Abstract
In contrast to that in children, pharmacokinetic, pharmacodynamic, and safety information on pegaspargase in adults is very limited. We administered a single intravenous dose of pegaspargase (2000 IU/m2) as part of a standard frontline induction regimen to 25 adults with newly diagnosed acute lymphoblastic leukemia (ALL), and obtained serum samples on several time points. The population mean peak serum concentration of asparaginase enzymatic activity was 1 IU/mL, the elimination half-life was 7 days, and the volume of distribution was 2.43 L/m2. After the single dose, asparagine deamination was complete in all patients after 2 hours, and in 100%, 81%, and 44% on days 14, 21, and 28, respectively. A pharmocodynamic correlation model showed minimal enzymatic activity of 0.2 IU/mL for optimal asparagine depletion. The kinetic posthoc analyses demonstrated enzymatic activity for 3 weeks or more. One patient developed neutralizing antiasparaginase antibodies on day 22 after administration. Pegaspargase was well tolerated, with few grade 3/4 side effects. No allergic reactions or pancreatitis were observed. In adults aged 55 years or younger, pegaspargase produces a long duration of asparagine depletion and can be given intravenously, with a safety profile that is similar to equivalent multiple doses of intramuscular Escherichia coli asparaginase.
Introduction
L-asparaginase (asparaginase), a bacterial enzyme that depletes serum asparagine, is a standard component in most treatment protocols for acute lymphoblastic leukemia (ALL),1,2 both in children3-8 and in adults.9-14 ALL cells are unable to produce asparagine, and are dependent on plasma levels of this amino acid for protein synthesis.15,16 Plasma asparagine depletion results in inhibition of protein synthesis, which leads to inhibition of RNA and DNA synthesis with a subsequent apoptotic cell death of the leukemic cells.1,2,17 The most commonly used form of asparaginase is the native (unmodified) enzyme derived from Escherichia coli.2 Inclusion of asparaginase in the induction regimen in pediatric ALL has improved complete remission (CR) rates.3 Further, in nonrandomized2 and randomized6,18-22 studies, dose intensification of asparaginase during consolidation in combination with other chemotherapeutic agents has resulted in superior long-term survival of newly diagnosed children with ALL
A major limitation of E coli asparaginase is development of hypersensitivity, reported in 15% to 73% of both adults and children.2,23-26 It has been suggested that allergies and other side effects from E coli asparaginase were more frequent and severe in adults than in children.25,27 Hypersensitivity is associated with the production of antibodies to this drug,25,27,28 which often also develop without clinical manifestation of hypersensitivity—so-called “silent” hypersensitivity.2,29-31 These antibodies can reduce plasma asparaginase activity, leading to a rebound of plasma asparagine and the possible development of drug resistance.2,30,32-34 In a recent pediatric study, 60% of patients with newly diagnosed ALL eventually became antibody (Ab) positive.34
Pegaspargase (Oncaspar) is a modified form of native E coli asparaginase in which the enzyme is covalently linked to polyethylene glycol. The binding preserves the enzymatic function of the drug, but decreases the immunogenicity of the protein, thus potentially reducing the risk of hypersensitivity reactions.1,2,35-38 Pegaspargase can be given safely to children with a history of allergic reaction to prior administration of E coli asparaginase,2,39,40 and is indicated for patients who require asparaginase but have developed hypersensitivity to the native form or as part of front-line treatment of ALL.41 Another advantage of pegaspargase is its prolonged half-life of elimination compared with the E coli or Erwinia forms, which may be important in improving the pharmacokinetic profile of the drug.32 In addition, a single injection of pegaspargase can be given instead of the inconvenient administration of multiple doses of native asparaginase. Pegaspargase has shown antileukemic activity similar to that of E coli asparaginase in children with recurring ALL39,42-44 who have already been exposed to the native form, as well as in newly diagnosed patients.19,35 In contrast to children, pharmacokinetic and toxicity data on pegaspargase in adults is very limited.45 We herein report, in adults, the results of Ab formation, as well as the pharmacokinetics, pharmacodynamics, and toxicity of pegaspargase when given intravenously to asparaginase-naive patients with ALL. For purpose of this study, the drug was given as a single intravenous dose, and was combined with a standard (vincristine, daunorubicin, and prednisone) frontline induction regimen in newly diagnosed adults with ALL. We also determined the rate of CR after receipt of a regimen that contained pegaspargase in newly diagnosed adults with ALL.
Patients, materials, and methods
Patients
Newly diagnosed adults with ALL, aged 17 to 55 years who were treated at the University of Southern California (USC) Hospitals (including Los Angeles County–USC Medical Center and USC/Norris Comprehensive Cancer Center) between 1995 and 1999 were enrolled into this study and treated by the same team of hematologists. The diagnosis of ALL was based on blasts in the bone marrow that were myeloperoxidase negative and TdT positive and/or expressed an ALL immunophenotype with monoclonal antibodies directed against precursor B-cell or T-cell lineage. Patients with ALL FAB L3 and blastic crisis of chronic myelogenous leukemia as well as HIV-positive patients were excluded. Bilirubin levels had to be lower than 34.2 μM (2 mg/dL), and creatinine levels had to be lower than 176.8 μM (2 mg/dL). The protocol was approved by the USC Institutional Review Board, and all patients signed an informed consent document, in accordance with the Declaration of Helsinki, prior to study entry.
