Abstract
Abstract 2305
Poster Board II-282
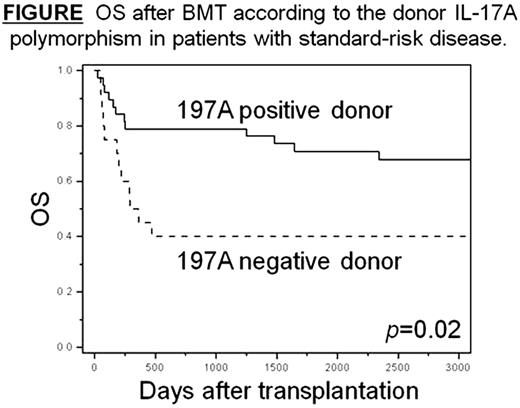
IL-17 plays an active role in autoimmune diseases and organ transplant rejection through its mediating proinflammatory responses and inducing inflammatory cytokine and chemokine production. This study examined the impact of donor and recipient polymorphism in the IL-17A gene on the clinical outcomes in unrelated HLA-fully-matched myeloablative bone marrow transplantation (BMT) through the Japan Marrow Donor Program. The IL-17A polymorphism (rs2275913, G197A) was retrospectively analyzed in a total 145 recipients with hematologic malignancies and their unrelated donors. In patients with standard risk disease, the donor IL-17A-197A genotype was associated with significantly improved OS (adjusted HR, 0.32; 95% CI, 0.13-0.79; p=0.01) and reduced transplant related mortality (TRM) (adjusted HR, 0.27; 95% CI, 0.11-0.67; p=0.005), but no impact on disease relapse or the development of grades II-IV acute GVHD or chronic GVHD. Patients with standard risk disease receiving transplants from donors with the 197A genotype had better 5-year OS (71% vs. 40%, p=0.02; Figure) and lower 5-year TRM rate (27% vs. 60%, p=0.02). The IL-17A polymorphism did not significantly influence the transplant outcomes in patients with high risk disease. These results suggest transplantation from IL-17A-197A positive donor is advantageous in improving OS and reducing TRM after HLA-matched unrelated BMT for standard risk hematologic malignancies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal