Abstract
The majority of patients with systemic mast cell disease express the imatinib-resistant Asp816Val (D816V) mutation in the KIT receptor tyrosine kinase. Limited treatment options exist for aggressive systemic mastocytosis (ASM) and mast cell leukemia (MCL). We evaluated whether PKC412, a small-molecule inhibitor of KIT with a different chemical structure from imatinib, may have therapeutic use in advanced SM with the D816V KIT mutation. We treated a patient with MCL (with an associated myelodysplastic syndrome (MDS)/myeloproliferative disorder [MPD]) based on in vitro studies demonstrating that PKC412 could inhibit D816V KIT-transformed Ba/F3 cell growth with a 50% inhibitory concentration (IC50) of 30 nM to 40 nM. The patient exhibited a partial response with significant resolution of liver function abnormalities. In addition, PKC412 treatment resulted in a significant decline in the percentage of peripheral blood mast cells and serum histamine level and was associated with a decrease in KIT phosphorylation and D816V KIT mutation frequency. The patient died after 3 months of therapy due to progression of her MDS/MPD to acute myeloid leukemia (AML). This case indicates that KIT tyrosine kinase inhibition is a feasible approach in SM, but single-agent clinical efficacy may be limited by clonal evolution in the advanced leukemic phase of this disease. (Blood. 2005; 106:2865-2870)
Introduction
Mastocytosis comprises a spectrum of disorders related to the abnormal growth and accumulation of mast cells in one or more organs. The World Health Organization (WHO) recognizes 4 systemic mastocytosis (SM) subtypes: indolent SM (ISM), SM with associated clonal hematologic non-mast-cell lineage disease (SM-AHNMD), aggressive SM (ASM), and mast cell leukemia (MCL).1 The AHNMD typically consists of a myelodysplastic syndrome (MDS), chronic myeloproliferative disorder (MPD), overlap MDS/MPD, or acute myelogenous leukemia.2
The proto-oncogene KIT encodes a transmembrane receptor tyrosine kinase that is expressed on mast cells and other hematopoietic lineages.3 A pathogenetic hallmark of the majority of SM cases in adults is the Asp816Val (D816V) somatic mutation in the catalytic domain of the KIT gene.1,4,5 This transforming mutation results in enhanced mast cell survival and proliferation because of constitutive activation of the tyrosine kinase activity of KIT, independent of KIT ligand.6
The management of patients with SM involves attempting to control symptoms related to mediator release from mast cells and to curtail organ damage caused by infiltrating mast cells.2 Advanced mast cell disease (eg, ASM and MCL) carries a poor prognosis. Current treatments such as interferon-alpha with or without corticosteroids and cladribine exhibit low response rates that are usually partial in nature.7-9 The D816V KIT mutation of SM has been shown to be resistant to the tyrosine kinase inhibitor imatinib mesylate (Gleevec) both in vitro and in vivo.10-12 We therefore evaluated the effects of PKC412 (N-benzoyl-staurosporine, Novartis, Basel Switzerland), an alternative small molecule inhibitor of multiple type III receptor tyrosine kinases, including the KIT tyrosine kinase, in a patient with mast cell leukemia.
Study design
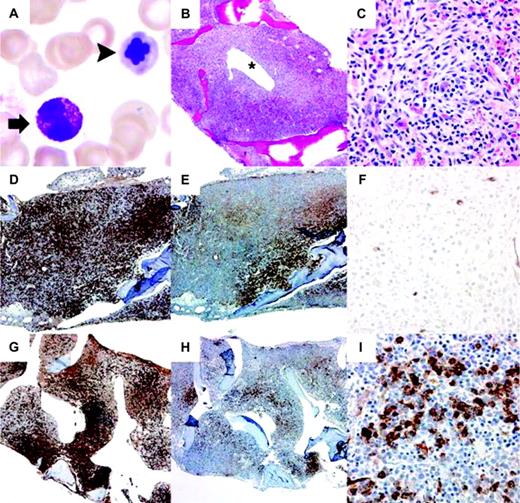
In April 2003, a previously healthy 48-year-old woman presented with a 4-week history of malaise, fever, night sweats, and rash. Notable physical findings included 3-cm palpable splenomegaly, a diffuse petechial rash, and scattered less than 1.0 cm hyperpigmented macular lesions on the trunk and extremities. Biopsy of the skin lesions revealed a mast cell infiltrate with no definite staining of mast cells by CD25. Table 1 shows laboratory studies at initial presentation. The peripheral blood was remarkable for an increase in myeloid immaturity and 11% circulating mast cells. A bone marrow aspirate revealed 8% myeloblasts, trilineage dysplasia, and markedly decreased megakaryocytes. The bone marrow biopsy revealed 90% to 100% cellularity, with mast cells accounting for 70% of marrow cellularity. Spindled-cell aggregates of mast cells (Figure 1B-C) were highlighted by immunohistochemical staining for CD117, mast cell tryptase, and CD25 (Figure 1D-E), but were negative for CD2 by flow cytometry immunophenotyping. Testing of the bone marrow aspirate revealed heterozygosity for the D816V KIT mutation. Cytogenetic analysis showed a normal female karyotype and polymerase chain reaction (PCR) for BCR-ABL was negative. The findings were consistent with MCL with an AHNMD, MDS/MPD.
Patient laboratory values before and during treatment with PKC412
. | Initial Presentation . | Pretreatment . | Cycle 1 . | Cycle 2 . | Cycle 3/Relapse . |
|---|---|---|---|---|---|
| Date | Apr 2003 | Jun 2003 | Jun-Jul 2003 | Jul-Aug 2003 | Aug-Sep 2003 |
| Hematology | |||||
| WBCs/mm3* | 15.8 | 8.4 | 8.0 | 7.9 | 12.2 |
| Differential count, % | |||||
| Segmented neutrophils | 14 | 19 | 46 | 44 | 20 |
| Bands | 10 | 6 | 29 | 26 | 7 |
| Lymphocytes | 19 | 19 | 11 | 17 | 7 |
| Monocytes | 8 | 5 | 7 | 8 | 0 |
| Eosinophils | 0 | 2 | 0 | 1 | 0 |
| Basophils | 0 | 0 | 0 | 0 | 0 |
| Immature myeloids | 31 | 3 | 2 | 4 | 51 |
| Blasts | 5 | 0 | 0 | 0 | 8 |
| Mast cells | 11 | 46 | 5 | 0 | 2 |
| Nucleated red blood cells/100 WBCs | 7 | 47 | 4 | 4 | 0 |
| Hemoglobin, g/dL† | 9.8∥ | 8.5∥ | 8.7∥ | 7.5∥ | 9.5∥ |
| Hematocrit, % | 29.8∥ | 26.6∥ | 25.8∥ | 22.8∥ | 31.0∥ |
| Platelets/mm3‡ | 5000∥ | 7000∥ | 13 000∥ | 16 000∥ | 11 000∥ |
| Chemistry | |||||
| Albumin, g/dL† | 2.4 | 2.2 | 2.8 | 3.4 | 2.3 |
| Total bilirubin, mg/dL§ | 1.2 | 4.8 | 2.1 | 1.3 | 13.6 |
| Direct bilirubin, mg/dL§ | 0.5 | 2.8 | 1.1 | 0.7 | 7.5 |
| LDH, U/L | 552 | 769 | 239 | 227 | 595 |
| Mastocytosis-related findings | |||||
| Serum histamine, ng/dL | ND | 6910 | 1031 | 779 | 2525 |
| Serum tryptase, μg/L | > 200 | > 200 | > 200 | > 200 | > 200 |
. | Initial Presentation . | Pretreatment . | Cycle 1 . | Cycle 2 . | Cycle 3/Relapse . |
|---|---|---|---|---|---|
| Date | Apr 2003 | Jun 2003 | Jun-Jul 2003 | Jul-Aug 2003 | Aug-Sep 2003 |
| Hematology | |||||
| WBCs/mm3* | 15.8 | 8.4 | 8.0 | 7.9 | 12.2 |
| Differential count, % | |||||
| Segmented neutrophils | 14 | 19 | 46 | 44 | 20 |
| Bands | 10 | 6 | 29 | 26 | 7 |
| Lymphocytes | 19 | 19 | 11 | 17 | 7 |
| Monocytes | 8 | 5 | 7 | 8 | 0 |
| Eosinophils | 0 | 2 | 0 | 1 | 0 |
| Basophils | 0 | 0 | 0 | 0 | 0 |
| Immature myeloids | 31 | 3 | 2 | 4 | 51 |
| Blasts | 5 | 0 | 0 | 0 | 8 |
| Mast cells | 11 | 46 | 5 | 0 | 2 |
| Nucleated red blood cells/100 WBCs | 7 | 47 | 4 | 4 | 0 |
| Hemoglobin, g/dL† | 9.8∥ | 8.5∥ | 8.7∥ | 7.5∥ | 9.5∥ |
| Hematocrit, % | 29.8∥ | 26.6∥ | 25.8∥ | 22.8∥ | 31.0∥ |
| Platelets/mm3‡ | 5000∥ | 7000∥ | 13 000∥ | 16 000∥ | 11 000∥ |
| Chemistry | |||||
| Albumin, g/dL† | 2.4 | 2.2 | 2.8 | 3.4 | 2.3 |
| Total bilirubin, mg/dL§ | 1.2 | 4.8 | 2.1 | 1.3 | 13.6 |
| Direct bilirubin, mg/dL§ | 0.5 | 2.8 | 1.1 | 0.7 | 7.5 |
| LDH, U/L | 552 | 769 | 239 | 227 | 595 |
| Mastocytosis-related findings | |||||
| Serum histamine, ng/dL | ND | 6910 | 1031 | 779 | 2525 |
| Serum tryptase, μg/L | > 200 | > 200 | > 200 | > 200 | > 200 |
WBCs indicates white blood cells; LDH, lactate dehydrogenase.