Treatment protocol
We used the adult ALL BFM protocol as reported by Hoelzer et al,11 which was modified by administering a single dose of pegaspargase at a dose of 2000 IU/m2 intravenously on day 16 instead of the 14 injections of E coli asparaginase as used in the original BFM protocol. The dose of pegaspargase was reduced from the approved dose of 2500 IU/m2 because of concerns of higher relative bioavailability after intravenous dosing and possibly greater toxicity in adults. The dose was not capped at 3750 IU, which is the content of a single vial of the drug. Pegaspargase was diluted in 100 mL of 0.9% of NaCl and given intravenously over 2 hours. The regimen also included 60 mg/m2 daunorubicin per day intravenously on days 1, 2, and 3; 1.4 mg/m2 vincristine per dose intravenously on days 1, 8, 15, and 22 (maximum dose, 2.0 mg); and 60 mg/m2 oral prednisone per day on days 1 to 28, with tapering over 2 weeks. Similar to the original BFM protocol, all patients, whether or not they had achieved a CR, were given a second induction phase that included 650 mg/m2 cyclophosphamide per dose intravenously on days 1, 15, and 28; 75 mg/m2 cytosine arabinoside per dose intravenously on days 1 to 4, 8 to 11, 16 to 19, and 21 to 25; 60 mg/m2 oral 6-mercaptopurine (MP) per day on days 1 to 28; and intrathecal (IT) methotrexate on days 1, 8, 15, and 22. Patients who achieved CR continued with consolidation and maintenance therapy as in the original BFM protocol.11 Granulocyte colony-stimulating factor (G-CSF) was not routinely used, except for severe infections during neutropenia at the discretion of the physician only.
A lumbar puncture was done at diagnosis only if central nervous system (CNS) involvement was clinically suspected. Blood for laboratory testing was obtained every 3 to 4 days and included complete blood counts, glucose, bilirubin, liver enzymes, creatinine, electrolytes, fibrinogen and antithrombin III, samples for phramcokinetic studies, and antiasparaginase antibodies.
We used in this cohort of adult patients with ALL the commercial pegaspargase formulation produced by Enzon Pharmaceuticals (Bridgewater, NJ) and licensed for marketing by Rhone-Poulenc Rorer (Collegeville, PA) that was available until 1999. At that time, the drug was temporarily removed from the market because “visible particulate matter” was discovered in 2 vials; thus, we were forced to close the study. In 2003, the manufacturing problems were resolved by Enzon, and the drug is directly marketed by this company under the same name.
Toxicity
The toxicity of the single intravenous dose of pegaspargase was graded according to the National Cancer Institute Common Toxicity Criteria version 3.
Pegaspargase pharmacokinetics: NONMEM population model
A population pharmacokinetic (PPK) model using the nonlinear mixed effects model (NONMEM; Globomax, Hanover, MD) program was developed that closely fit the measured enzyme activity and asparagine concentrations. A population model for a 1-compartment open model using the NONMEM computer program was designed as described.35 The Michaelis-Menten equation was programmed into a separate subroutine of this program, so that the serum asparaginase enzymatic activity and its substrate asparagine could be modeled simultaneously. Serum pegaspargase activity and asparagine values during induction were analyzed with a combined population pharmacokinetic pharmacodynamic (PD) model using the Michaelis-Menten equation in the NONMEM program. Steady-state asparagine concentration was estimated to be 50 μM. These classical PPK analyses were performed, and the results were compared with the results from the NONMEM analyses for pegaspargase in pediatric patients.35
Pegaspargase enzymatic assay
Pegaspargase enzymatic activity was determined in a total of 25 patients, including 18 patients in whom 5 to 6 serum specimens were available per patient at various time points over 28 days of therapy, in an additional 3 patients with 3 sera specimens after drug treatment, and in an additional 4 patients who had only 2 sera specimens available for analysis. Pegaspargase enzymatic activity was measured by 2 different assays. One assay is based on the determination of ammonia (NH3) produced from l-asparagine amino acid, and is a modification of the assay previously reported.32,35 The assay procedure is based on the nesslerization of ammonia. l-aspartic acid, the deaminated amino acid, can also be used to determine the progress of the enzymatic reaction, an assay which requires high-performance liquid chromatography (HPLC) reverse-phase capability.35 The second assay used has previously been reported.34,35 This assay couples the formation of L-aspartate that results from the hydrolysis of asparagine by asparaginase with the production of oxaloacetate and l-glutamate via the enzymatic action of oxaloacetic transaminase. The enzyme malic dehydrogenase uses oxaloacetate to oxidize NADH, the oxidation of which is measured spectrophotometrically at 340 nm by the Dynatech spectrophotometer (Dynatech Laboratories, Chantilly, VA). Both enzymatic assays show excellent linearity.
Development of the antiasparaginase Ab ELISA assays for native E coli asparaginase and pegaspargase
We developed enzyme-linked immunosorbent assay (ELISA) equipment (Dynatech Laboratories) to allow a computer-controlled assay procedure. The Ab against E coli asparaginase was used initially to titrate human patients' sera who were hypersensitive to either E coli asparaginase or pegaspargase. The sera from patients hypersensitive to pegaspargase were used as the source of the antiasparaginase Ab for the ELISAs. The pegaspargase Ab assay in human sera is performed by a modified indirect solid-phase ELISA methodology previously reported.32,34,35 The assays exhibit excellent linearity and low detection limits. The Ab titers were compared with the same patient's negative control serum. Thus, the ratios of Ab titers over the negative control have the same denominator.
Pegaspargase levels
Pegaspargase protein was measured by an ELISA similar to the 1 for the antiasparaginase Ab.35 The main difference is that the ELISA plates are loaded with the antiasparaginase Ab instead of the antigen as in the Ab assay. This assay was used primarily to determine the possible Ab-induced neutralization of the pegaspargase enzymatic activity.
HPLC assay for asparagine
The asparagine concentration in the serum was measured using a reported HPLC assay modified for our specific needs.35 Amino acids were derivatized with phenylisothiocyanate (PITC) to form stable amino acid derivatives. The derivatized samples were analyzed on μC18 columns by a 2-step gradient elution. Calibration curves for asparagine were used to quantitate amino acids in the serum.
Response criteria
Patients were considered to be in CR when bone marrow cellularity was greater than 20% with maturation of all cell lines and less than 5% blasts, granulocyte count was greater than 1.5 × 109/L, platelet count was greater than 100 × 109/L, leukemic blasts were absent from the peripheral blood, and any detectable extramedullary leukemia had resolved. Isolated and stable splenomegaly was not considered extramedullary disease.
Results
Patient characteristics
A group of 25 patients were entered; their characteristics at diagnosis are listed in Table 1. A high proportion of patients (80%) were of Latino origin. The median white blood cell count at diagnosis was 10.3 × 109/L (range, 1.1-389.2 × 109/L). Of these, 21 patients presented with precursor B-cell ALL, 3 presented with T-cell ALL, and in 1 patient the phenotype was not established. Cytogenetic information was not available. No patient had CNS involvement at the time of diagnosis.
Patient characteristics
| Characteristic . | Value . |
|---|---|
| Median age, y (range) | 27 (17-55) |
| Immunophenotype,* no. of patients | |
| Precursor B-cell | 21 |
| T-cell | 3 |
| Median WBC at diagnosis, × 109/L (range) | 10.3 (1.1-389.0) |
| Female sex, no. of patients (%) | 9 (36) |
| Race, no. of patients | |
| Latino | 20 |
| White | 2 |
| Asian | 3 |
| Characteristic . | Value . |
|---|---|
| Median age, y (range) | 27 (17-55) |
| Immunophenotype,* no. of patients | |
| Precursor B-cell | 21 |
| T-cell | 3 |
| Median WBC at diagnosis, × 109/L (range) | 10.3 (1.1-389.0) |
| Female sex, no. of patients (%) | 9 (36) |
| Race, no. of patients | |
| Latino | 20 |
| White | 2 |
| Asian | 3 |
Phenotype was not determined in 1 patient.
Pegaspargase pharmacokinetic and PD studies
Pegaspargase was administered as a single intravenous dose of 2000 IU/m2 on day 16 of induction. There was no apparent difference between pegaspargase protein (antigen) and asparaginase enzymatic activity, except in 1 patient who developed antiasparaginase antibodies on day 22 after administration. In this patient, the day-28 specimen had the expected pegaspargase protein but lacked the reciprocal enzymatic asparaginase activity due to Ab neutralization. Hence, the asparaginase enzymatic activity set of data were used for PPK analyses.
