (Figure 6E). Because type I-IFN signaling within CTL targets enhances sensitivity to killing whereas signaling within donor T cells concurrently enhances the CTL effector response, we investigated whether exogenous cytokine could suppress tumor growth after allogeneic BM transplantation. We used the C3H.SW→B6 system in the presence of luciferase expressing host-type EL-4 lymphoma. We administered recombinant murine IFNα every other day for 1 week once recipients displayed low levels of tumor burden detectable by bioluminesnce imaging, because administration of cytokine to animals with high levels of established tumor was ineffective (data not shown). Although lymphoma burden increased significantly in recipients of saline as expected, this did not occur in recipients receiving IFNα (Figure 6F). Thus, the administration of exogenous IFNα to recipients in early relapse after BM transplantation can modulate tumor growth.
Discussion
Although the protective role of type I-IFN's in viral infection has been well established, the effect of the cytokine on adaptive immunity and in particular, the control of alloimmunity is poorly understood. Recombinant IFN-α was routinely used to treat patients with chronic myeloid leukemia in the preimatinib era, resulting in cytogenetic responses thought primarily to relate to antiproliferative effects.17-19 The ability of the cytokine to modulate GVHD and GVL after allogeneic BM transplantation has been described primarily in anecdotal case series and although difficult to interpret, clear cases of disease control are evident.20-22 In this study, we have demonstrated that type I-IFN signaling plays an important role in both GVHD and GVL responses. Importantly, the effects of the cytokine are pleiotropic, with differential effects on immune outcomes mediated by donor CD4+ and CD8+ T cells. Our data suggest the effects on donor CD4+ T cells are likely mediated indirectly, putatively by recipient antigen presenting cells, whereas direct effects on donor T cells and their targets control the outcome in response to MHC class I–restricted cellular responses.
Although most cells can produce type I-IFN in response to viral infection, plasmacytoid DCs (pDCs) are typically a dominant source of this cytokine.23 The source of type I-IFN in the BM transplantation setting is unclear because type I-IFN levels in the serum were below those detectable by conventional assays such as ELISA and viral inhibition assays (data not shown). However, the clearly altered transplantation outcome in the absence of cytokine signaling demonstrates its importance after BM transplantation.
The effect of pDCs in controlling transplant outcome is somewhat controversial.24-26 After myeloablative conditioning, this APC subset is rapidly depleted and appears redundant for donor T-cell priming.25 The differentiation of donor pDCs is disrupted in the presence of GVHD, and immature BM-derived forms appear suppressive,26 although this has not been linked to type I-IFN secretion. pDCs express TLR7 and TLR9 that respond to single-stranded RNA and CpG-rich DNA, respectively.27 The administration of CpG to BM transplantation recipients from day 0 markedly accelerated GVHD in MHC disparate (and CD4-dominant) systems via signaling through TLR9 and effects on host APC and IFN-γ.28
Although this strategy would be expected to promote type I-IFN secretion, the acceleration of GVHD is opposite to the early protective effects observed in our studies, suggesting the effects of CpG are independent of type I-IFN. In these studies TLR8/9 agonists also increased GVHD, consistent with effects after TLR4 ligation, which can also initiate type I-IFN production by DCs and macrophages.29 Thus, the dominant signal inducing type I-IFN secretion within specific cell types is unknown and will require the development of more sensitive reagents to allow informative analysis.
We have demonstrated that type I-IFN signaling in BM transplantation recipients provides protection from CD4-dependent GVHD. Although it is possible that type I-IFN can enhance graft rejection, studies in a parent to F1 model, where conventional rejection is absent, demonstrated identical results to that seen in the BALB/c→B6 model. Therefore, type I-IFN signaling in BM transplantation recipients alters the capacity of host cells to invoke donor T-cell differentiation to alloantigen. The predilection of GVHD for the colon in the absence of type I-IFN signaling within recipient tissue was surprising. The studies in chimeric recipients clearly demonstrate this was because of an effect of signaling in hematopoietic cells rather than target epithelium. Recipient cells of hematopoietic origin are traditionally considered important as APC for initiating GVHD although the relative importance of specific host APC subsets in initiating GVHD is currently unknown. Analysis early after irradiation demonstrated that survival of recipient cDC was not different between B6.WT and B6.IFNAR1−/− recipients. However, residual cDC in B6.IFNAR1−/− recipients were more efficient at inducing proliferation and effector function in allodisparate CD4+ T cells.
Interestingly, type I-IFN signaling has been shown to inhibit osteopontin expression in DC, resulting in inhibition of IL-27 secretion and Th17-mediated inflammatory responses.30 The demonstrated contribution of IL-17A to GVHD in this model suggests that this regulatory axis in host DC may be contributing to the protection mediated by type I-IFN signaling. However, current paradigms, and the data presented here, suggest that Th1 rather than Th17 differentiation is the major pathway responsible for acute GVHD, and the suppression of the former is likely responsible for the majority of the effects seen by type I-IFN early after BM transplantation. Nevertheless, the ability of donor-derived IL-17A to play a pathogenic role in GVHD is consistent with data published by ourselves31 and others.32,33 In conjunction with demonstrated effects of type I-IFN signaling on DC, it has also been shown that signaling in macrophages results in a dampening of immune responses and the activation of macrophages by lipopolysaccharide in the presence of type I-IFN induces IL-10 production to amplify this regulatory effect.34 Thus, although the recipient hematopoietic-derived cell type signaled by type I-IFN to regulate GVHD remains to be determined, it is likely to be an APC.
In contrast to the suppression of CD4-dependent GVHD by type I-IFN signaling in recipient tissue, there was a paradoxical increase in CD8-mediated GVHD. Surprisingly, this was not associated with apparent changes in CD8+ T-cell function, as was seen with CD4+ T-cell responses. Conversely, type I-IFN signaling increased the susceptibility of host tissue to CTL damage. After the submission of our study, Li et al35 reported only a mild reduction in hepatic GVHD histopathology in the C3HSW→B6 model in the absence of type I IFN signaling in host. This likely reflects the mild and nonlethal nature of GVHD in this system in the absence of donor immunization, as was undertaken in our studies. Increased susceptibility of different immune cell subsets (CD4+ T cells, macrophages, splenic cells) to apoptosis has been described after type I-IFN signaling during infection with Listeria and Chlamydia.36-38 Interestingly, clinical data from the 1990s also demonstrated a detrimental effect of type I-IFN administration in the pretransplantation period, with increases in severe GVHD and transplant-related mortality.39,40 This finding is consistent with CD8-dominant GVHD in clinical BM transplantation, where donor and recipients are matched at HLA loci. Type I-IFN has also been shown to promote apoptosis in several tumor cell lines in vitro, including multiple myeloma and acute lymphoblastic leukemia.41-43 Together with the in vivo data presented here, this provides a rationale for studying the expression of the type I-IFN receptor on primary human hematopoietic malignancies. In receptor-positive malignancies, the administration of type I-IFN after BM transplantation may augment the sensitivity of residual malignancy to GVL responses and may be worthy of study in patients at very high risk or relapse (eg, myeloma, primary refractory acute myeloid leukemia).
With this in mind we also dissected the effect of type I-IFN signaling on the donor graft after BM transplantation. These studies confirmed that the cytokine enhanced CTL activity and consequent GVL via a direct effect on donor T cells. Although these results are inconsistent with a recent study in which the authors used skin allograft models that indicated that type I-IFN signaling does not contribute to CD8+ T-cell–mediated rejection,44 the authors of other studies have clearly demonstrated a vital role for type I-IFN in the expansion and differentiation of effector CTL and in bystander activation.45,46 Furthermore, in studies in both patients and experimental models in which tolerance has been achieved investigators have demonstrated that type I-IFN signaling after either viral infection or endogenous administration can initiate rejection.47,48 Conversely, type I-IFN blockage in conjunction with immunosuppression can prolong allograft survival.49
Therefore, although the role of type I-IFN after solid-organ transplantation still remains controversial, a majority of studies suggest that signaling enhances alloreactive responses. Increased levels of type I-IFN have also been demonstrated to increase cross presentation to CD8+ T cells by APC independently of CD4+ T-cell help.50 Although type I-IFN signaling in donor APCs does not appear to contribute to GVL in our system, we investigated this using donors who cannot respond to type I-IFN and therefore comparing physiologic levels of signaling to its absence. In contrast, Le Bon et al induced high levels of type I-IFN, via both viral infection (lymphocytic choriomeningitis virus) and direct IFNα administration, which improved cross priming.50 In conjunction with demonstrating a clear role for physiologic type I-IFN signaling in CTL activity, we have also confirmed that administration of recombinant IFNα can modulate tumor growth after allogeneic BM transplantation. Donor NK-cell responses are also important for GVL responses and importantly, early NK tumor responses are dependent on type I-IFN signaling.12 Therefore, enhancement of these responses in conjunction with CD8+ T-cell responses would further improve GVL in BM transplanation recipients with NK-sensitive malignancies.
Although we have demonstrated potential for both prevention of GVHD and improvement of GVL by treatment with type I-IFN, the most effective therapeutic use of this cytokine would likely be as an adjunct treatment for patients at very high risk of relapse after BM transplantation, while tumor burdens are low. If given before transplantation, there is the risk of rendering recipient tissue more susceptible to donor cytolytic damage and perhaps that induced by chemoradiotherapy. In contrast, the ability of type I-IFN to make residual malignancy more susceptible to killing while enhancing cellular cytotoxicity makes this an attractive strategy to promote GVL in high-risk settings. The availability of new pegylated forms of the cytokine in clinical practice suggests this approach could be revisited in a controlled and prospective fashion.
An Inside Blood analysis of this article appears at the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Robert Negrin and Remi Creusot for the luciferase transgenic mice and Yoichiro Iwakura for the BALB/c.IL-17A−/− mice.
This work was supported by grants from the Cancer Council Queensland, LFQ and the NH&MRC.
Authorship
Contribution: R.J.R. designed and performed experiments and wrote manuscript; E.K., R.D.K., Y.A.W., S.D.O., A.L.J.D., N.C.R., K.E.L., A.V., K.A.M., and M.K. performed experiments; N.A.D.W provided vital reagents; A.D.C. performed all blinded histologic analysis; P.J.H. provided vital reagents and helped design experiments; K.P.A.M. designed studies and helped write manuscript; and G.R.H. designed studies and helped write the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Geoffrey Hill, Bone Marrow Transplantation Laboratory, Queensland Institute of Medical Research, 300 Herston Road, Herston, QLD, 4006 Australia; e-mail: geoff.hill@qimr.edu.au.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal