Key Points
BCR-ABL–specific CTLs may be obtained by stimulation with peptides derived from BCR-ABL junctional region and alternative splicing.
T-cell therapy with BCR-ABL–specific CTLs from healthy donors or patients mediates molecular or hematologic CR in patients with Ph+ ALL.
Abstract
Although the emergence of bone marrow (BM)–resident p190BCR-ABL–specific T lymphocytes has been correlated with hematologic and cytogenetic remissions in patients with Philadelphia chromosome–positive acute lymphoblastic leukemia (Ph+ ALL) undergoing maintenance tyrosine-kinase inhibitor treatment, little is known about the possibility of culturing these cells ex vivo and using them in T-cell therapy strategies. We investigated the feasibility of expanding/priming p190BCR-ABL–specific T cells in vitro by stimulation with dendritic cells pulsed with p190BCR-ABL peptides derived from the BCR-ABL junctional region and alternative splicing, and of adoptively administering them to patients with relapsed disease. We report on the feasibility of producing clinical-grade BCR-ABL–specific cytotoxic T lymphocytes (CTLs), endowed with antileukemia activity, from Ph+ ALL patients and healthy donors. We treated 3 patients with Ph+ ALL with autologous or allogeneic p190BCR-ABL–specific CTLs. No postinfusion toxicity was observed, except for a grade II skin graft-versus-host disease in the patient treated for hematologic relapse. All patients achieved a molecular or hematologic complete remission (CR) after T-cell therapy, upon emergence of p190BCR-ABL–specific T cells in the BM. Our results show that p190BCR-ABL–specific CTLs are capable of controlling treatment-refractory Ph+ ALL in vivo, and support the development of adoptive immunotherapeutic approaches with BCR-ABL CTLs in Ph+ ALL.
Introduction
Philadelphia chromosome–positive acute lymphoblastic leukemia (Ph+ ALL) was formerly burdened by uniformly poor prognosis.1 Widespread application of allogeneic hematopoietic stem cell (HSC) transplantation (alloHSCT) and advent of targeted BCR-ABL–specific tyrosine-kinase inhibitors (TKIs) have significantly improved complete response rates and disease-free survival.1,2 Despite these therapeutic advances, some unresolved issues remain, including the high prevalence in older patients,3 often ineligible for alloHSCT, and the extremely poor prognosis of relapsed Ph+ ALL, particularly following alloHSCT.1,4
Prolonged hematologic and cytogenetic remissions have been observed with imatinib mesylate (IM) alone, even in the presence of persisting levels of minimal residual disease (MRD).5-7 Our group was able to demonstrate that attainment of such clinical responses directly correlated with the emergence of BCR-ABL–specific T cells in the bone marrow (BM) and, to a lesser extent, in the peripheral blood of nonallografted Ph+ ALL patients undergoing postremission maintenance treatment with either IM or other second-generation TKIs.8,9 These observations extended previous evidence of functional leukemia-specific cellular immune responses developing in patients receiving IM, and possibly acting in synergy with IM to reach disease control,10,11 and represent the basis for a combined TKI and T-cell therapy approach to Ph+ ALL in elderly patients, or in patients relapsing after alloHSCT.
We report on the feasibility of inducing durable MRD clearance and leukemia control, without additional toxicity, by transfer of donor-derived or autologous cytotoxic T lymphocytes (CTLs) specific for the BCR-ABL fusion product in patients receiving TKI treatment of leukemia relapse after alloHSCT, or for molecular relapse in patients ineligible for alloHSCT. In addition, we describe the immunological parameters correlated with clinical response.
Study design
Patient 1 was a 61-year-old man in second molecular recurrence after matched unrelated donor (MUD) alloHSCT and unmanipulated donor lymphocyte infusions (DLIs). Patient 2 was a 30-year-old man diagnosed with Ph+ ALL with hyperleukocytosis and central nervous system (CNS) involvement, in third hematologic relapse (BM blast 66%, F317L mutation) after MUD-HSCT, DLI, and rescue therapy with Nilotinib. Patient 3 was a 62-year-old woman diagnosed with Ph+ ALL with CNS involvement, showing persistent molecular disease (last MRD before T-cell therapy 0.1% BCR-ABL/ABL) after induction, maintenance chemotherapy, and prolonged TKI treatment. She was not eligible for alloHSCT due to comorbidities. Details on patients’ clinical histories are reported in supplemental Methods (available on the Blood Web site).
Methods for p190BCR-ABL–specific CTL preparation and testing are detailed in supplemental Methods. The BCR-ABL peptide pool used in the stimulation procedure has been previously reported.8 BCR-ABL–specific treatment was administered on a compassionate basis according to bioethical committee approval.
MRD values were measured sequentially on BM mononuclear cell (MC) samples at baseline, and after each CTL infusion, by means of a previously described reverse transcriptase–polymerase chain reaction quantification of BCR-ABL transcripts.12 Immunological responses were evaluated sequentially by flow cytometry (supplemental Methods).8,13
Results and discussion
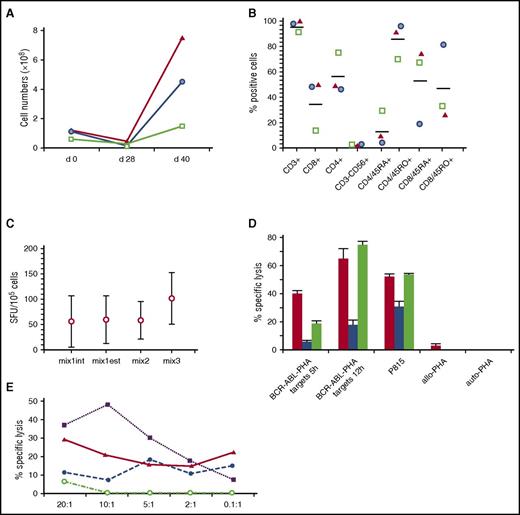
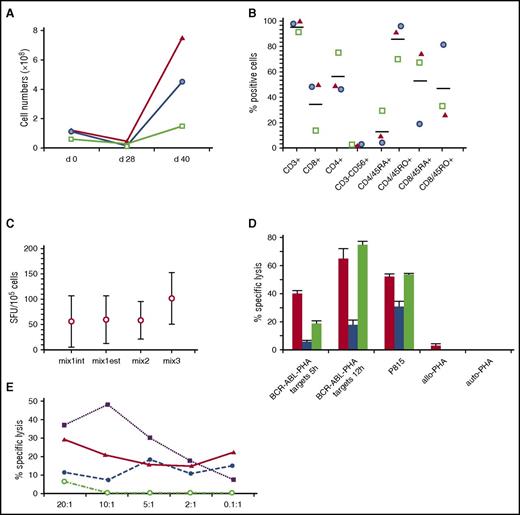
BCR-ABL–specific CTLs were expanded from peripheral blood MCs collected from the patient (case 3) or from HSC donors (cases 1-2) (Figure 1A). CTL lines were polyclonal (supplemental Figure 1) and included both CD3+CD8+ and CD3+CD4+ T cells (Figure 1B). Each CTL line produced interferon γ (IFNγ) in response to at least 1 BCR-ABL peptide pool (Figure 1C), and recognized autologous targets pulsed with BCR-ABL peptides and/or patient leukemia blasts (Figure 1D-E). Cytotoxic activity was likely mediated by both CD8+ and CD4+ T cells because we observed lysis in both 5-hour and 12-hour assays, the latter being HLA class II–restricted (supplemental Figure 2). Regarding specific activity against BCR-ABL peptides, we observed a broad response to the different peptide pools; of note, all CTLs recognized mix3 peptides, which included epitopes derived from products of BCR-ABL alternative splicing, confirming data on the suitability of these proteins as leukemia-specific antigens capable of eliciting an effective tumor-specific CTL response in vitro and also in vivo.14 As previously reported,15,16 by stimulating with dendritic cells pulsed with BCR-ABL peptides that included long peptides along with 9-mer epitopes, and using homeostatic cytokines in the culture process,17 we were able to prime leukemia-specific responses also in healthy donors.
Characteristics of the p190BCR-ABL–specific T cells used in the 3 patients. (A) T-cell expansion of p190BCR-ABL–specific T-cell lines achieved over a 40-day period based on cell counting using trypan blue exclusion (green square, patient 1; blue circle, patient 2; red triangle, patient 3). (B) Phenotype of p190BCR-ABL–specific T-cell lines, reported as the percentage of positive cells (green square, patient 1; blue circle, patient 2; red triangle, patient 3). (C) Response, measured as IFNγ production in a enzyme-linked immunospot (ELISPOT) assay, to the different peptide pools used in the activation/expansion process. Mix1int indicates 9- and 10-mer peptides spanning the internal p190 breakpoint region; Mix1est, 9- and 10-mer peptides spanning the external p190 breakpoint region; Mix3, 9-mer peptides derived from the alternative BCR-ABL splice variants. (D) Cytotoxic activity of T-cell lines, measured as the percentage of specific lysis at a effector-to-target (E:T) ratio of 5:1, against autologous phytohemagglutinin (PHA) blasts pulsed with p190BCR-ABL peptides (BCR-ABL-PHA targets, cytotoxicity measured at 5 hours and 12 hours, calculated after subtraction of background, consisting of cytotoxicity against autologous PHA blasts pulsed with irrelevant peptides), P815 cell line, nonpulsed PHA blasts from patients 1 and 2 (allo-PHA), nonpulsed autologous PHA blasts (auto-PHA) (red column, patient 1; blue column, patient 2; green column, patient 3). (E) Cytotoxicity profile of p190BCR-ABL–specific CTLs obtained from patient 2. The figure reports the percentage of specific lysis against patient ALL blasts (solid line and triangle), autologous PHA blasts pulsed with p190BCR-ABL peptides (dashed line and solid circle), P815 cell line (dotted line and solid squares), nonpulsed PHA blasts of the patient (dashed-dotted line and empty circles). The mean percentage of lysis of duplicate wells for 5 different E:T ratios is shown. SFU, spot-forming unit.
Characteristics of the p190BCR-ABL–specific T cells used in the 3 patients. (A) T-cell expansion of p190BCR-ABL–specific T-cell lines achieved over a 40-day period based on cell counting using trypan blue exclusion (green square, patient 1; blue circle, patient 2; red triangle, patient 3). (B) Phenotype of p190BCR-ABL–specific T-cell lines, reported as the percentage of positive cells (green square, patient 1; blue circle, patient 2; red triangle, patient 3). (C) Response, measured as IFNγ production in a enzyme-linked immunospot (ELISPOT) assay, to the different peptide pools used in the activation/expansion process. Mix1int indicates 9- and 10-mer peptides spanning the internal p190 breakpoint region; Mix1est, 9- and 10-mer peptides spanning the external p190 breakpoint region; Mix3, 9-mer peptides derived from the alternative BCR-ABL splice variants. (D) Cytotoxic activity of T-cell lines, measured as the percentage of specific lysis at a effector-to-target (E:T) ratio of 5:1, against autologous phytohemagglutinin (PHA) blasts pulsed with p190BCR-ABL peptides (BCR-ABL-PHA targets, cytotoxicity measured at 5 hours and 12 hours, calculated after subtraction of background, consisting of cytotoxicity against autologous PHA blasts pulsed with irrelevant peptides), P815 cell line, nonpulsed PHA blasts from patients 1 and 2 (allo-PHA), nonpulsed autologous PHA blasts (auto-PHA) (red column, patient 1; blue column, patient 2; green column, patient 3). (E) Cytotoxicity profile of p190BCR-ABL–specific CTLs obtained from patient 2. The figure reports the percentage of specific lysis against patient ALL blasts (solid line and triangle), autologous PHA blasts pulsed with p190BCR-ABL peptides (dashed line and solid circle), P815 cell line (dotted line and solid squares), nonpulsed PHA blasts of the patient (dashed-dotted line and empty circles). The mean percentage of lysis of duplicate wells for 5 different E:T ratios is shown. SFU, spot-forming unit.
Cells were administered in a dose-escalating manner on a monthly schedule. The 3 patients received a mean of 10 monthly infusions (range, 6-13). No immediate infusion-related adverse events were observed, and no grade 2-4 toxicities, including development of cytokine release syndrome, attributable to the T-cell infusions were recorded during follow-up. Patient 2, treated for hematologic relapse after alloHSCT, showed grade II skin graft-versus-host disease after administration of dose-level 2, successfully treated with topic steroids.
Molecular or hematologic complete remission (MCR or HCR) was obtained in all patients, associated with emergence of p190BCR-ABL–specific T-cells (Figure 2). Patient 1, who had detectable BCR-ABL transcripts in the BM prior to donor CTL treatment, achieved MCR after 4 weeks from the first CTL dose. He was maintained in MCR with monthly T-cell infusions, associated with IM treatment, for 12 months. After T-cell therapy discontinuation, he persists in MCR at 57-month follow-up (Figure 2A). Patient 3, who had persistent molecular disease and was ineligible for an alloHSCT, was treated with autologous p190BCR-ABL–specific CTLs. She achieved MCR at month +6 from cell therapy initiation (Figure 2C). In the patient with hematologic relapse (no. 2), we obtained HCR after 6 monthly p190BCR-ABL–specific CTL infusions at lower doses (0.1-0.5 × 106 T cell/kg), in combination with ponatinib treatment. Of note, in this last patient, the sole administration of p190BCR-ABL–specific CTLs, before the introduction of ponatinib, reduced BM blasts from 66% to 25%. Leukemia-specific T-cell responses were undetectable in the BM prior to CTL administration in all 3 patients. Progressive emergence of BM-resident, polyfunctional (cases 1, 3), or IFNγ-secreting (case 2) p190BCR-ABL–specific CD4+ and CD8+ T cells was associated with clearance of residual disease (Figure 2). Parallel epitope spreading to WT-1-antigen was observed in the patients’ BM (supplemental Figure 3).
Clinical and immunological responses to p190BCR-ABL–specific CTL infusion in 3 patients with molecular or hematological relapse of Ph+ ALL. Longitudinal data tracking MRD kinetics (left y-axis) and frequency of IFNγ-, interleukin 2 (IL-2)-, and tumor necrosis factor α (TNFα)-producing, p190BCR-ABL–specific, CD8+ and CD4+ T cells in the BM of patients, measured by flow cytometry and reported as the percentage of positive cells (right y-axis) are summarized in a single time-course graph for each patient. For each cytokine-producing T-cell subset, memory profiles are depicted over the related time points, defined as following: CD62L− CD45RA− (effector memory [EM]), CD62L+CD45RA− (central memory [CM]). On each patient’s graph, data on the percentage of donor chimerism, TKI treatment, and cell therapy (unmanipulated DLI; p190BCR-ABL–specific CTLs) timing and dose are also reported.
Clinical and immunological responses to p190BCR-ABL–specific CTL infusion in 3 patients with molecular or hematological relapse of Ph+ ALL. Longitudinal data tracking MRD kinetics (left y-axis) and frequency of IFNγ-, interleukin 2 (IL-2)-, and tumor necrosis factor α (TNFα)-producing, p190BCR-ABL–specific, CD8+ and CD4+ T cells in the BM of patients, measured by flow cytometry and reported as the percentage of positive cells (right y-axis) are summarized in a single time-course graph for each patient. For each cytokine-producing T-cell subset, memory profiles are depicted over the related time points, defined as following: CD62L− CD45RA− (effector memory [EM]), CD62L+CD45RA− (central memory [CM]). On each patient’s graph, data on the percentage of donor chimerism, TKI treatment, and cell therapy (unmanipulated DLI; p190BCR-ABL–specific CTLs) timing and dose are also reported.
Despite concerns on deleterious effects of TKIs on immune effectors, experimental and clinical evidence obtained in patients on long-term imatinib treatment suggests that the immune system is functional, and may be harnessed toward antitumor surveillance.18 After underscoring the role of p190BCR-ABL–specific T cells, emerging during TKI treatment, in controlling Ph+ ALL,8 we show the feasibility of expanding/priming these T cells from patients and HSCT donors, and demonstrate their excellent safety profile and in vivo antileukemic activity, in combination with TKI therapy.
In the last 5 years, impressive results have been obtained in the control of relapsed/refractory ALL by administration of T lymphocytes genetically modified to express chimeric antigen receptors (CARs) targeting B-cell–associated antigens.19-22 The increase in CAR–T-cell clinical efficacy, however, has been paralleled by the potential to induce severe adverse events, such as cytokine release syndrome, and on-target off-tumor toxicities.19,21,23 In this regard, BCR-ABL–specific CTLs may represent a valuable immunotherapeutic option for patients not amenable to or experiencing severe adverse events after CAR–T-cell infusion, or for patients with persistent levels of MRD during TKI maintenance treatment after HSCT.
Clinical trials using immune checkpoint inhibitors (ICIs) have shown enhancement of naturally occurring T-cell immunity against cancers, with promising therapeutic results.24 In perspective, combination treatments with ICIs or the bispecific T-cell antibody blinatumomab25 could allow the prevention of T-cell anergy and exhaustion after p190BCR-ABL–specific CTL infusions, thus improving persistence of antileukemia CTLs and restoring a durable immune surveillance against Ph+ ALL. At the same time, leukemia-specific T cells mediating tumor lysis may expose neoantigens, further potentiating the activity of ICIs.
The online version of the article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported by grants from the Ministero della Salute (Ricerca Finalizzata, GR-2010-2313609 [L.P.]; RF-2009-1548666 [P.C.]), the Associazione Italiana per la Ricerca sul Cancro (AIRC), Milan, Italy (IG 14797-2013) (M.L.), AIRC 5 × 1000 (MCO1007) (R.F.), and the Associazione Italiana Lotta alle Leucemie, Linfoma e Mieloma–Sezione ‘Luciano Pavarotti’–Modena-ONLUS (L.P. and F.F.); Fondazione Istituto di Ricovero e Cura a Carattere Scientifico Policlinico San Matteo (Ricerca Corrente 08069113 [P.C.]; 08045801/10 and 08045801/11 [M.Z.]).
Authorship
Contribution: P.C., S.B., G.R., P. Barozzi, M.L., and L.P. conceived and designed the study, analyzed results, and wrote the manuscript; S.B., I.G., A.G., G.Q., L.R., I.L., D.V., and A.P., produced and controlled CTL lines, processed samples, and executed experiments; F.F., M.M., P. Bresciani, A. Cuoghi, A.P., and E.C., provided clinical care, collected patient data, and commented on the manuscript; and R.M., A. Cuneo, L.I., T.T., F.N., R.F., and M.Z. supervised the study and critically revised the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Patrizia Comoli, Oncoematologia Pediatrica, Fondazione IRCCS Policlinico San Matteo, Viale Golgi 19, 27100 Pavia, Italy; e-mail: pcomoli@smatteo.pv.it.
References
Author notes
P.C., S.B., M.L., and L.P. contributed equally to this study.

![Figure 2. Clinical and immunological responses to p190BCR-ABL–specific CTL infusion in 3 patients with molecular or hematological relapse of Ph+ ALL. Longitudinal data tracking MRD kinetics (left y-axis) and frequency of IFNγ-, interleukin 2 (IL-2)-, and tumor necrosis factor α (TNFα)-producing, p190BCR-ABL–specific, CD8+ and CD4+ T cells in the BM of patients, measured by flow cytometry and reported as the percentage of positive cells (right y-axis) are summarized in a single time-course graph for each patient. For each cytokine-producing T-cell subset, memory profiles are depicted over the related time points, defined as following: CD62L− CD45RA− (effector memory [EM]), CD62L+CD45RA− (central memory [CM]). On each patient’s graph, data on the percentage of donor chimerism, TKI treatment, and cell therapy (unmanipulated DLI; p190BCR-ABL–specific CTLs) timing and dose are also reported.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/129/5/10.1182_blood-2016-07-731091/4/m_blood731091f2.jpeg?Expires=1768175594&Signature=zAzbG4mM2DBJt1qqqghOm~Di-N80bVqM-hHzxyxZfwJ13-APTFVjlTuRYeUcD2E4qaFomFPW64qMnPlL2nViO9T4S3T8mJnpUU0IHE-RmZh8cRpYlrt5l2U2kAlBprb3B9TcMbIYTFaM7M~6hfMAwNCRupmk3Re5cppeRRxzZE9dE3IdscyVXEhxdhqwyFYjrhFDEbjaj0lsXtWuMmb5RmKw1VWicVLQASeo0~KDCJPr2mUbA7vUYHTli0QuYu1Qpf6vKIUK15SjwAlqpH-RBrcqX6wJ7vKKsJ84h0VHZ1V3i-Oal1KXlolXjlNurnqfNtRZNqSL0eRs0X-WXXkNEA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)

![Figure 2. Clinical and immunological responses to p190BCR-ABL–specific CTL infusion in 3 patients with molecular or hematological relapse of Ph+ ALL. Longitudinal data tracking MRD kinetics (left y-axis) and frequency of IFNγ-, interleukin 2 (IL-2)-, and tumor necrosis factor α (TNFα)-producing, p190BCR-ABL–specific, CD8+ and CD4+ T cells in the BM of patients, measured by flow cytometry and reported as the percentage of positive cells (right y-axis) are summarized in a single time-course graph for each patient. For each cytokine-producing T-cell subset, memory profiles are depicted over the related time points, defined as following: CD62L− CD45RA− (effector memory [EM]), CD62L+CD45RA− (central memory [CM]). On each patient’s graph, data on the percentage of donor chimerism, TKI treatment, and cell therapy (unmanipulated DLI; p190BCR-ABL–specific CTLs) timing and dose are also reported.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/129/5/10.1182_blood-2016-07-731091/4/m_blood731091f2.jpeg?Expires=1768175595&Signature=pXarNYGPMKxNCaumAYvBlMiRsLtej8KLvmoznjVEEi0OHUNe38tdFyZ5pYwI1hS5HTjAWBc2tg8pzIVdIZ4-3FfY6gS2xK2W~Ss6Dhfa~HzTfjzywzRtD5nOBJxa4xioRqMSGQwWz45Tp6NpZ7OX19H-OY4DEq7fw8JupNEB9lf8B2DgGSjY3tPoZygPCDHX4nXi~MzgtuSbMU0RSu3L7KYBF3c2MJWmL0YN96wuGfnFOfubjEKxaPj10r9jGRckDQIN26oxFDvLO3pVrHr4omFkB4mZScsrbbAljrCQd~Qyk-JltNI8zgpbDYkw1VEHQ8vWs~ooEXFk4GqOnPdQ8g__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)