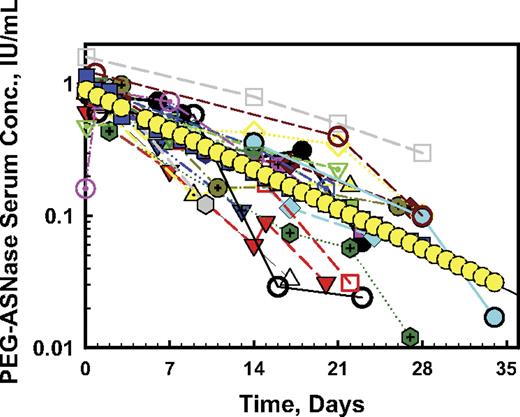
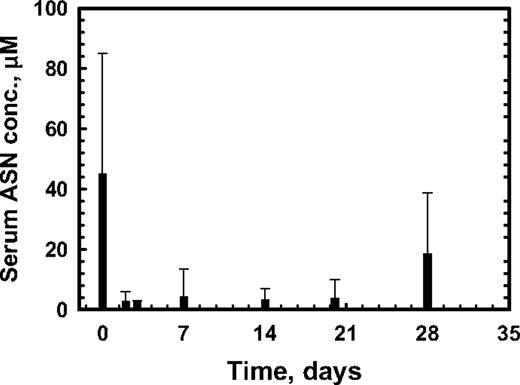
The serum concentrations of asparaginase activity in 23 patients who had at least 2 serum specimens after drug administration is shown in Figure 1. Significant intrapatient variability existed in the serum pegaspargase activity over time in these patients. The drug followed a 1-compartment open model analyzed by the NONMEM population program described elsewhere.35,46 The population posthoc (best fit) analysis (yellow symbols in Figure 1) showed an average peak serum concentration of enzymatic activity in the adult ALL population of 1 IU/mL, an elimination half-life of 7 days (95% confidence interval [CI] = 6.04-7.90), and a volume of distribution of 2.43 L/m2 equivalent to plasma volume. The mean serum asparaginase enzymatic activity in patients who had at least 4 samples was 0.997 ± 0.44 IU/mL (mean ± SD), 0.601 ± 0.39 IU/mL, 0.471 ± 0.35 IU/mL, 0.195 ± 0.186 IU/mL, and 0.052 ± 0.075 IU/mL on days 2, 7, 14, 20, and 28, respectively (Figure 2).
NONMEM posthoc model of serum asparaginase enzymatic activity. The data are from 23 adult patients who had 2 or more serum specimens after a single intravenous dose (2000 IU/m2) of pegaspargase. Each color indicates an individual patient, showing the variability between patients. Several patients had enzymatic activity of 0.2 IU/mL or greater on day 28. The NONMEM posthoc (best fit) model is shown in yellow circles demonstrating T1/2 = 7 days (95% CI, 6.04-7.90) and volume of distribution = 2.43 L/m2, which is equal to plasma volume in adults.
NONMEM posthoc model of serum asparaginase enzymatic activity. The data are from 23 adult patients who had 2 or more serum specimens after a single intravenous dose (2000 IU/m2) of pegaspargase. Each color indicates an individual patient, showing the variability between patients. Several patients had enzymatic activity of 0.2 IU/mL or greater on day 28. The NONMEM posthoc (best fit) model is shown in yellow circles demonstrating T1/2 = 7 days (95% CI, 6.04-7.90) and volume of distribution = 2.43 L/m2, which is equal to plasma volume in adults.
Serum asparaginase enzymatic activity. The results are from 19 patients who had 4 or more serum specimens after a single intravenous dose (2000 IU/m2) of pegaspargase over a period of 28 days. The results are depicted as the mean ± SD activity at the nearest time point to 7, 14, 21, and 28 days, respectively, after a single intravenous dose (2000/ IU/m2) of pegaspargase.
Serum asparaginase enzymatic activity. The results are from 19 patients who had 4 or more serum specimens after a single intravenous dose (2000 IU/m2) of pegaspargase over a period of 28 days. The results are depicted as the mean ± SD activity at the nearest time point to 7, 14, 21, and 28 days, respectively, after a single intravenous dose (2000/ IU/m2) of pegaspargase.
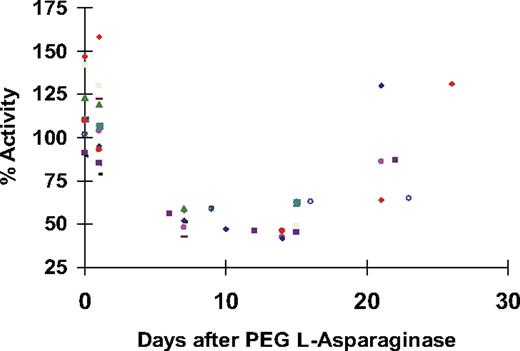
The mean serum asparagine concentrations remained markedly lower than baseline (prior to drug administration) up to day 21 and still significantly lower on day 28 (Figure 3). Deamination of asparagine was complete in all patients by 2 hours after administration and on day 14, in 81% on day 21, and in 44% on day 28 after drug administration (Table 2). Furthermore, the population average pegaspargase enzymatic activity levels correlated with the serum asparagine deamination, expressed as a percentage of pretreatment control yielding the upper portion of a sigmoid curve per Michaelis-Menten relationship (Figure 4). This PD correlation between the serum deamination and asparaginase activity showed that a minimal enzymatic activity of 0.2 IU/mL was needed for optimal asparagine deamination of 90% compared with the baseline. As seen in Figure 1, several patients had enzymatic activity of 0.2 IU/mL or greater even up to day 28 after drug administration.
Serum asparagine concentrations representing asparagine deamination. The results are from 19 patients who had 4 or more serum specimens after a single intravenous dose (2000 IU/m2) of pegaspargase. The results are expressed as the mean ± SD. ASN indicates asparagine.
Serum asparagine concentrations representing asparagine deamination. The results are from 19 patients who had 4 or more serum specimens after a single intravenous dose (2000 IU/m2) of pegaspargase. The results are expressed as the mean ± SD. ASN indicates asparagine.
Serum asparagine deamination (depletion) at different time intervals after drug administration
| Time . | No. of patients tested . | Asparagine deamination, no. of patients (%) . |
|---|---|---|
| 2 h | 14 | 14 (100) |
| Day 7 | 16 | 16 (100) |
| Day 14 | 12 | 12 (100) |
| Days 20-21 | 11 | 9 (82) |
| Days 26-28 | 9 | 4 (44) |
| Time . | No. of patients tested . | Asparagine deamination, no. of patients (%) . |
|---|---|---|
| 2 h | 14 | 14 (100) |
| Day 7 | 16 | 16 (100) |
| Day 14 | 12 | 12 (100) |
| Days 20-21 | 11 | 9 (82) |
| Days 26-28 | 9 | 4 (44) |
Samples were obtained from 19 adult patients after a single IV dose (2000/IU/m2) of pegaspargase. Serum asparagine concentration of less than 3 μM is considered optimal deamination.44
The relationship between asparaginase enzymatic activity of the pegaspargase and its substrate (asparagine). The results are shown as a sigmoid pharmacodynamic relationship between the population mean of deaminated asparagine levels expressed as a percentage of pretreatment controls versus log10 of asparaginase enzymatic activity. The sigmoid relationship is of the third order of regression, as it is the upper portion of the sigmoid fit according to the Michelis-Menten reaction. Of note is that the time does not appear in the figure since it is embedded in the PPK of asparaginase enzymatic activity, which was obtained from Figure 2. Minimal enzymatic activity of 0.2 IU/mL was needed for optimal asparagine deamination of 90% compared with the baseline. Horizontal line indicates 90% of asparagine depletion below pretreatment levels; vertical line, 0.2 IU/mL of asparaginase activity; and ASN, asparagine.
The relationship between asparaginase enzymatic activity of the pegaspargase and its substrate (asparagine). The results are shown as a sigmoid pharmacodynamic relationship between the population mean of deaminated asparagine levels expressed as a percentage of pretreatment controls versus log10 of asparaginase enzymatic activity. The sigmoid relationship is of the third order of regression, as it is the upper portion of the sigmoid fit according to the Michelis-Menten reaction. Of note is that the time does not appear in the figure since it is embedded in the PPK of asparaginase enzymatic activity, which was obtained from Figure 2. Minimal enzymatic activity of 0.2 IU/mL was needed for optimal asparagine deamination of 90% compared with the baseline. Horizontal line indicates 90% of asparagine depletion below pretreatment levels; vertical line, 0.2 IU/mL of asparaginase activity; and ASN, asparagine.
Finally, a population PD model was constructed which took into consideration the serum enzymatic asparaginase activity and serum asparagine. Based on the Michaelis-Menten equation, at steady state, the model predicted that serum asparagine should be deaminated completely up to 21 days after dose administration. However, the estimated Km for deamination of asparagine by asparaginase enzymatic activity was 39.84 μM, a value which is 1/3-fold higher that the Km estimated in pediatric patients with ALL.35 This may indicate that the presence of higher serum glutamine and other amino acids in the serum of adult patients may hinder the affinity of the enzymatic activity to deaminate asparagines efficiently.
One patient developed an Ab to pegaspargase on day 22 after the drug was administered. The emergence of the Ab was associated with immediate disappearance of pegaspargase enzyme activity and rebound of serum l-asparagine, but was not associated with any clinical manifestations of hypersensitivity.
Pegaspargase toxicity
The adverse effects attributed to pegaspargase are summarized in Table 3. Pegaspargase was well tolerated with predominantly grade 1 or 2 side effects. No allergic reactions, pancreatitis, or myelosuppression was noted. The most common side effects were elevated liver enzymes (76%), elevated bilirubin (72%), and hyperglycemia (76%). Elevated serum bilirubin levels were seen in 18 patients, but only 2 patients had grades 3 to 4 hyperbilirubinemia, and 3 patients had grades 3 to 4 elevated aspartate aminotransferase (AST)/alanine aminotransferase (ALT). The abnormal liver tests returned to normal without clinical manifestations of liver disease. Hyperglycemia was severe (grade 3 or 4) in only 4 (16%) patients, and then returned to baseline values. The plasma fibrinogen level dropped below 2.941 μM (100 mg/dL) in 15 (60%) patients, with a median nadir level of 2.59 μM (88 mg/dL). No patient developed evidence of bleeding. Plasma antithrombin III levels were below the baseline level in all 24 patients. In 16 (67%) patients, the antithrombin III level dropped below 50% of baseline, and the median nadir level was 45% of normal control plasma. In 11 patients the antithrombin III was measured serially; it declined in all patients by day 5, and remained low until returning to normal levels by approximately day 21 or later (Figure 5). One patient developed superior vena cava thrombosis related to a central venous cathether. No plasma was given for low antithrombin III. Cryoprecipitate was given when serum fibrinogen was less than approximately 1.764 μM (60 mg/dL). Anticoagulants were not used prophylactically, and Doppler studies of the legs were not done to look for silent deep vein thrombosis.
Number of patients with toxicity following pegaspargase administration (n = 25)
| Adverse effect . | Toxicity grade, no. of patients . | Total no. of patients . | ||
|---|---|---|---|---|
| Grades 1, 2 . | Grade 3 . | Grade 4 . | ||
| Hyperbilirubinemia | 16 | 1 | 1 | 18 |
| Elevated AST/ALT level | 16 | 2 | 1 | 19 |
| Hyperglycemia | 15 | 2 | 2 | 19 |
| Nausea/vomiting | 9 | 1 | 0 | 10 |
| Diarrhea | 4 | 0 | 0 | 4 |
| Constipation | 6 | 0 | 0 | 6 |
| Fever | 2 | 0 | 0 | 2 |
| Neuropathy | 5 | 0 | 0 | 5 |
| Fatigue | 2 | 0 | 0 | 2 |
| Deep vein thrombosis | 0 | 1 | 0 | 1 |
| Adverse effect . | Toxicity grade, no. of patients . | Total no. of patients . | ||
|---|---|---|---|---|
| Grades 1, 2 . | Grade 3 . | Grade 4 . | ||
| Hyperbilirubinemia | 16 | 1 | 1 | 18 |
| Elevated AST/ALT level | 16 | 2 | 1 | 19 |
| Hyperglycemia | 15 | 2 | 2 | 19 |
| Nausea/vomiting | 9 | 1 | 0 | 10 |
| Diarrhea | 4 | 0 | 0 | 4 |
| Constipation | 6 | 0 | 0 | 6 |
| Fever | 2 | 0 | 0 | 2 |
| Neuropathy | 5 | 0 | 0 | 5 |
| Fatigue | 2 | 0 | 0 | 2 |
| Deep vein thrombosis | 0 | 1 | 0 | 1 |
There were no allergic reactions or pancreatitis.
Serum antithrombin activity. The results are from 11 patients who had 2 or more serum specimens taken after a single intravenous dose of pegaspargase administration (2000 IU/m2). Day 0 indicates prior to pegaspargase. Each color indicates an individual patient. The results are represented as a percentage of normal control plasma.
Serum antithrombin activity. The results are from 11 patients who had 2 or more serum specimens taken after a single intravenous dose of pegaspargase administration (2000 IU/m2). Day 0 indicates prior to pegaspargase. Each color indicates an individual patient. The results are represented as a percentage of normal control plasma.
Response
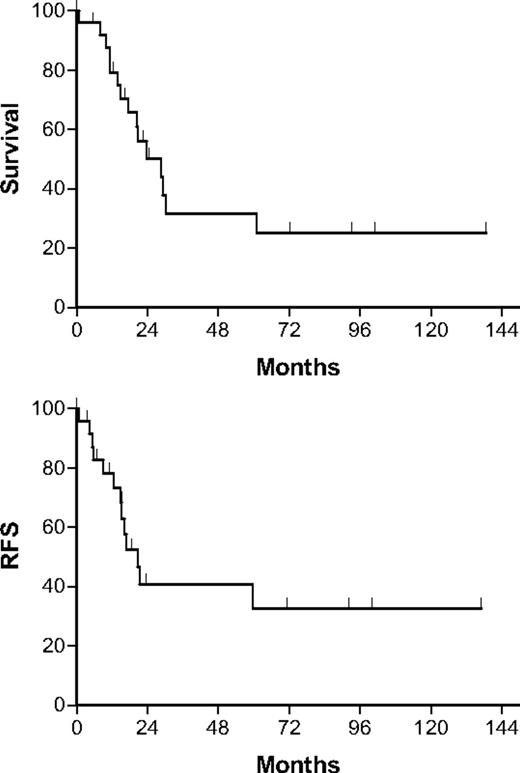
All but 1 of the 25 patients (96%; 95% CI = 80%-99.8%) achieved a CR, including 23 patients who were in CR after phase 1 of induction. Only 1 patient failed to achieve CR, and died of lung aspergillosis on day 27 of induction therapy. The 1 patient with the silent antipegaspargase Abs achieved a CR. Relapse occurred in 13 patients: 10 in the bone marrow, 1 with isolated CNS relapse, 1 in bone marrow and CNS, and 1 in bone marrow, CNS, and testis. One patient died after an allogeneic bone marrow transplantation (BMT) in first remission. A number of patients (10 [40%]) have not relapsed and are alive at a median follow-up interval of 36 months. At 4 years the overall survival and relapse-free survival were 31% and 40%, respectively (Figure 6).
Overall survival and relapse-free survival (RFS). The median follow-up was only 36 months as the study was conducted between 1995 and1999; since then, several patients were lost to follow-up and were censored at the time of last follow-up.
Overall survival and relapse-free survival (RFS). The median follow-up was only 36 months as the study was conducted between 1995 and1999; since then, several patients were lost to follow-up and were censored at the time of last follow-up.
Discussion
Asparaginases are included in most treatment protocols for both pediatric and adult patients with newly diagnosed ALL.47 This report provides pharmacokinetic and PD data on intravenous administration of pegaspargase in adults who are asparaginase naive. Because of concerns of excessive toxicity in elderly patients, inclusion was limited to adults 55 years or younger, and the conclusions may not be applicable to an older population. Although several adult ALL studies12,14,47 excluded adults older than 60 years, in others47-49 approximately 20% of the patients were older and therefore the cut-off age of 55 years limits the comparison between studies. It should also be emphasized that in our study pegaspargase was given on only one occasion, and only during induction therapy.
The mean plasma half-life of single intravenous injection of 2000 IU/m2 was 7 days, which is longer than the half-life of 5.73 and 6.0 days after a single intramuscular injection of a higher dose of 2500 IU/m2 reported in 2 studies of newly diagnosed children with ALL, but this difference is not statistically significant.32,35 The drug had a very long duration of asparagine deamination activity, determined phramocodynamically by plasma asparagine depletion, which is the most direct parameter of asparaginase activity. Asparagine depletion lasted at least 2 weeks in all patients, lasted 3 weeks in 81% of patients, and 4 weeks in 44% of patients. Importantly, we also demonstrated that for optimal asparagine deamination and depletion, the minimal therapeutic level of asparaginase enzymatic activity should be 0.2 IU/mL, which is similar to what was found recently in children,44,50 but higher than the levels of 0.1 IU/mL and 0.03 IU/mL that were used in other pediatric35,51 and adult studies.45 This level should be useful to investigators in future studies to assess the PD effect of the drug when only the enzymatic activity is measured. The population posthoc analyses demonstrated a long duration of serum concentration of enzymatic activity that was continuously present for 3 weeks in all patients and in several individual patients (20%) for even longer periods. Since only 18% of the patients have recovered asparagine levels at 3 weeks we suggest, at least for adults, an interval of 3 weeks between intravenous doses of pegaspargase, instead of 1- to 2-week intervals of intramuscular dosing used in children19,43,44 or adults.45 The clinical importance of a continuously long duration of asparaginase activity has been demonstrated in several pediatric studies in patients with recurring52 or newly diagnosed disease.18-20,35 There have been no such studies in adults with ALL, although in the Cancer and Leukemia Group B (CALGB) 9511 study, the survival of newly diagnosed patients was greater when the asparaginase activity was higher than 0.03 U/mL for at least 14 days after subcutaneous pegaspargase.45
A serious problem of asparaginase treatments is the production of antiasparaginase Abs that neutralize the enzymatic activity.23,34,35 As a result, plasma asparagine levels are not depleted after readministration of the drug, often leading to asparaginase resistance.2,30,32,33 The reported frequency of Ab formation is highly variable and has been found in as many as 79% of adults25 and 70% of children.27,34 Such Abs are often detected after development of clinically mild, moderate, or severe hypersensitivity reactions, but may also develop without clinical manifestations of hypersensitivity (“silent hypersensitivity”),1,2,29-31 although they are still associated with neutralization of subsequent asparaginase, which may be administered. Kurtzberg et al demonstrated that 50% of children with ALL in relapse, previously treated with E coli asparaginase, had “silent hypersensitivity” with the presence of serum antiasparaginase Abs.2 It has been suggested that pegaspargase might cause less Ab formation in patients with no prior exposure to asparaginase because of its low immunogenicity.35 This notion was supported in children by a randomized trial (CCG-1962 study) in newly diagnosed ALL: “silent” antiasparaginase Abs were detected after the first delayed induction phase in 42% of patients treated with the native asparaginase compared with 11% among the patients treated with pegaspargase.35 No such comparison has been done in adults, but similar to the pediatric study, 15% of the adults enrolled on the CALGB 9511 ALL trial who received 1 to 4 doses of subcutaneous pegaspargase formed Abs.45 During the 28 days of monitoring in our study, only 1 (4%) of the 25 adult patients developed “silent hypersensitivity,” occurring on day 22 after a single injection of intravenous pegaspargase and resulting in immediate disappearance of the enzymatic activity and normalization of serum asparagine levels. Similar to a previous report,53 the protein was still measured antigenically even after the enzymatic activity had disappeared, indicating that the protein was not rapidly removed from the circulation after binding to the Ab. It is unclear whether this lower rate of Ab production is related to the mode of administration or the fact that only 1 injection was given. The concurrent use of high-dose steroids could also have been responsible for the low level of Ab formation. Interestingly, in contrast to our finding, in some children the enzymatic activity of pegaspargase could be preserved despite the presence of Abs formed during prior exposure to E coli asparaginase2,32,51 or even pegaspargase.35
The clinical significance of Ab production, clinical hypersensitivity and resistance to asparaginase activity in ALL has been questioned. Larson et al26 in adults, and Woo et al54 in children found that developing hypersensitivity to the E coli asparaginase had no impact on overall clinical outcome; in children, the outcome was also unaffected by the presence of Abs.54 In contrast, the response rate was higher after receipt of a chemotherapy regimen containing pegaspargase in pediatric patients with ALL in second relapse with low-titer Abs to the E coli enzyme when compared with those with high-titer Abs.42 Further, an interim analysis of the pediatric CCG-1961 protocol showed that the presence of Abs without clinical hypersensitivity was correlated with an adverse outcome compared with patients who had no Abs and no clinical allergy, or to patients who had clinical allergy and were switched to Erwinia asparaginase.34
