Abstract
Graft-versus-host disease (GVHD), the primary cause of non-relapse mortality (NRM) following allogeneic hematopoietic stem cell transplantation, does not always respond to treatment with high dose systemic corticosteroids. We have recently shown that a combination of three biomarkers (TNFR1, ST2, and REG3α) measured at onset of GVHD can predict day 28 response to treatment and 6-month NRM (Levine, Lancet Haem, 2015). Our goal in the current study was to determine if the same biomarker-based Ann Arbor GVHD algorithm can alsopredict treatment response andmortality whenapplied after one week of systemic corticosteroid treatment.
The study population consisted of 378 patients (pts) with acute GVHD from 11 centers in the Mount Sinai Acute GVHD International Consortium. All pts were treated with systemic steroids and provided a plasma or serum sample obtained after one week of treatment (±3 days). The median starting dose of systemic steroids for Grade II-IV GVHD was 2.0 mg/kg/day and for Grade I was 1.0 mg/kg/day, after which treatment varied. Patients were divided into test (n=236) and validation (n=142) cohorts. We applied the Ann Arbor GVHD algorithm to concentrations of TNFR1, ST2, and REG3α measured after one week of treatment to generate a predicted probability of 6-month NRM, which we term the treatment score (TS). We employed unsupervised k-medoidclustering to partition TS values from the test cohort into two groups (high and low). This unbiased approach identified a high score group made up of 25% of pts (n=58) in the test cohort.
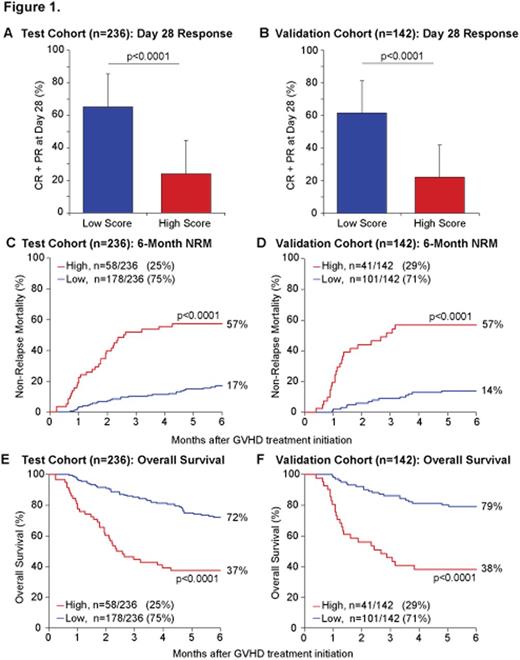
We observed that the day 28 response rate (complete, CR + partial, PR) was significantly lower in pts with high scores compared to low scores in the test cohort (24% vs 65%, p<0.0001) (Fig 1A). Analysis of the validation cohort using the same TS definitions showed similar differences in response rates (22% vs 61%, p<0.0001) (Fig 1B). Further, nearly four times as many pts with high scores in both cohorts died within 6 months from non-relapse causes compared to pts with low scores (test: 57% vs 17%, p<0.0001; validation: 57% vs 14%, p<0.0001) (Fig 1C/D). As expected, the majority of non-relapse deaths in pts treated for GVHD were directly attributable to GVHD (test: 95%; validation: 89%). Relapse rates for high and low score pts were similar (data not shown), and thus pts with a high TS experienced significantly worse overall survival in both cohorts (test: 37% vs 72%, p<0.0001; validation: 38% vs 79%, p<0.0001) (Fig 1E/F).
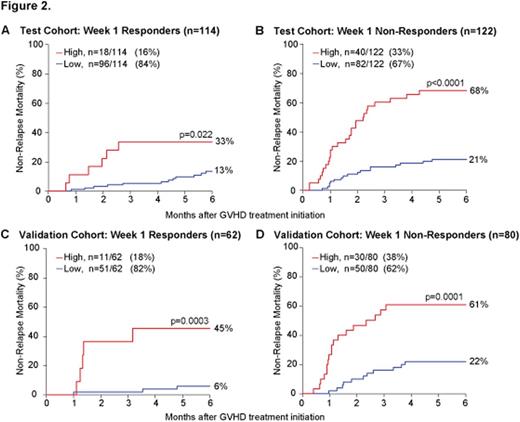
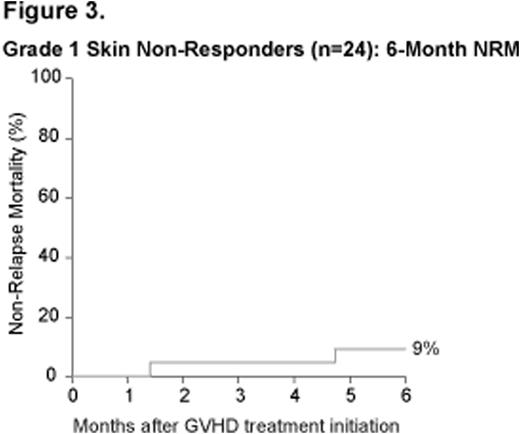
Approximately half of the pts in each cohort (test: 48%; validation: 44%) responded (CR+PR) to the first week of steroids and these ptshad significantly lower 6-month NRM than non-responders (NR) (test: 17% vs 36%, p=0.0002; validation: 13% vs 36%, p=0.0014). Yet the TS continued to stratify mortality risk independently of clinical response. In the test cohort, pts with a high score comprised 16% of all early responders and experienced more than twice the NRM of early responders with a low score (33% vs 13%, p=0.022) (Fig 2A). Conversely, test cohort pts who did not respond by day 7, but had a low score, fared much better than non-responders with a high score (NRM 21% vs 68%, p<0.0001) (Fig 2B). Two thirds of early non-responders comprised this more favorable group. These highly significant results reproduced in the independent validation cohort in similar proportions (CR+PR: 45% vs 6%, p=0.0003; NR: 61% vs 22%, p=0.0001) (Fig 2C/D). Finally, a subset analysis revealed that pts classified as NR after one week of steroids due to isolated, yet persistent, grade I skin GVHD (24/378, 6%) overwhelmingly had low treatment scores (22/24, 92%) and experienced rates of NRM (9%) comparable to responders with low scores, thus forming a distinct, albeit small, subset of pts with non-responsive GVHD that fares particularly well (Fig 3).
In conclusion, a treatment score based on three GVHD biomarkers measured after one week of steroids stratifies pts into two groups with distinct risks for treatment failure and 6-month NRM. It is particularly noteworthy that the TS identifies two subsets of pts with steroid refractory (SR) GVHD who have highly different outcomes (Fig 2B/D). The much larger group, approximately two thirds of all SR pts, may not need the same degree of treatment escalation as is traditional for clinical non-response, and thus overtreatment might be avoided. Because the TSis measured at a common decision making time point, it may prove useful to guide risk-adapted therapy.
Mielke:Novartis: Consultancy; MSD: Consultancy, Other: Travel grants; Celgene: Other: Travel grants, Speakers Bureau; Gilead: Other: Travel grants; JAZZ Pharma: Speakers Bureau. Kroeger:Novartis: Honoraria, Research Funding. Chen:Incyte Corporation: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Research Funding. Jagasia:Therakos: Consultancy. Kitko:Therakos: Honoraria, Speakers Bureau. Ferrara:Viracor: Patents & Royalties: GVHD biomarker patent. Levine:Viracor: Patents & Royalties: GVHD biomarker patent.
Author notes
Asterisk with author names denotes non-ASH members.