To convert to × 109 cells per liter, multiply by 1.
To convert to grams per liter, multiply by 10.
To convert to × 109 platelets per liter, divide by 1000.
To convert to micromoles per liter, multiply by 17.1.
Transfusion-dependent.
During the following 2 months, the patient's disease progressed with 30% to 50% circulating mast cells. The patient was supported with red blood cell and platelet transfusions, famotidine, lansoprazole, loratadine, and cromolyn sodium for mediator-related symptoms, including pruritis and persistent diarrhea. She developed progressive liver dysfunction, severe ascites, and a portal vein thrombosis. She was hospitalized for marked deterioration of her clinical status. She declined treatment with alpha-interferon. Findings of a repeat bone marrow biopsy were similar to the specimen at initial presentation. The patient agreed to participate in a compassionate use trial of PKC412. The Stanford Medical Center institutional review board approved the study, and the patient gave written informed consent according to the Declaration of Helsinki. PKC412 was initiated in June 2003 at 100 mg twice daily as 28-day cycles, the recommended dose from phase 1 studies in acute myelogenous leukemia (AML). The patient was also treated with furosemide, spirinolactone, and tincture of opium for diarrhea.
Histology and immunophenotyping studies
For immunohistochemistry, antibodies included CD25 (4C9; Novocastra, Newcastle upon Tyne, United Kingdom), CD34 (My10) (Becton Dickinson, San Jose, CA); CD117 (KIT, Dako, Carpinteria, CA), and mast-cell tryptase (G3, Chemicon, Temecula, CA). Direct dual-parameter flow cytometry was performed on a FACSCalibur instrument (Becton Dickinson). Fluorescein isothiocyanate, phycoerythrin, and tricolor-conjugated monoclonal antibodies were used: CD45 (H130; Caltag, Burlingame, CA); CD34 (581) CD64 (22) (Immunotech, Marseille, France); CD2 (S5.2), CD117 (104D2), and CD25 (2A3) (Becton Dickinson).
PKC412 pharmacokinetics (PK)
DNA constructs, cell cultures, and cell growth inhibition studies
The D816V mutation of human KIT (lacking amino acids 510-513, GNNK) in pCDNA3 was generated (Transformer Site-Directed Mutagenesis kit, Clontech, Mountain View, CA), then subcloned into the XhoI site of retroviral vector MSCV-IRES-GFP. Retroviral transduced Ba/F3 cells were selected for interleukin-3 (IL-3) independent growth. 1 × 104 cells were plated in triplicate in 96 well plates with or without indicated concentrations of drug and the absence of IL-3. After 24 hours, 1 μCi (0.037 MBq) 3H-thymidine was added, followed by a 4-hour incubation. Cells were harvested and 3H-thymidine incorporations determined.
Peripheral blood and bone marrow findings before and after treatment with PKC 412. (A-F) Before treatment. (G-I) After treatment. (A) Circulating mast cell (arrow, left) and dysplastic nucleated red blood cell (arrowhead, right) in peripheral blood. Wright-Giemsa, 1000 ×. (B) Hypercellular bone marrow with aggregates of pale-staining mast cells surrounding a dilated sinus (*). Hematoxylin and eosin, 40 ×. (C) Whorled nodule of mast cells with characteristic clear cytoplasm including spindled forms. Hematoxylin and eosin, 400 ×. (D) Increased mast cells show a nodular and interstitial pattern in the bone marrow occupying approximately 70% marrow cellularity. Mast cell tryptase, 40 ×. (E) The majority of mast cells are highlighted by CD25 antibody. CD25, 40 ×. (F) Few numbers of CD34-positive blasts (∼5%) detected on bone marrow biopsy. CD34, 400 ×. (G) The posttreatment bone marrow shows a similar mast cell burden as seen prior to treatment. Mast cell tryptase, 40 ×. (H) A slight decrease in CD25-positive mast cells (∼40% of marrow cellularity) is noted after therapy. CD25, 40 ×. (I) Increased numbers of CD34-positive blasts (10%-20%) in bone marrow biopsy indicating progression of this patient's AHNDMD, MDS/MPD. CD34, 400 ×.