In children, the toxicities of equivalent dose of pegaspargase and E coli asparaginase were compared in 2 randomized studies in newly diagnosed patients. In both studies, the rate of side effects was very similar.19,35 In 1 study, 15 doses of pegaspargase caused less allergic reactions (13%) than 30 doses of the E coli form (21%) when given after remission.19 Without similar trials in adults, it is difficult to directly compare the toxicities between these 2 forms of asparaginase. However, our study would indicate that in adults aged 55 years or younger, a single dose of intravenous pegaspargase is not more toxic compared with equivalent multiple doses of E coli asparaginase.1,11,23 Very few grade 3 or 4 toxicities were seen, and no drug-related deaths or unexpected toxicities were observed. No allergic reactions were seen in any of our 25 patients. Interestingly, nonallergic adverse effects to pegaspargase were common in our study, but were predominantly mild and not life-threatening. Hepatotoxicity was the most common nonallergic side effect, although there were only 3 cases of grade 3 or 4 hyperbilirubinemia and/or liver enzyme elevation, which were reversible in all patients. The CALGB 9511 study, which did not have an upper age limit, reported grade 4 hyperbilirubinemia in 54% of patients who received 1 to 4 doses.45 Hypofibrinogenemia from pegaspargase has been shown in more than 50% of pediatric patients, which is similar to the rate in our study of adults.45 All of our patients were found to have low antithrombin III levels after receipt of intravenous pegaspargase. Nonetheless, clinical evidence of thrombosis was rarely encountered in our study. Of interest, the duration of low levels of plasma antithrombin III corresponded with the duration of the asparaginase serum enzymatic activity. Pancreatitis, the most serious side effect, was not observed after single-dose pegaspargase in any of our patients. This complication has been reported in 1% to 4% of more than 250 adults and children treated in several pegaspargase clinical trials1,23,41 and in up to 15% of patients after E colil-asparaginase.1,26,33
These safety observations are important, since all 3 forms of asparaginase are used via intramuscular injection in children and adults in the US due to the finding in the early pediatric experience that E coli asparaginase had greater toxicity and more severe allergic reactions after intravenous administration.55,56 Similar to our own current results, E coli, Erwinia, and pegylated forms of asparaginase have been administered intravenously to children in Europe without a higher incidence or severity of allergic or nonallergic side effects than that reported for intramuscular or subcutaneous injection routes.20,57,58 Furthermore, Aguayo et al59 reported no greater toxicity associated with intravenous pegaspargase in 32 adults with recurring or refractory ALL who had previously received asparaginase. It is thus apparent that pegaspargase can be given by the more convenient intravenous route, obviating painful intramuscular doses, without incurring greater toxicity. In addition, in our study intravenous administration resulted in an immediate complete asparagine deamination (at 2 hours), while maximal deamination in a pediatric study after intramuscular injection35 was at day 5, with the potential for subtherapeutic drug activity during this time.
The 96% CR rate in our trial is as good as the 80% to 91% published response rates of large clinical trials of patients younger than 60 years and a similar median age which used frontline ALL remission induction regimens that included E coli asparaginase in combination with similar chemotherapy agents.12,14,47 Our study focused on the induction phase, and no conclusions can be drawn on the overall outcome.
Based on our results, we recommend that 1 dose of pegaspargase can replace multiple doses of native asparaginase during the induction phase, at least for patients aged 55 years or younger. Future trials should study multiple doses of pegaspargase in the postremission phase. In that respect, several pediatric studies have suggested that intensive and long postremission treatment with asparaginase is associated with a better clinical outcome without added morbidity.19,21 In poor-risk pediatric patients with ALL, the augmented BFM protocol which escalated the postinduction dose of several drugs, including an 3.5-fold increase in E coli asparaginase, improved the survival rate when compared with the standard BFM protocol.8 The role of dose intensification and prolonged duration of asparaginase administration has not been studied in adults. Our results provide the pharmacokinetic, PD, and toxicity profile data to study the effect of longer-term asparaginase enzymatic activity and asparagine depletion in adults with ALL. To that end, we are currently conducting a clinical trial to determine the toxicity and rate of asparaginase Ab formation after multiple doses of postremission pegaspargase in adults with ALL.
Authorship
Contribution: D.D. designed the trial, performed research, analyzed data, and wrote the paper; H.Y. collected and analyzed data; L.J.C. designed the trial; K.W. performed research and collected and analyzed data; A.M.L. contributed to writing the paper; A.P.P. contributed analytical tools; and V.L.A. designed the trial, performed research, analyzed data, contributed analytical tools, and contributed to writing the paper
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Dan Douer, Division of Hematology, University of Southern California/Norris Cancer Center, 1441 Eastlake Ave, Rm 3460, Los Angeles, CA 90033; e-mail: douer_d@ccnt.hsc.usc.edu.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
Supported in part by research funding from Aventis Pharmaceutical (D.D.), and in part by an Institutional support grant (CHLA) (V.I.A.).



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal