Identification of the specific roles of individual members of the hypoxia-inducible factor (HIF) family of transcriptional activators provides insights into the pathogenesis of anemia and erythrocytosis that may enable the development of novel therapies for these disorders. In this issue of Blood, Kapitsinou and colleagues1 use conditional ablation of Hif-2α in the murine kidney to establish that hypoxic induction of erythropoietin (Epo) is completely dependent on Hif-2α and that in the absence of renal Hif-2, hepatic Hif-2 becomes the main regulator of serum Epo.
Toward the end of the 19th century, 3 Frenchmen—Paul Bert, Denis Jourdanet, and Francois-Gilbert Viault—established the relationship between reduced oxygen pressure and increased circulating red blood cells (RBCs) based on their work on altitude in Mexico and the Peruvian Andes.2 Interest in understanding the physiologic and molecular basis of this adaptation to hypoxia led to the discovery of EPO and the HIF family of transcriptional activators.
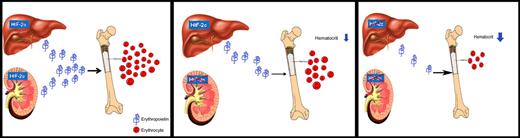
Erythropoietin (Epo) regulates red cell production in response to tissue oxygenation. Hypoxia, the main physiological stimulus of enhanced Epo gene transcription, can induce several 100-fold increases in circulating serum Epo levels mediated by hypoxia-inducible factor (Hif). Kapitsinou and colleagues ablated Hif-2α in the kidney and partially in the liver. They found that hypoxic induction of Epo is completely Hif-2–dependent and that in the absence of renal Hif-2, hepatic Hif-2 takes over as the main regulator of the serum Epo response to hypoxia. Their report corroborates recent genetic studies in mice and investigations of patients with familial erythrocytosis which have provided strong evidence that HIF-2α, not HIF-1α, is the prevalent regulator of circulating Epo levels. The image provided is a composite of the liver, kidney, and bone and RBC images as follows: liver image,11 kidney image,12 and bone and RBC image.13
Erythropoietin (Epo) regulates red cell production in response to tissue oxygenation. Hypoxia, the main physiological stimulus of enhanced Epo gene transcription, can induce several 100-fold increases in circulating serum Epo levels mediated by hypoxia-inducible factor (Hif). Kapitsinou and colleagues ablated Hif-2α in the kidney and partially in the liver. They found that hypoxic induction of Epo is completely Hif-2–dependent and that in the absence of renal Hif-2, hepatic Hif-2 takes over as the main regulator of the serum Epo response to hypoxia. Their report corroborates recent genetic studies in mice and investigations of patients with familial erythrocytosis which have provided strong evidence that HIF-2α, not HIF-1α, is the prevalent regulator of circulating Epo levels. The image provided is a composite of the liver, kidney, and bone and RBC images as follows: liver image,11 kidney image,12 and bone and RBC image.13
During human fetal development EPO is produced mainly in the liver but its primary site of production changes to the kidney during late gestation. Although the adult liver does not normally produce EPO under normoxic conditions, it retains the capacity to produce EPO in the event of renal impairment.
In the 1990s, in vitro studies by Gregg Semenza and colleagues identified a novel transcription factor, HIF-1, which was widely assumed to be responsible for the hypoxia-induced increase in EPO found in Hep3B cells, based on its binding to an 18-nucleotide fragment of the oxygen-sensitive 3′ EPO regulatory element.3,4 However, recent genetic studies in mice5-7 and investigations of patients with familial erythrocytosis8-10 have provided strong evidence that HIF-2α, not HIF-1α, is the prevalent regulator of circulating EPO levels.
In an elegant study, Kapitsinou and colleagues inactivate Hif-2α specifically in the kidney by Cre-loxP recombination enabling the contribution of renal Hif-2 signaling to Epo homeostasis to be determined directly (see figure). Loss of renal Hif-2α resulted in hypoproliferative anemia with RBCs and hematocrit (HCT) reduced to half of the normal levels, due to significantly lower circulating serum Epo levels in the mutant mice. The mutant mice also had increased levels of renal Hif-1α protein and increased expression of the Hif target genes Glut1, Pkf, Ldha, and Phd3, but not Epo production, providing further evidence that hypoxic regulation of Epo in the kidney is not dependent on Hif-1α.
To investigate the role of hepatocyte-derived Hif-2, the authors generated double mutants lacking or substantially reducing Hif-2α in the kidney and liver (see figure). These animals had significantly reduced serum Epo levels compared with their renal Hif-2–deficient, single mutant littermates indicating that hepatic Hif-2 plays a role in Epo regulation of the single mutants under baseline conditions. When further challenged by phlebotomy the double mutants had a 70% reduction in serum Epo levels compared with their single mutant counterparts. This suggests that in this scenario, at least 70% of serum Epo is produced via hepatocyte Hif-2 signaling, taking into account that Hif-2 is not produced in all of the hepatocytes due to limitations in recombination efficiency.
Hypothesizing that Hif-2 may coordinate Epo production with iron metabolism, the authors generated 2 different models of Hif activation based on cell-type–specific von Hippel-Lindau protein (pVHL) inactivation in hepatocytes, and on stabilization of systemic hypoxia in all liver cells. The experimental data provide convincing evidence that Hif-2 is involved in the transcriptional regulation of several genes implicated in iron metabolism, such as Dmt1, ceruloplasmin, and hephaestin, but its contribution to the coordination of Epo synthesis with iron homeostasis requires further investigation.
Although the present work confirms that Hif-2 responds to the body's demand for oxygen and is the predominant regulator of the erythropoiesis, its role in the supply of iron vis-à-vis Hif-1 remains to be established. As Kapitsinou et al indicate, stabilization of human HIF has the potential to stimulate latent hepatic human EPO synthesis in patients with renal impairment, through prolyl-4-hydroxylase domain (PHD) inhibition with 2-oxoglutarate analogs. Because inhibition of PHD causes stimulation of multiple HIF-regulated biologic processes, a superior strategy would entail the design of a drug that preferentially enhances HIF-2 activity, but such an approach is likely to be extremely challenging.
Conflict-of-interest disclosure: The author declares no competing financial interests. ■