Peripheral blood and bone marrow findings before and after treatment with PKC 412. (A-F) Before treatment. (G-I) After treatment. (A) Circulating mast cell (arrow, left) and dysplastic nucleated red blood cell (arrowhead, right) in peripheral blood. Wright-Giemsa, 1000 ×. (B) Hypercellular bone marrow with aggregates of pale-staining mast cells surrounding a dilated sinus (*). Hematoxylin and eosin, 40 ×. (C) Whorled nodule of mast cells with characteristic clear cytoplasm including spindled forms. Hematoxylin and eosin, 400 ×. (D) Increased mast cells show a nodular and interstitial pattern in the bone marrow occupying approximately 70% marrow cellularity. Mast cell tryptase, 40 ×. (E) The majority of mast cells are highlighted by CD25 antibody. CD25, 40 ×. (F) Few numbers of CD34-positive blasts (∼5%) detected on bone marrow biopsy. CD34, 400 ×. (G) The posttreatment bone marrow shows a similar mast cell burden as seen prior to treatment. Mast cell tryptase, 40 ×. (H) A slight decrease in CD25-positive mast cells (∼40% of marrow cellularity) is noted after therapy. CD25, 40 ×. (I) Increased numbers of CD34-positive blasts (10%-20%) in bone marrow biopsy indicating progression of this patient's AHNDMD, MDS/MPD. CD34, 400 ×.
PCR analysis of the KIT gene
Genomic DNA (gDNA) was isolated from ficolled peripheral blood or bone marrow mononuclear cell specimens (200 μL) with the QIAamp DNA blood minikit (Qiagen, Valencia, CA). PCR of the exon 17 region of the KIT gene containing the site of the D816V mutation was performed with the primer sequences KIT17S: TGGCAGCCAGAAATATCCTC and KIT17AS: CACGGAAACAATTTTTATCGAA. Amplification was carried out on an ABI 9600 thermocycler. The 182-nucleotide (nt) PCR product was purified after electrophoresis on a 2% agarose gel. Sequencing reactions were analyzed on an ABI Prism 377 DNA Sequencer.
RNA (1 μg) from ficolled bone marrow samples was isolated using an RNeasy minikit (Qiagen, Valencia, CA). First-strand cDNA was generated using oligo(dT)12-18 primers (Promega, Madison, WI) and Omniscript reverse transcriptase (Qiagen) before amplification with PCR KIT13: GACGAGTTGGCCCTAGAC and PCR KIT14: AGTTGGAGTAAATATGATTGGTG using PfuTurbo polymerase (Stratagene, La Jolla, CA).14 The resulting 538-base pair (bp) fragment was gel purified then cloned using Zero Blunt TOPO PCR cloning kit (Invitrogen, Carlsbad, CA). For each cloning, 3 positive clones were selected for sequencing (by Sequentech, Mountain View, CA) at both strands.
In-depth mutational analysis of all KIT exons (1-21) and the corresponding 30 bp of flanking intronic sequence was conducted using fluorescent denaturing high-performance liquid chromatography (DHPLC) technology15 and Surveyor mismatch cleavage analysis16 both with the WAVE HS System (Transgenomic, Omaha, NE). Purified gDNAs (5-10 ng) were subjected to 35 cycles of PCR using Optimase, a proofreading DNA polymerase (Transgenomic) and primer pairs for each KIT amplicon. Negative gDNA controls were included in the amplifications. Aliquots (3-15 μL) were scanned for mutations by DHPLC, confirmed by Surveyor mismatch cleavage, and identified with bidirectional sequence analysis on an ABI 3100 sequencer using BigDye terminator chemistry (Applied Biosystems, Foster City, CA). For semiquantitative determination of mutant and normal allele frequencies, relative peak areas of DHPLC elution profiles and Surveyor mismatch cleavage products were determined after normalization and comparison to reference controls using the WAVE Navigator software.
The sensitivity of the DHPLC assay as compared to direct DNA sequencing was determined by mixing a mast cell leukemia cell-line (HMC-1) containing the KIT D816V mutation6 with wild-type KIT cells at mutant allele frequencies of 0.5%, 0.75%, 1%, 2%, 5%, 7.5%, 10%, 20%, 50%, and 90%. Genomic DNA was extracted from each sample as described, and mutation analysis was performed in triplicate. The D816V KIT mutation was confirmed by DHPLC in all replicates down to an allelic frequency of 1%, as compared to 7.5% for DNA sequencing.
Ex vivo analysis of KIT phosphorylation during PKC412 treatment
Cell lysates were prepared from frozen peripheral blood and bone marrow aspirates of the patient before and after treatment with PKC412. KIT protein immunoprecipitation was performed using a cocktail of anti-KIT antibodies (M-14, C-19, and Ab81; all from Santa Cruz Biotechnology, Santa Cruz, CA), as previously described.17 For Western blot analysis, total KIT protein was detected with anti-KIT antibody C-19 (Santa Cruz Biotechnology), and phosphorylated KIT protein was visualized by probing duplicate blots with a phospho-KIT-specific antibody (Tyr719; Cell Signaling Technology, Beverly, MA).
Results and discussion
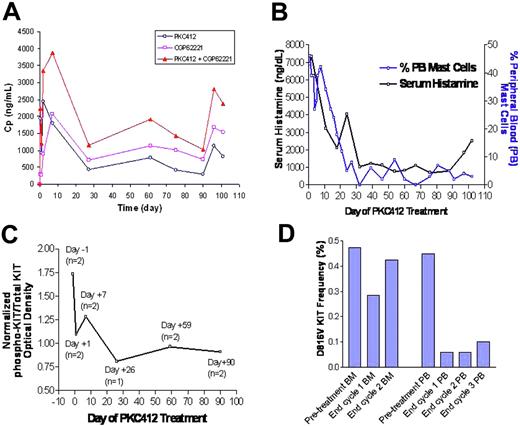
Table 1 lists relevant abnormal laboratory studies at the start of treatment, best responses during subsequent 28-day cycles of PKC412 treatment, and findings at disease progression. During cycle 1, the patient's Karnofsky performance status improved from 20% to 70%. She experienced improvement in her diarrhea and ascites, and her portal vein thrombosis recanalized. Mild reduction of splenomegaly was noted on physical examination. The percentage of peripheral blood mast cells decreased from 46% to 5% (Figure 2B), accompanied by increasing myeloid maturity (Table 1). The total/direct bilirubin decreased from 82.08/47.88 μM (4.8/2.8 mg/dL) to 35.91/18.81 μM (2.1/1.1 mg/dL), and the lactate dehydrogenase (LDH) decreased from 769 to 239 U/L. The serum histamine decreased from 6910 ng/dL to 1031 ng/dL (Figure 2B), but the serum tryptase remained more than 200 μg/L. A bone marrow biopsy at the end of cycle 1 showed a decrease in myeloblasts to lower than 5%, but there was persistent dysplasia and both interstitial and nodular aggregates of mast cells, comprising 70% of the marrow cellularity (similar to baseline).
Changes in the pharmacokinetics of PKC412 and patient mast cell disease-related parameters during PKC412 therapy. (A) Trough plasma concentration-time profiles of PKC412 and its major active metabolite CGP62221 and the sum of PKC412 and CGP62221 in the mast cell leukemia patient receiving PKC412 100 mg twice a day between day 1 and day 90, and 75 mg three times a day starting from day 90. (B) Serum histamine level and percent peripheral blood mast cells quantified by manual differential. (C) Normalized phospho-KIT/total KIT optical density ratio. The number of samples analyzed at each time point is shown in parentheses. (D) Semiquantitative DHPLC determination of the D816V KIT mutation frequency in the bone marrow and peripheral blood.
Changes in the pharmacokinetics of PKC412 and patient mast cell disease-related parameters during PKC412 therapy. (A) Trough plasma concentration-time profiles of PKC412 and its major active metabolite CGP62221 and the sum of PKC412 and CGP62221 in the mast cell leukemia patient receiving PKC412 100 mg twice a day between day 1 and day 90, and 75 mg three times a day starting from day 90. (B) Serum histamine level and percent peripheral blood mast cells quantified by manual differential. (C) Normalized phospho-KIT/total KIT optical density ratio. The number of samples analyzed at each time point is shown in parentheses. (D) Semiquantitative DHPLC determination of the D816V KIT mutation frequency in the bone marrow and peripheral blood.
During the second cycle of PKC412, the peripheral blood mast cell count was undetectable or below 5% (Figure 2B), myeloid maturity persisted, and there was a 2-week period of platelet transfusion independence. The serum histamine decreased further, to 779 ng/dL (Figure 2B). The total/direct bilirubin almost normalized to 22.23/11.97 μM (1.3/0.7 mg/dL). At the end of cycle 2, a repeat bone marrow biopsy showed a decrease in the proportion of CD25+ mast cells to 40% of marrow cellularity (Figure 1H) and an increase in myeloblasts to 10% to 20% of marrow cellularity by CD34 immunohistochemical staining (Figure 1I). During cycle 3 of treatment, the patient exhibited signs of disease progression. Laboratory findings included an increasing white blood cell (WBC) count with reappearance of myeloid immaturity and 5% to 10% myeloblasts in the peripheral blood and loss of platelet transfusion independence. Despite an increase in the PKC412 dose to 75 mg 3 times daily, the patient experienced deterioration of her performance status in conjunction with progressive liver failure. The patient expired on day 111 after initiation of PKC412 treatment. At the time of disease progression, peripheral blood mast cells generally remained less than 5% (Figure 2B).
Side effects of PKC412
PKC412 was generally well tolerated. The patient experienced grade 1 to 2 nausea and vomiting (National Cancer Institute version 3.0 Common Terminology Criteria for Adverse Events)18 with a suspected relationship to PKC412. Grade 4 hyperbilirubinemia developed during relapse, which was considered unlikely related to PKC412 since the patient presented with liver disease.
Pharmacokinetics
PKC412 trough plasma concentrations increased in the first 3 days and reached a maximum trough concentration of 2450 ng/mL on day 3, and then started to decline slowly and reached a new steady-state concentration of approximately 450 ng/mL on day 28 (Figure 2A). It appeared that the plasma concentration of PKC412 showed a trend of decrease in cycle 3 (days 60 to 90) until the dose was increased on day 90. On day 90, PKC412 and CGP62221 concentrations were 297 ng/mL and 730 ng/mL, respectively. After the PKC412 dose was increased from 100 mg twice a day to 75 mg three times a day, both PKC412 and CGP62221 concentrations were elevated substantially.
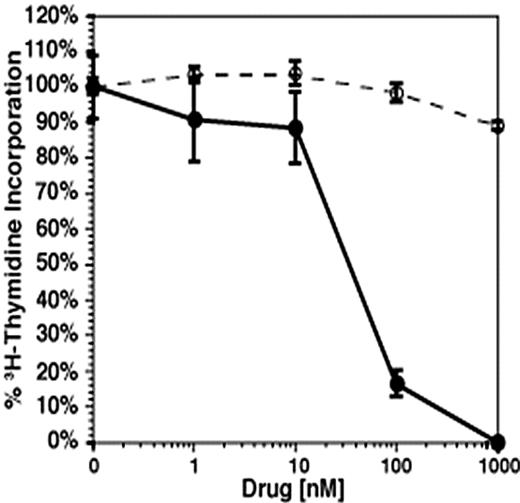
In vitro analysis of the effects of PKC412 on D816V KIT-transformed cell growth
The D816V KIT mutant stably transformed Ba/F3 cells to IL-3-independent growth (data not shown). As measured by 3H-thymidine incorporation, D816V KIT-transformed Ba/F3 cells were resistant to treatment with imatinib (Figure 3). In contrast, PKC412 effectively inhibited the growth of D816V KIT-transformed Ba/F3 cells with a cellular 50% inhibitory concentration (IC50) of approximately 30 nM to 40 nM (Figure 3). Using Western blot analysis of lysates from PKC412-treated Ba/F3 cells, we (J.D.G. and D.G.G) recently demonstrated reduction of the phosphotyrosine content of both c-KIT and the downstream effector STAT3, but not STAT5.19 Previous reports have shown that STAT3 is aberrantly phosphorylated by D816V KIT.20,21
Ba/F3-KIT D816V is sensitive to PKC-412 but not to imatinib. Plotted is the percentage of 3H-thymidine incorporation in drug-treated wells relative to no drug controls. Cells were treated with imatinib (dashed lines, ○) or PKC412 (solid line, •) for 24 hours in the presence of 10 ng/mL IL-3 and the absence of recombinant human stem cell factor (SCF). Plotted is the percent 3H-thymidine incorporation in drug-treated wells relative to no drug controls. Data are the mean of triplicates (plot standard deviation). PKC412 IC50 30 nM-40 nM.
Ba/F3-KIT D816V is sensitive to PKC-412 but not to imatinib. Plotted is the percentage of 3H-thymidine incorporation in drug-treated wells relative to no drug controls. Cells were treated with imatinib (dashed lines, ○) or PKC412 (solid line, •) for 24 hours in the presence of 10 ng/mL IL-3 and the absence of recombinant human stem cell factor (SCF). Plotted is the percent 3H-thymidine incorporation in drug-treated wells relative to no drug controls. Data are the mean of triplicates (plot standard deviation). PKC412 IC50 30 nM-40 nM.
PCR of the KIT gene
Using PCR of KIT exon 17 followed by direct sequencing or sequencing of cloned RT-PCR products, the D816V KIT mutation was detected in the patient's bone marrow at the time of initial presentation in April 2003 and from peripheral blood after completion of 1 cycle of PKC412. However, these methods could not detect the D816V KIT mutation in the bone marrow after 2 cycles of therapy or from peripheral blood obtained at the completion of 3 cycles of PKC412 (during disease progression). All samples were re-evaluated with a more sensitive, semiquantitative mutation detection approach using DHPLC/Surveyor mismatch cleavage analysis (via WAVE DHPLC) and confirmatory sequencing. This method detected the D816V KIT mutation at a similar frequency in pretreatment and follow-up marrows, but an 80% decrease in the frequency of the mutation was observed in the peripheral blood through cycles 1 and 3 (Figure 2D), consistent with the marked decline in circulating mast cells (Figure 2B). Screening of the entire KIT coding region and splice junctions detected no additional mutations during treatment and at relapse.
Ex vivo analysis of KIT phosphorylation during PKC412 treatment
The densitometric signal obtained for phospho-KIT (eg, activated KIT) was, in each case, normalized to the densitometric signal obtained for total KIT from the same sample. Since KIT is predominantly expressed on mast cells, this ratio controls for change in mast cell number from sample to sample. Because of insufficient bone marrow material for serial assessment of activated KIT, the patient's peripheral blood was used instead. The mean phospho-KIT/total KIT optical density declined during therapy (Figure 2C), by -26% on day 7 of treatment, to -53% on day 26 of treatment. There was no relative increase in KIT phosphorylation in the peripheral blood at the time of relapse (day 90).
PKC412 is an inhibitor of the family of FLT3, KIT, vascular endothelial growth factor receptor 2, platelet-derived growth factor receptor (PDGFR), and fibroblast growth factor receptor (FGFR) tyrosine kinases.22-24 It is currently under evaluation in phase 2 clinical trials of AML associated with mutated FLT3.25 PKC412 also demonstrated activity in a patient with stem cell myeloproliferative disorder (MPD) with the constitutively activated ZNF198-FGFR1 fusion tyrosine kinase.24 PKC412 was previously shown to be effective in a murine model of FIP1L1-PDGFR-α-induced myeloproliferative disease containing the imatinib-resistant T674I mutation.26 Accordingly, we hypothesized that PKC412 might also be useful in SM disease related to the imatinib-resistant D816V KIT mutation.
We demonstrated that PKC412 could inhibit D816V KIT-transformed cells at an IC50 of 30 nM to 40 nM, whereas these cells exhibit no significant inhibition by imatinib at concentrations of more than 1 μM. These in vitro results prompted us to initiate a trial of PKC412 in our patient with mast cell leukemia. Our patient experienced substantial improvement in her performance status and mast cell-related symptoms. Her portal vein thrombosis recanalized, ascites decreased, and liver function improved. These findings constitute a partial response by proposed SM response criteria.27 In addition, there was improvement in mast cell disease-related laboratory findings, including a marked decrease in peripheral blood mast cells and serum histamine level, associated with decreased KIT phosphorylation and D816V KIT mutation frequency. Persistent elevation of the serum tryptase level with PKC412 therapy may reflect ongoing infiltration of the bone marrow and other sites with mast cells, or the serum tryptase may have remained increased due to the patient's associated MDS/MPD.1,28
In contrast to the peripheral blood, there was minimal reduction of the burden of mast cells within the bone marrow. In phase 2 trials of FLT3 tyrosine kinase inhibitors (including PKC412) in AML, significant reductions in the percentage of peripheral blood blasts have frequently been observed without a corresponding decrease in bone marrow blasts.25 These findings suggest that bone marrow mast cells and leukemic blasts may somehow be protected from this class of drugs by factors related to the bone marrow microenvironment.29 If this is the case, then the identification of such factors and approaches for counteracting their effects would be important for developing new approaches for the effective and long-term treatment of these disorders.
PK results from this one patient suggest that PKC412 and its presumed active metabolite reached an effective level in the first week, when clinical responses were first observed, and the concentrations were maintained thereafter at generally the same levels between the end of months 1 through 3 of treatment (∼500 ng/mL for PKC412 alone and ∼1500 ng/mL for the sum of PKC412 and CGP62221). Although it cannot be concluded that the concentrations of PKC412 and CGP62221 were maintained above an effective level during this period, the quantity of D816V KIT-mutated DNA remained stable in the blood during cycles 2 and 3. Also, an increase of dosage to 75 mg three times a day on day 90 resulted in a rise in PK levels to troughs in the range of the first cycle of therapy, yet did not result in further improvement of the clinical findings, suggesting that inadequate PK was unlikely to be the cause for disease progression. The decreasing plasma concentrations are probably related to CYP3A4 enzyme induction by PKC412 and its metabolites.25
In this case, disease progression was related to transformation of the patient's MDS/MPD to AML. This is supported by the increasing percentage of myeloblasts and immature myeloid cells (but not mast cells) in the peripheral blood and bone marrow at the time of relapse. It is unknown whether this disease progression represents some form KIT-dependent or KIT-independent resistance of the patient's MCL to PKC412 therapy. However, screening of all exons of the KIT gene at the time of relapse did not reveal any other mutations that could have attributed to resistance to targeted therapy with PKC412. Also, there was no rebound increase in KIT phosphorylation at the time of relapse. We hypothesize that additional genetic mutations could have contributed to a clonal expansion of more phenotypically immature cells/blasts.
Taken together, these results indicate that PKC412 has promise in the treatment of aggressive forms of SM that are associated with the D816V KIT mutation. Akin to the more favorable experience with imatinib in chronic versus more advanced BCR-ABL-positive CML, it may also be useful to explore the efficacy of this agent in symptomatic patients with SM with less advanced disease. Use of PKC412 in this case provides the first proof-of-principle in humans that resistance of the D816V KIT tyrosine kinase to inhibition by imatinib can be circumvented with a structurally different small molecule inhibitor that targets the same protein.
Prepublished online as Blood First Edition Paper, June 21, 2005; DOI 10.1182/blood-2005-04-1568.
Supported in part by grants from the National Institutes of Health (K23HL04409 [J.G.]; CA66996 and DK50654 [D.G.G.]; and AI-23990, CA-72074, and AI-41995 [Project 1] [S.J.G.]); a grant from the Leukemia and Lymphoma Society (D.G.G.); and a postdoctoral fellowship grant no. PF-02-133-01-LIB from the American Cancer Society (J.D.G.). D.G.G. is an investigator of the Howard Hughes Medical Institute.
P.S.C. and Y.W. are employed by a company (Novartis Pharmaceuticals) whose product was studied in the present work.
J.G. participated in the writing of the manuscript, design of the clinical trial protocol, treatment of the patient, and interpretation of the data; C.B., J.R., and S.E.C. participated in treatment of the patient; J.D.G. performed the in vitro cell growth inhibition studies and KIT immunoprecipitation experiments with PKC412; D.G.G. participated in the experimental design of these studies and provided the in vitro data to support the use of PKC412 in this patient; C.-C.C. and S.J.G. performed sequencing of cloned RT-PCR products containing the KIT sequence; S.J.G. also contributed to the writing of the manuscript and interpretation of the data; Y.W. performed the pharmacokinetic studies; P.S.C. provided PKC412 for the in vitro studies and treatment of the patient and contributed to writing of the manuscript; S.L.L. and J.A.D. performed semiquantitative D816V KIT mutation analysis and screening of all KIT exons and interpretation of these data; J.H.L. performed initial direct sequencing of the KIT gene from genomic DNA before and during PKC412 therapy; T.I.G. and D.A.A. performed the immunohistochemical and flow cytometric analysis of patient samples and contributed to writing of the manuscript; L.N. generated the experimental design for the KIT phosphorylation studies; T.K. and C.W. performed the KIT phosphorylation experiments; and M.C.H. performed in vitro analysis of the effects of PKC412 on D816V-transformed cell growth, serving as the rationale for treatment of this patient with PKC412.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We are indebted to Rhoda Falkow for collection and processing of patient samples, and to Kathleen Dugan, Karen Mena, Marianne Rosamilia, and Debra Resta for administrative management of the PKC412 trial.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal