Several studies suggest an implication of transforming growth factor-β1 (TGF-β1) in the promotion of myelofibrosis associated with hematopoietic malignancies, but the involvement of this cytokine is not fully investigated. To test directly the impact of TGF-β1 in the pathogenesis of myelofibrosis, bone marrow stem cells from homozygous TGF-β1 null (TGF-β1−/−) and wild-type (WT) littermates were infected with a retrovirus encoding the murine thrombopoietin (TPO) protein and engrafted into lethally irradiated wild-type hosts for long-term reconstitution. Over the 4 months of follow-up, TPO levels in plasma were markedly elevated in both groups of mice, and animals typically developed a myeloproliferative syndrome characterized by thrombocytosis, leukocytosis, splenomegaly, increased numbers of progenitors in blood, and extramedullary hematopoiesis. Severe fibrosis was observed in spleen and marrow from all the mice engrafted with WT cells. In contrast, none of the mice repopulated with TGF-β1−/− cells (chimerism > 70%) showed deposition of reticulin fibers at any time during the follow-up. In accordance with the development of fibrosis, latent TGF-β1 levels in plasma and extracellular fluid of the spleen from mice engrafted with WT cells were increased 6-fold and 4-fold, respectively, over levels found in normal hosts, whereas no increase over baseline levels could be demonstrated in animals undergoing transplantation with TGF-β1−/− cells. These data provide evidence that TGF-β1 produced by hematopoietic cells is pivotal for the pathogenesis of myelofibrosis that develops in mice with TPO overexpression.
Introduction
Myelofibrosis is a prominent clinical feature of several hematopoietic disorders1 and particularly in idiopathic myelofibrosis.2,3 It occurs as a cytokine-mediated secondary response to a clonal malignant event originating in a pluripotent stem cell4,5 and is characterized by excessive deposits of extracellular matrix proteins, neoangiogenesis and, in severe cases, osteosclerosis.6 In vivo and in vitro studies have involved several cytokines, such as transforming growth factor-β1 (TGF-β1), platelet-derived growth factor (PDGF), or basic fibroblast growth factor (bFGF), in the development of myelofibrosis.7-10 Among these growth factors, the pleiotropic cytokine TGF-β1 has received attention because TGF-β1 potently stimulates fibroblasts to produce extracellular matrix and cell adhesion proteins11-14 and enhances the expression of proteases that inhibit enzymes involved in the degradation of the extracellular matrix.15 TGF-β1 is secreted by numerous cell types in the body, but several lines of evidence have suggested a crucial role of megakaryocytes in myelofibrosis induction.16 First, TGF-β1 is the most abundant isoform found in megakaryocytes and platelets. Second, on marrow biopsies from patients with idiopathic myelofibrosis, megakaryocytes are often found in close proximity or surrounded by reticulin fibers6 and, third, acute myelofibrosis is often associated with megakaryoblastic leukemia.17 18Despite this circumstantial evidence, it remains unclear whether TGF-β1 alone promotes myelofibrosis or whether it acts in concert with others fibrogenic cytokines to induce the aberrant stromal reaction. Such a demonstration has been hampered by the lack of an experimental model allowing us to address this issue.
Over the past years, animal models that recapitulate the clinical features of human idiopathic myelofibrosis have been reported. In vivo administration of suprapharmacologic doses of thrombopoietin (TPO), the physiological regulator of platelet production, resulted in megakaryocyte hyperplasia associated with a densification of the reticulin network.19,20 Mice permanently exposed to high doses of TPO delivered through retroviral infection of hematopoietic stem cells developed a myeloproliferative syndrome with a prominent proliferation of megakaryocytes and leukocytes, extramedullary hematopoiesis and, invariably, splenic and medullary fibrosis and osteosclerosis.21-23 In these experimental models, it has been hypothesized that TGF-β1 had an important role in the development of myelofibrosis because elevated levels were detected in plasma, platelet extracts, and marrow fluids at the time of myelofibrosis development, which gradually decreased with fibrosis normalization.20 However, increased levels of PDGF were also demonstrated in plasma from TPO-overexpressing mice,22 suggesting that both TGF-β1 and PDGF, or possibly other cytokines, could influence the fibrogenic and osteogenic responses.
To clarify further the pathological effect of TGF-β1 in mice with megakaryocyte hyperplasia, we repopulated over the long term lethally irradiated wild-type hosts with either TGF-β1−/−24 or wild-type (WT) hematopoietic stem cells engineered to overexpress the murine TPO protein via a retroviral-mediated gene transfer. TPO elevation in plasma was similar in both groups of mice, and all animals invariably developed a myeloproliferative syndrome. However, although myelofibrosis occurred in all the mice engrafted with WT cells, no deposition of reticulin was seen in mice reconstituted with a majority of TGF-β1−/− cells. Our data provide a direct demonstration that TGF-β1 released by hematopoietic cells plays a major impact in the pathophysiology of myelofibrosis.
Materials and methods
Mice
Heterozygote TGF-β1 breeders with a mixed Sv129 × CF-1 genetic background were provided by T. Doetschman (Cincinatti, OH).25 Mice were bred in our animal facility under specific pathogen-free conditions. Because 100% of homozygote TGF-β1−/− animals die before weaning,25experiments were performed with cells obtained from 14- to 16-day-old male and female TGF-β1−/− or WT littermates. Lethally irradiated (10 Gy delivered by an X-ray apparatus) male and female WT mice (8-10 weeks old) were used as hosts. For engraftment, irradiated hosts were injected via the retro-orbital sinus with 4 × 106 to 6 × 106 lineage-negative (Lin−) cells exposed to the MIGR-TPO virus.
PCR genotyping
DNA was extracted from distal tail segments from 12-day-old pups using standard techniques. For genotyping, 3 primers were used: primer A: 5′-GAGAAGAACTGCTGTCG-3′; primer B: 5′-GTGTCCAGGCTCCAAATATAGG-3′; and primer C: 5′-GCCGAGAAAGTATCCATCAT-3′. Primers A and B amplify a 142-bp product from the WT allele; primers B and C amplify a 500-bp product from the targeted allele. Polymerase chain reaction (PCR) conditions were as previously described.25
Generation of the retrovirus
A full-length murine TPO cDNA was cloned upstream from the IRES of the MSCV-IRES-GFP (MIGR) (murine stem cell virus–internal ribosome entry site–green fluorescent protein) retrovirus.26 Infectious defective virions were transiently produced by transfection of the 293 EBNA cell line with 3 plasmids: pCMV gag-pol, pCMV-VSV-G (vesicular stomatite virus envelope glycoprotein) (both provided by J. Morgenstein, Cambridge, MA), and the MIGR-TPO-GFP construct. Briefly, 293 EBNA cells were seeded at a concentration of 106 cells per well in 6-wells plates (Costar, Dutscher, France). The next day, 0.5 μg of each plasmid was cotranfected using Exgen reagent (Euromedex, Mundolshein, France) according to the manufacturer's recommendations. Supernatants were collected after 48, 72, and 96 hours and concentrated 20-fold over an amicon membrane (Centricon Plus-80; Millipore, St-Quentin en Yvelines, France). Viral titers were determined by limiting dilution assay on NIH 3T3 cells. GFP fluorescence was analyzed by flow cytometry. Virus stocks containing 107 infectious particles per milliliter or more were used to infect the Lin− cell populations isolated from donors' marrow.
Marrow cell preparation and infection
Single-cell suspensions prepared from femurs and tibiae were enriched for progenitors by immunomagnetic selection using a cocktail of CD45/B220 (clone RA3-6B2), CD4 (clone GK.1.5), CD5 (clone 53-7.3), Ly-6/GR1 (clone RB6-8C5), CD11/Mac-1 (clone M1/70), and TER 119 monoclonal antibodies (Pharmigen, San Diego, CA). Cells were incubated with immunomagnetic beads (Dynabeads M-450; Oslo, Norway) at a bead-cell ratio of approximately 4:1. To check for purity, the Lin− fraction was stained with a sheep antirat κ light chain phycoerythrin-conjugated immunoglobulin G (IgG) and analyzed by flow cytometry. Routinely, purity ranged from 80% to 90%.
The Lin− fraction obtained from WT mice was prestimulated during 24 hours in α-minimal essential medium (Sigma Aldrich, Saint Quentin Fallavier, France) containing 10% heat-inactivated fetal bovine serum (FBS) and 5 recombinant cytokines (mu–FLT3-L, 20 ng/mL; mu-SCF, 25 ng/mL; mu–IL-3, 100 U/mL; mu-TPO, 10 ng/mL; mu–IL-6, 10 ng/mL). All cytokines were purchased from R&D (Oxon, United Kingdom). The Lin− fraction obtained from TGF-β1−/−mice was not subjected to prestimulation. Cells (1 × 106) were incubated with 1 mL MIGR-TPO virus in the presence of the 5 cytokines for 24 hours and 4 μg/mL Polybrene (Sigma, St Louis, MO). Cells were centrifuged and incubated for another 24 hours in fresh virus stock, fresh cytokines, and Polybrene. An aliquot was used for colony-forming cell (CFC) assays; the remainder were inoculated into lethally irradiated hosts in a ratio of 3 donors per 1 recipient.
In vitro clonogenic progenitor assay
The frequency of CFCs in the Lin− fraction immediately after infection in spleen, marrow, and blood of engrafted animals was assessed in methylcellulose culture (Myelocult M3134; Stem Cell Technologies, Vancouver, BC) containing 20% FBS and recombinant murine interleukin-3 (mu–IL-3) (100 U/mL), mu-TPO (10 ng/mL), murine stem cell factor (mu-SCF) (50 ng/mL), and human erythropoietin (hu-EPO) (2 U/mL). Seeding densities were 5000 cells per milliliter for the Lin− fraction or 1 × 105 cells per milliliter for spleen, marrow, and blood mononuclear cells. All cultures were plated in triplicate and incubated at 37°C in a humidified incubator containing 5% CO2 in air. Colonies (> 50 cells) were scored at day 7 under an inverted microscope and randomly picked for PCR analysis.
Analysis of engraftment and gene transfer
To evaluate chimerism in hosts engrafted with TGF-β1−/− cells, CFC-derived colonies from the marrow were analyzed by PCR using the TGF-β1 primers indicated above. To assess gene transfer efficiency, marrow-derived colonies from mice undergoing transplantation with TGF-β1−/− or WT cells were analyzed by PCR to detect the integrated retroviral sequence. Primers corresponding to the TPO cDNA were as follows: sense 5′-ACTTTAGCCTGGAGAATGGAAA-3′ and antisense 5′-CCAGGAGTAATCTTGACTCTGA-3′ allowing the amplification of a 499-bp product. Actin was used as an internal control: sense 5′-GTACCACAGGCATTGTGATG-3′ and antisense 5′-GCAACATAGCACAGCTTCTC-3′. Thirty colonies were individually deposited into Eppendorf tubes containing 10 μL lysis buffer (10 mmol/L Tris [tris(hydroxymethyl)aminomethane] hydrochloride [pH 8.3], 2 mmol/L MgCl2, 50 mmol/L KCl, 0.45% Tween 20) and 1 mg/mL proteinase K. Samples that failed to show a PCR product with actin were not included in the calculation of chimerism or gene transfer efficiency.
Hematology, histopathology, and immunohistochemistry
Retro-orbital venous blood was sampled in citrated tubes. Numbers of nucleated cells and platelets, hematocrit values, and differential cell counts were determined with a Coulter calibrated for mouse blood (MS9, Schloessing Melet, Cergy-Pontoise, France). Platelet-poor plasma (PPP) was prepared and stored at −20°C for determination of TPO and TGF-β1 levels. Tissues were fixed in Glyo-Fixx fixative (CML, Nemours, France) and embedded in paraffin. Sections (4-5 μm) were stained with hematoxylin and eosin, periodic acid–Schiff, and Giemsa for overall cytology. Reticulin fibers were revealed by silver staining according to Gordon-Sweet. Immunohistochemistry on spleen sections was performed with an anti–TGF-β monoclonal antibody (MAB 1835, clone 1D11, R&D Systems) used at 150 mg/mL. Antibody reactivity was revealed with streptavidin APAP (alkaline phosphatase antialkaline phosphatase) and Fast Red TR as a chromogene (DAKO, Trappes, France).
TPO and TGF-β1 quantification
TPO levels in PPP were determined with an enzyme-linked immunosorbent assay (ELISA) (murine TPO Quantikine Kit; R&D Systems) according to the manufacturer's instructions. The sensitivity limit of the assay was 62.5 pg/mL. The human TGF-β1 immunoassay (R&D Systems), which detects only active forms of TGF-β1, was used for determination of TGF-β1 levels in PPP, platelet extracts, and extracellular fluid of spleens. Samples were prepared with a slight modification of the reported procedure.20 Briefly, 500 μL whole blood was collected on 500 μL citrated Hanks buffered saline solution (HBSS, Sigma Aldrich) and centrifuged at 200g to prepared platelet-rich plasma. Platelets were pelleted (2000g for 10 minutes), suspended in 200 μL HBSS, and counted. An aliquot containing 4 × 108 platelets was suspended in a final volume of 500 μL HBSS and subjected to 3 cycles of freeze-thawing. Samples were centrifuged (12 000g for 5 minutes), and platelet extracts were collected. An aliquot of the spleen (100 mg) was gently disrupted in 1 mL HBSS, samples were centrifuged (1000g for 10 minutes), and supernatants were collected. All samples were assayed before (active TGF-β1) and after acidification (latent forms). For acidification, the protocol recommended by manufacturers was followed. The sensitivity of the assay was 62.5 pg/mL.
Statistical analysis
The results are presented as mean ± SD. The data were analyzed with the 2-tailed Student t test.
Results
Engraftment with virus-infected TGF-β1−/− and TGF-β1+/+ marrow cells
To assess the contribution of TGF-β1 in myelofibrosis, Lin− cells from TGF-β1−/− pups and their WT littermates were infected with the MIGR-TPO retrovirus and engrafted into lethally irradiated wild-type hosts for long-term reconstitution. Whatever the donor genotype, recovery of the Lin− fraction was routinely around 5% with a mean purity of 80% (78%-90%; n = 12). To ensure efficient transduction in primitive hematopoietic stem cells, the Lin− fraction from WT donors was prestimulated in vitro during 24 hours before being exposed during 48 hours to the virus at a multiplicity of infection of 20. Because TGF-β1 negatively controls the cell cycle of primitive hematopoietic stem cells (HSCs),27 28 we omitted the prestimulation step in the TGF-β1−/− group. At the end of the infection protocol, the cellular amplification was 1.5- to 2-fold in the 2 groups, and the mean CFC numbers per 5000 cells plated was comparable (153 ± 73 in WT vs 122 ± 19 in TGF-β1−/−; n = 5, respectively). Transduction efficiencies varied between experiments (11%-36%). These variations were not related to the cell genotype but merely due to the different batches of virus used, which were freshly prepared for each experiment. Given the low virus integration level and to ascertain a high chimerism in the long term, each recipient was injected with 4 × 106 to 6 × 106 cells corresponding to the Lin− fraction isolated from 3 donors. With one exception due to a splenic rupture, all recipients undergoing transplantation survived longer than 6 months.
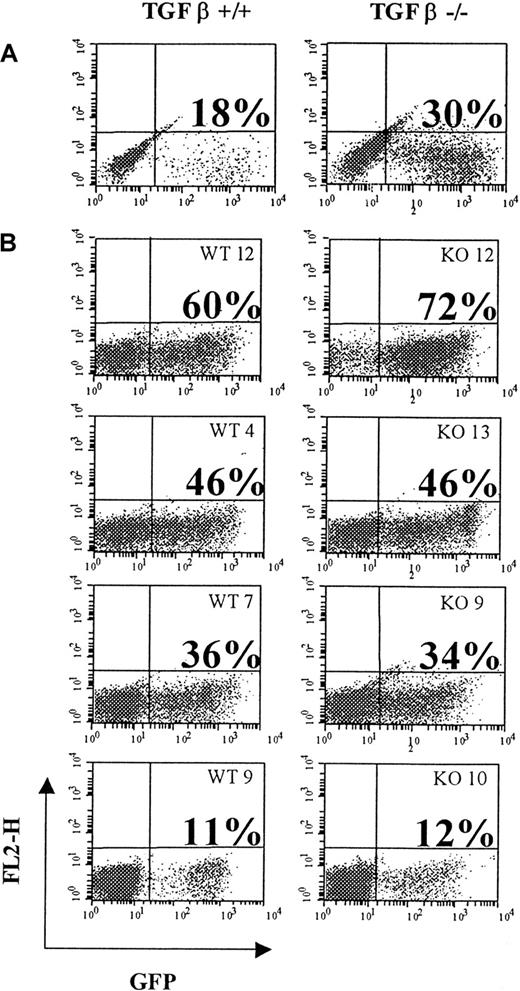
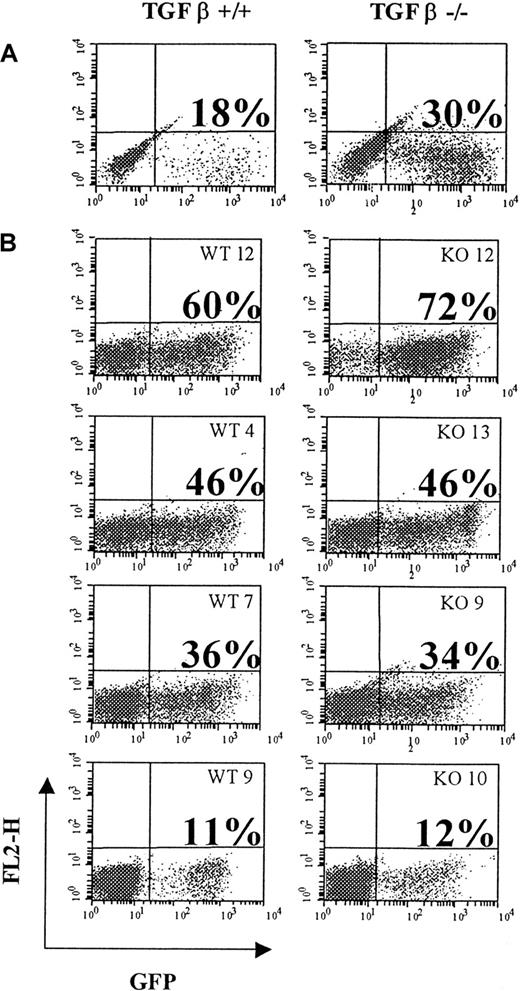
Levels of engraftment were analyzed by tracking expression of the GFP reporter gene by fluorescence-activated cell sorting (FACS) in mature nucleated blood cells. All mice displayed GFP fluorescence in leukocytes. However, the percentage of GFP+ cells was variable between each individual, ranging from 10% to 96% of GFP marking at any time. These variations were not consistent with the degree of transduction at the end of the infection protocol and were not related to the cell genotype. As illustrated in Figure1 (2 representative experiments), of 4 mice engrafted with a pool of WT cells showing an initial transduction level of 18% and 4 mice engrafted with a pool of TGF-β1−/− cells with an initial transduction level of 30%, one mouse in each group (WT12 and KO12) showed 60% and 72% GFP+ leukocytes in blood, respectively; WT9 and KO10 had about 10%, whereas the others displayed intermediate levels with 46% GFP+ (WT4 and KO13) or 36% GFP+ leukocytes for WT7 and KO9. Nevertheless, mice showing the highest percentage of GFP+ cells at week 6 remained relatively stable over time, whereas no significant increase in GFP expression was noted in animals with low expression (data not shown). To more precisely evaluate the percentage of transduced progenitor cells over time, marrow cells were seeded in methylcellulose at time of killing and CFC-derived colonies were subjected to PCR with primers amplifying the viral TPO cDNA. As seen for the analysis of GFP+ leukocytes, the percentage of virus-transduced CFCs in marrow was variable, with high or low levels of infection detected in both groups (Table 1). However, the largest variations were observed in the TGF-β1−/−group, with some animals demonstrating up to 96% of infected progenitor cells, while others were below 5%. One animal (KO7) showing no infected progenitors 4 months after the graft was discarded from the data. In some mice, the percentage of virus-infected CFCs detected at week 6 or 16 was higher than immediately after infection, suggesting that transduction could be more efficient in short-term and possibly in long-term repopulating cells than in CFC.
Flow cytometry profile showing green fluorescent protein (GFP)–positive cells.
Shown at the end of the infection protocol (A) and in peripheral blood leukocytes (B) of individual mice engrafted with virus-infected cells at week 6 after transplantation. WT transplant (left panels) or TGF-β1−/− transplants (right panels). Percent of positive cells is given above each corresponding profile.
Flow cytometry profile showing green fluorescent protein (GFP)–positive cells.
Shown at the end of the infection protocol (A) and in peripheral blood leukocytes (B) of individual mice engrafted with virus-infected cells at week 6 after transplantation. WT transplant (left panels) or TGF-β1−/− transplants (right panels). Percent of positive cells is given above each corresponding profile.
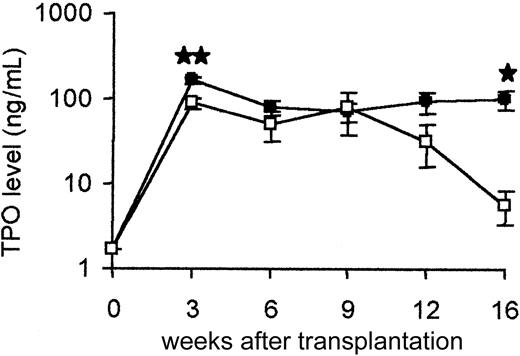
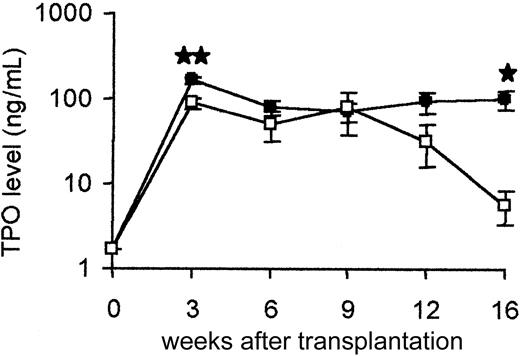
TPO levels in plasma
Baseline levels measured in plasma from normal adult wild-type mice from this colony were at least 1.7 ± 0.2 ng/mL (n = 10). In all mice undergoing transplantation, TPO levels were sharply increased at week 3, with values reaching up to 100 ng/mL. This elevation was sustained during 9 weeks in both groups (Figure2). However, although values remained high in animals undergoing transplantation with WT cells over time, TPO levels progressively decreased in hosts undergoing transplantation with TGF-β1−/− donor cells.
TPO quantification in plasma.
Each point is the mean ± SD of 12 to 14 animals, with the exception that only 6 TGF-β1−/− animals were analyzed at week 16. ● represents TGF-β1+/+ (WT) transplant; ■, TGF-β1−/− (–/–) transplant. Results of statistical analysis with the 2-tailed Student t test: WT versus TGF-β1−/−, ★P < .05 and★★P < .001.
TPO quantification in plasma.
Each point is the mean ± SD of 12 to 14 animals, with the exception that only 6 TGF-β1−/− animals were analyzed at week 16. ● represents TGF-β1+/+ (WT) transplant; ■, TGF-β1−/− (–/–) transplant. Results of statistical analysis with the 2-tailed Student t test: WT versus TGF-β1−/−, ★P < .05 and★★P < .001.
Hematologic analysis
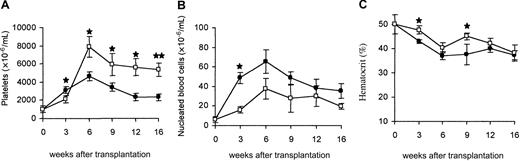
In accordance with TPO elevation in circulation, platelet numbers in mice reconstituted with WT cells increased over 6 weeks, achieving values 4-fold higher than normal controls (4.8 × 106/μL ± 0.6 × 106/μL vs 1.1 × 106/μL ± 0.2 × 106/μL, respectively). Thereafter, a progressive drop occurred, but all mice remained thrombocythemic with numbers 2-fold above normal. No correlation between TPO levels and platelet numbers was observed. The elevation in platelet numbers in mice engrafted with TGF-β1−/− cells was even more striking, with animals maintaining values above 6 × 106/μL at 4 months after transplantation (Figure 3A). The excessive platelet production is likely related to the inhibitory effect of TGF-β1 on thrombocytopoiesis.29,30 Mononuclear blood cells were increased in both groups of mice (Figure 3B) due to a striking increment in mature polymorphonuclear neutrophils in association with immature myeloid precursor cells (data not shown). However, leukocyte numbers were consistently more elevated in mice reconstituted with WT cells, suggesting a stimulatory effect of TGF-β1 on granulopoiesis.31 Mice in both groups became progressively anemic (Figure 3C). These data indicate that overproduction of TPO in hosts repopulated with WT or TGF-β1−/− hematopoietic cells resulted in a comparable myeloproliferative syndrome.
Blood parameters.
Evolution in platelet numbers (A), leukocyte numbers (B), and hematocrit (C) in mice undergoing transplantation with WT (●) or TGF-β1−/− (■) virus-infected hematopoietic cells. Each point represents the mean ± SD of 12 to 14 animals, with the exception that only 6 TGF-β1−/− animals were analyzed at week 16. Results of statistical analysis with the 2-tailed Student t test: WT versus TGF-β1−/−,★P < .05 and★★P < .001.
Blood parameters.
Evolution in platelet numbers (A), leukocyte numbers (B), and hematocrit (C) in mice undergoing transplantation with WT (●) or TGF-β1−/− (■) virus-infected hematopoietic cells. Each point represents the mean ± SD of 12 to 14 animals, with the exception that only 6 TGF-β1−/− animals were analyzed at week 16. Results of statistical analysis with the 2-tailed Student t test: WT versus TGF-β1−/−,★P < .05 and★★P < .001.
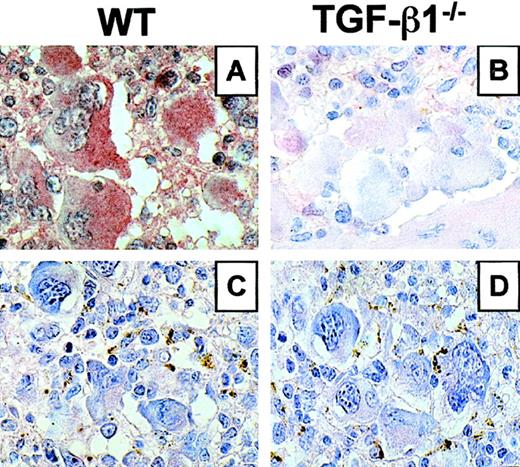
Chimerism of mice repopulated with TGF-β1−/−transduced cells
To ascertain that hematopoietic reconstitution of WT hosts engrafted with TGF-β1−/− cells was donor derived in the long term, we performed a PCR analysis for the neo gene indicative of TGF-β1 mutated allele on CFC-derived colonies from the marrow. Except for one animal (KO7), 64% to 100% of CFCs were positive for the neo gene at week 16 (Table2). In addition, when immunocytochemistry was carried out on spleen sections with an anti–TGF-β antibody, immunolabeling showed a strong positivity in megakaryocytes and granulocytes from mice repopulated with WT cells (Figure4A), whereas no reactivity was seen in mice repopulated with TGF-β1−/− hematopoietic cells (Figure 4B). No immunostaining was observed when the anti–TGF-β antibody was omitted (Figure 4C-D). These results demonstrate that TGF-β1−/− stem cells were able to ensure a high level and long-term engraftment in WT irradiated hosts.
TGF-β expression in spleen section from mice engrafted with WT or TGF-β1−/−virus–infected hematopoietic cells.
Immunocytochemistry using a TGF-β–specific antibody (A,B). Immunostaining specificity was checked by omitting the primary antibody (C,D). Representative sections are shown at 3 months after transplantation. (A) Mouse engrafted with WT cells showing strong positivity in MK and granulocytes. (B) Mouse engrafted with TGF-β1−/− cells showing no immunoreactivity. (C,D) No immunostaining was revealed when the primary antibody was omitted. Original magnification, × 600 for all panels.
TGF-β expression in spleen section from mice engrafted with WT or TGF-β1−/−virus–infected hematopoietic cells.
Immunocytochemistry using a TGF-β–specific antibody (A,B). Immunostaining specificity was checked by omitting the primary antibody (C,D). Representative sections are shown at 3 months after transplantation. (A) Mouse engrafted with WT cells showing strong positivity in MK and granulocytes. (B) Mouse engrafted with TGF-β1−/− cells showing no immunoreactivity. (C,D) No immunostaining was revealed when the primary antibody was omitted. Original magnification, × 600 for all panels.
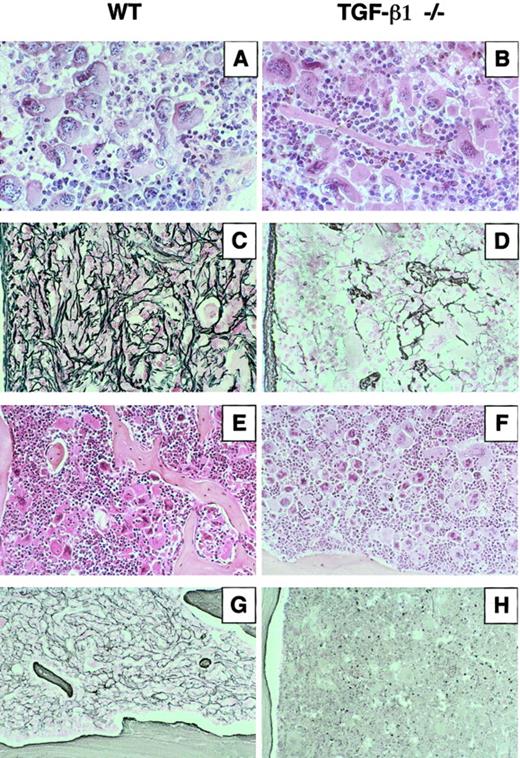
Pathological changes in tissues
Mice were humanely killed at week 6 and 16 after transplantation to examine the pathological changes. All animals displayed a splenomegaly at week 6. At week 16, spleen weights were decreased but remained 4-fold above normal in mice engrafted with WT cells, whereas they were slightly above normal in the TGF-β1−/− group (Table3). Irrespective of the transplant, the marrow cellularity remained lower than in the controls at all times studied. At week 6, numbers of CFCs were highly augmented in spleen and blood (20-fold and 1000-fold, respectively) and 2-fold decreased in the marrow, but no major difference was seen between the 2 groups (Table3). After 4 months, although spleen sizes were augmented in the WT group, the cellularity was quite low (1.28 × 108 ± 0.65 × 108 cells per spleen compared with 1.75 × 108 ± 0.56 × 108 per spleen in animals reconstituted with cells from TGF-β1−/− donors, n = 3). Compared with week 6, CFC numbers were sharply decreased in spleen and blood from mice repopulated with WT cells, but the extent of decrease was far less pronounced in TGF-β1−/−–reconstituted mice (Table 3).
Histologically, spleens from animals repopulated with WT or TGF-β1−/− cells appeared similar whether examinations were performed at week 6 or 16. The spleen architecture was partly preserved. The major change was a hyperplasia of the red pulp due to an extensive proliferation of heterogeneous megakaryocytes often found in clusters and numerous maturing granulocytes (Figure 5A-B). However, when silver impregnation was used to examine the degree of fibrosis, densification of the reticulin network with deposition in the vicinity of megakaryocytes was observed as early as week 6 after graft in mice repopulated with WT cells (data not shown). At 4 months, fibrosis was dense and severe (Figure 5C). In sharp contrast, no densification of the reticulin network was seen in the TGF-β1−/− group during the time course (Figure 5D). A hyperplasia of megakaryocytes and granulocytic cells was also observed on sections from the femurs (Figure 5E-F). Upon silver impregnation, myelofibrosis was prominent in mice repopulated with WT cells (Figure 5G), whereas no changes in densification of reticulin were seen in the mice engrafted with TGF-β1−/− hematopoietic cells (Figure 5H). In addition, an increase in the femoral cortical thickness and formation of new bony trabeculae extending within the bone cavity were systematically observed in the WT group (Figure 5E,G). Osteosclerosis was not seen in the mice repopulated with TGF-β1−/− cells (Figure5F,H). In all the animals, extramedullary hematopoietic foci composed of megakaryocytes and neutrophils were observed in the liver, particularly in the sinusoidal spaces and along the portal tracts. No architectural change was noted in the kidney. However, one abnormality found in all the engrafted mice was small infiltrates of lymphocytes in the lung.
Histologic sections of spleen and femur from mice engrafted with WT or TGF-β1−/− virus–infected hematopoietic cells.
Three mice in each group (WT5, WT8, WT14 and KO8, KO11, KO14) were killed 4 months after transplantation. Representative sections are shown. Spleen sections stained by hematoxylin and eosin from (A) WT5 engrafted with TGF-β1+/+ cells and (B) KO14 engrafted with TGF-β1−/− cells show the hyperplasia of megakaryocytes and granulocytes. Silver staining revealed massive fibrosis in spleen sections from WT5 (C), whereas no significant reticulin deposition was detected in KO14 (D). Longitudinal femur sections stained by hematoxylin and eosin from WT5 (E) show the growth of new bone trabeculae within the marrow cavity and from KO14 (F) where no bone growth was detected. Silver staining of a femur section from WT5 (G) showing myelofibrosis and from KO14 (H) shows no deposition of reticulin fibers. Original magnifications: A-D, × 400; E-H, × 250.
Histologic sections of spleen and femur from mice engrafted with WT or TGF-β1−/− virus–infected hematopoietic cells.
Three mice in each group (WT5, WT8, WT14 and KO8, KO11, KO14) were killed 4 months after transplantation. Representative sections are shown. Spleen sections stained by hematoxylin and eosin from (A) WT5 engrafted with TGF-β1+/+ cells and (B) KO14 engrafted with TGF-β1−/− cells show the hyperplasia of megakaryocytes and granulocytes. Silver staining revealed massive fibrosis in spleen sections from WT5 (C), whereas no significant reticulin deposition was detected in KO14 (D). Longitudinal femur sections stained by hematoxylin and eosin from WT5 (E) show the growth of new bone trabeculae within the marrow cavity and from KO14 (F) where no bone growth was detected. Silver staining of a femur section from WT5 (G) showing myelofibrosis and from KO14 (H) shows no deposition of reticulin fibers. Original magnifications: A-D, × 400; E-H, × 250.
TGF-β1 levels in plasma, platelet extracts, and extracellular fluid of spleen
Changes of TGF-β1 levels were measured in PPP during the time course. The level of spontaneously active TGF-β1 was nonsignificant whether plasma was prepared from mice reconstituted with WT or TGF-β1−/− cells. When latent TGF-β1 was activated by acidification of the samples, no increase over levels found in normal hosts could be demonstrated in mice reconstituted with TGF-β1−/− hematopoietic cells. In contrast, levels of latent TGF-β1 were 4- to 8-fold increased at week 3 after transplantation and remained elevated during the follow-up in the mice repopulated with WT cells (Figure 6). Levels of TGF-β1 were compared in platelet extracts and extracellular fluid of spleens from normal mice and mice engrafted with WT cells (week 12 after engraftment). In all the samples, immunoreactive TGF-β1 was at or slightly above the detection limit of the assay (62.5 pg/mL). After acidification, levels in platelet extracts were not significantly different (49.6 ± 0.9 ng per 4 × 108platelets vs 40.5 ± 0.8 ng per 4 × 108 platelets, respectively; n = 3). However, a 4-fold increase over controls could be demonstrated in extracellular fluids from WT spleens (19.1 ± 3.7 ng/mL vs 5.7 ± 1.2 ng/mL in controls; P < .001; n = 3). Together, these results show that levels of latent TGF-β1 were increased in plasma and extracellular fluids of spleen from mice that developed a myelofibrosis and indicate that release of TGF-β1 by hematopoietic cells has a major impact in myelofibrosis induction.
TGF-β1 quantification in plasma.
Bars indicate TGF-β1 levels after acidification of the samples: ▪ indicate levels in mice engrafted with TGF-β1+/+hematopoietic cells; ■, levels in hosts engrafted with TGF-β1−/− hematopoietic cells; ▨, constitutive level in WT adult hosts. No spontaneously active TGF-β1 was detected prior to acidification of the samples. Results of statistical analysis with the 2-tailed Student t test: WT versus TGF-β1−/−, ★P < .05 and★★P < .001.
TGF-β1 quantification in plasma.
Bars indicate TGF-β1 levels after acidification of the samples: ▪ indicate levels in mice engrafted with TGF-β1+/+hematopoietic cells; ■, levels in hosts engrafted with TGF-β1−/− hematopoietic cells; ▨, constitutive level in WT adult hosts. No spontaneously active TGF-β1 was detected prior to acidification of the samples. Results of statistical analysis with the 2-tailed Student t test: WT versus TGF-β1−/−, ★P < .05 and★★P < .001.
Discussion
The critical role of TGF-β1 has been established in a variety of fibrotic disorders,11,32 but the impact of this cytokine in the development and progression of myelofibrosis has not been fully investigated. To address this issue, we exploited an experimental murine model in which overexpression of TPO by genetically modified hematopoietic cells induces severe fibrosis in hemopoietic organs.21,23 The present study compared the pathological changes induced in irradiated WT recipients repopulated in the long term with TPO-overexpressing hematopoietic stem cells from homozygote mutant TGF-β1−/− or WT littermates. Because homozygote TGF-β1−/− mice die of a multifocal inflammatory syndrome at weaning time,24 33 it was not possible to perform these experiments in a background totally deficient in TGF-β1. Nevertheless, the data demonstrate the induction of a comparable myeloproliferative syndrome in hosts repopulated with TGF-β1−/− or WT marrow cells. However, while no sign of fibrosis was seen in spleen and marrow from hosts reconstituted with TGF-β1−/− donor cells (marrow chimerism > 70%), severe reticulin deposition was systematically observed in animals reconstituted with WT cells.
Previous studies on myelofibrosis induced in rodents by a chronic exposure to high TPO levels have suggested an implication of both TGF-β1 and PDGF-B in the stromal reaction.20,22However, a key impact of PDGF-B may be ruled out because a hyperexpression of this growth factor in mice caused a myeloproliferative syndrome but no myelofibrosis.34 To determine the contribution of TGF-β1, we undertook studies with TGF-β1–deficient hematopoietic stem cells. In the TGF-β1 knock-out models, the frequency of birth of homozygote null pups is highly dependent on the genetic background of the mothers.24,25,35 In this study, marrow transplants were obtained from TGF-β1−/− pups born on a mixed Sv129 × CF-1 genetic background, where a high proportion of born homozygotes develop normally until 2 weeks before they exhibit the wasting syndrome.24 One concern with marrow grafts originating from TGF-β1−/− donors was the possibility of transplanting the acute inflammatory syndrome as previously reported.36 In our experiments, none of the mice repopulated with Lin− cells from TGF-β1−/−donors developed clinical symptoms of acute illness or died with exaggerated inflammation during the follow-up of 8 months. Nevertheless, all the animals undergoing transplantation with WT or TGF-β1−/− cells developed small inflammatory lesions in the lung, which may be attributed to some immunologic reaction induced by the mixed genetic background of these animals.
Whatever the cell genotype, high and reproducible transduction levels in hematopoietic progenitors were difficult to achieve. In preliminary experiments, the Lin− fractions from both genotypes were cocultured on the Gp+E86 ecotropic packaging cell line producing the MPZenTPO virus as we previously described.23 Surprisingly, the proviral cDNA was detected in less than 5% of CFCs at the end of the infection protocol, whereas more than 80% were infected when C57Bl/6 marrow cells were tested as a control. Semiquantitative RT-PCR analysis of the ecotropic retrovirus receptor mRNA revealed a similar expression level in Lin− cells from Sv129 × CF-1 and C57Bl/6 mice, an observation that could not explain the resistance of Sv129 × CF-1 cells to infection (data not shown). To improve transduction efficiency, we produced retroviral particles pseudotyped with the vesicular stomatitis virus G (VSV-G), which can be concentrated to high titers.37 According to the demonstration that a short ex vivo prestimulation of primitive hematopoietic stem cells was sufficient to confer efficient gene transfer with VSV-G pseudotyped retroviruses,38Lin− cells from WT donors were induced to proliferation during 24 hours before being exposed to virions. The prestimulation step was omitted with the TGF-β1−/− Lin−cells because several reports indicate that autocrine TGF-β1 maintains hematopoietic stem cells in a quiescent state.27 28 Regardless of the cell genotype or the infection protocol, the percentage of transduced CFCs was not significantly different between the 2 groups of mice but never exceeded 36%. Further investigations are needed to understand the relative resistance to retrovirus infection of hematopoietic cells from Sv129 × CF-1 mice.
The comparison of the pathological changes seen in mice repopulated with TPO-overexpressing WT or TGF-β1−/− hematopoietic cells disclosed common features. All mice developed thrombocytosis, leukocytosis, and greatly increased numbers of progenitors in blood and spleen. When viewed in combination, no striking differences in the myeloproliferative syndrome induced in both groups of mice were seen, indicating that the repopulating and proliferating ability of stem cells from TGF-β1−/− donors was not markedly impaired. Upon histologic examination, hemopoietic tissues were invaded with an excess of megakaryocytes and granulocytes. However, although myelofibrosis was systematically observed in hemopoietic tissue from mice reconstituted with WT cells as early as week 6 after transplantation, no reticulin deposition was seen in mice repopulated with TGF-β1−/− hematopoietic cells even after 4 months. Because hosts were WT animals producing TGF-β1 constitutively, these observations support the notion that TGF-β1 released by hematopoietic cells plays a prominent role in the promotion of myelofibrosis. Of note, the frequency of CFCs in spleen and blood was greatly decreased in the WT group at the time of myelofibrosis development.23 This is merely related to the difficulty of extracting cells from the fibrous tissue. However, a direct inhibitory effect of TGF-β1 on primitive progenitor cells cannot be ruled out.27,28 In addition, osteosclerosis occurred after 4 months in all the mice engrafted with WT cells.22,23 This pathological process was not observed in mice repopulated with TGF-β1−/− cells. Although we cannot exclude that abnormal bone growth may occur at later times in these animals, it is recognized that TGF-β1 plays a pivotal role in the coupling between bone formation and resorption by stimulating osteoblasts39,40 and suppressing osteoclastogenesis.41 It is thus tempting to speculate that, in addition to its inductive effect on myelofibrosis, TGF-β1 may also be directly or indirectly involved in the abnormal bone growth observed in this animal model.
Measurements of TGF-β1 levels in plasma and spleen extracellular fluids from mice reconstituted with WT cells showed a 4- to 8-fold increase over normal hosts. In contrast to a previous work,20 no significant increment was found in platelet extracts. This may be related either to the different strategies used to induce myelofibrosis, the time of examination, or the animals. However, no immunoreactive TGF-β1 was measured in the circulation even when myelofibrosis was massive. Accordingly, we were unable to identify fibrotic lesions in distant organs known to be targets of the fibrogenic effect of TGF-β1, such as the lung, liver, or kidney. This indicates that critical regulatory mechanisms controlling TGF-β1 activation must take place within the hematopoietic environment at secretion sites. Cells involved in the abnormal secretion of TGF-β1 are not fully identified. Several observations postulate an important role of the megakaryocyte.7,16 Hyperplasia and disturbed differentiation of megakaryocytes are observed in human primary idiopathic myelofibrosis and in animal models of TPO hyperstimulation. In addition, on marrow biopsies, reticulin fibers are often seen in close vicinity to megakaryocytes,6 an observation also made in our murine model. However, other studies suggest an implication of the monocyte/macrophage. Indeed, myelofibrosis is seen in all subtypes of human myelodysplastic or chronic myeloproliferative disorders,1 and no fibrotic process was observed in monocyte-deficient nonobese diabetic/severe combined immunodeficient (NOD-SCID) mice treated with an adenovirus vector expressing the human TPO protein.42 Although our studies demonstrate an absence of reticulin deposition when hematopoietic cells are deficient in TGF-β1 production, we cannot exclude the possibility that some hypothetic accessory cells that might be required for myelofibrosis promotion are functionally impaired in TGF-β1−/− hematopoietic cells. The mechanisms involved in the local activation of TGF-β1 are complex and not yet understood. Nevertheless, recent studies suggest that megakaryocytes and/or monocytes might play a central role in the process of TGF-β activation in vivo. Thrombospondin-1 or integrins αvβ6, αIIbβ3, and αvβ3 are potent in vivo activators of TGF-β1.43,44 Because TGF-β1 and thrombospondin-1 are synthesized and stored within the same organelles in the megakaryocyte, it is tempting to speculate that the abnormal release of the 2 molecules in the microenvironment may contribute to local TGF-β1 activation. Furthermore, megakaryocytes and platelets express the integrins αIIbβ3 and αvβ3, which may also participate in the local activation of TGF-β1. Alternatively, monocytes are sources of cytokines that are potent stimulators and activators of TGF-β1 in vivo.45 The availability of knock-out mice for these different pathways would be useful models to dissect the mechanism(s) accounting for TGF-β1 activation in the marrow environment.
The present studies add to our understanding of the pathophysiology of myelofibrosis by demonstrating that TGF-β1 overproduction is a major contributor to the pathogenesis of this process. Although the molecular mechanisms leading to aberrant clonal proliferation of malignant hematopoietic cells in human syndromes with myelofibrosis are not fully understood, the mouse model offers an experimental assay to test new therapeutic approaches aimed at decreasing TGF-β1 production and/or activation and to study the beneficial effects on the progression of myelofibrotic disorders in which no drug therapy exists.3
We are grateful to Dr T. Doetschman for kindly providing the heterozygote TGF-β1 breeders, to Dr W. Pear for providing the MIGR vector, and to Drs J. Morgenstien and J. L. Villeval for providing the plasmids. We acknowledge A. Rouchès for her assistance with the animals and A. M. Hagnere for her expert assistance with the histopathological studies.
Prepublished online as Blood First Edition Paper, July 5, 2002; DOI 10.1182/blood-2002-04-1133.
Supported by grants from the Institut National de la Santéet de la Recherche Médicale, the Institut Gustave Roussy, the Ministère de la Recherche, and the Ligue Nationale contre le Cancer (Equipe labellisée 2000).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
William Vainchenker, INSERM U362, Institut Gustave Roussy, 39 rue Camille Desmoulins, 94805 Villejuif, France; e-mail: verpre@igr.fr.