Abstract
To determine whether the antigen-driven T-cell response is involved in the pathogenesis of aplastic anemia (AA), we examined the complementarity-determining region 3 (CDR3) size distribution of T-cell receptor (TCR) β-chain (BV) subfamilies in the bone marrow (BM) of untreated AA patients. AA patients who did not respond to immunosuppressive therapy and those who obtained unmaintained remission early after cyclosporine (CyA) or antithymocyte globulin (ATG) therapy exhibited essentially a normal CDR3 size pattern. In contrast, five patients who needed continuous administration of CyA to maintain remission exhibited a skewed CDR3 size pattern in a number (>40%) of BV subfamilies suggestive of clonal predominance. The skewing of CDR3 size distribution became less pronounced in one of the CyA-dependent patients when the patient achieved unmaintained remission after a 4-year therapy with CyA, whereas it persisted longer than 7 years in the other patient requiring maintenance therapy. Sequencing of BV15 cDNA for which the CDR3 size pattern exhibited apparent clonal predominance in all CyA-dependent patients showed high homology of the amino acid sequence of the CDR3 between two different patients. These findings indicate that antigen-driven expansion of T cells is involved in the pathogenesis of AA characterized by CyA-dependent recovery of hematopoiesis.
APLASTIC ANEMIA (AA) is a syndrome characterized by pancytopenia and bone marrow (BM) hypoplasia. Although the etiology is unknown, clinical observations such as the high rate of response to immunosuppressive therapy in patients with AA suggest the importance of immune mechanisms in the development of AA.1,2 Among several immune mechanisms, T-cell–mediated suppression of hematopoiesis has been considered the most important in the development of AA.3 This hypothesis has been supported by in vitro findings such as suppression of hematopoietic progenitor cell growth4-6 and increased production of myelosuppressive cytokines by the patients’ T cells,7-10 as well as an increased proportion of activated T cells in the peripheral blood11,12 and BM.13 Recent studies demonstrated that T-cell clones capable of inhibiting autologous hematopoietic progenitor cells can be generated by culturing T cells of AA patients with autologous hematopoietic progenitor cells.14 15 These findings suggest that AA is a type of autoimmune disease that involves a T-cell attack against hematopoietic progenitor cells. However, there has been no convincing evidence for involvement of the antigen-driven T-cell response in the development of AA, not to mention the causal antigen that elicits the T-cell attack against hematopoietic progenitor cells.
In well-known autoimmune diseases such as multiple sclerosis16-18 and rheumatoid arthritis,19,20the T-cell repertoire in the involved organ has been extensively studied to characterize an antigen-driven response that may induce the disease process. It was revealed that a limited number of T cells using a restricted diversity of the T-cell receptor (TCR) β chain (BV) dominantly proliferated in the involved organ.21 Such oligoclonal proliferation of T cells is generally thought to reflect the specific response of autoreactive T cells to certain antigens, since T cells bearing similar BV subfamilies have been demonstrated to proliferate dominantly in different patients and the TCR repertoire of these patients is distinct from that of patients with other inflammatory diseases due to a definite pathogen.16,18 22If specific recognition of hematopoietic cells by T cells plays a role in the development of AA, clonal expansion of a limited number of T cells should be observed in the BM of AA patients as well. Such clonally expanding T cells in the BM of different patients may share a clonotype if a common antigen is responsible for inciting T cells to attack hematopoietic cells.
To test these hypotheses, we analyzed the T-cell repertoire in the BM of AA patients. Since AA is a mixture of illnesses with BM hypoplasia, studying unselected patients is expected to produce varying results that may be hard to interpret. We thus limited the study subjects to patients who were treated with cyclosporine (CyA) or antithymocyte globulin (ATG) after a failure to respond to CyA. Complementarity-determining region 3 (CDR3) size distribution analysis, single-strand conformation polymorphism (SSCP) analysis, and sequencing of TCR cDNA were used to determine whether clonal expansion of a limited number of T cells occurs in the BM. Clonal predominance was not evident in AA patients who obtained unmaintained remission early after CyA or ATG therapy after failing to respond to CyA and those who did not respond to CyA therapy, whereas it was present in a number of BV families in AA patients with HLA-DRB1*1501 whose hematopoietic function depended on continuous administration of CyA. Sequencing of BV15 cDNA for which the CDR3 size profile exhibited apparent clonal predominance in all CyA-dependent patients showed a high homology of the amino acid sequence of the CDR3 between two different patients with CyA-dependent AA.
MATERIALS AND METHODS
Patients.
Eighteen patients with idiopathic AA were included in the analysis of the T-cell repertoire in the BM. These patients were first treated with CyA 4 to 6 mg/kg daily for at least 4 months, and nonresponders were subsequently treated with ATG 15 mg/kg daily for 5 days. The BM of 14 normal subjects aged 16 to 51 years was studied as a control. All but two patients (patients no. 8 and 9) were untransfused at the time of sampling. Three of 14 normals (normals no. 1, 2, and 3) possessed HLA-DRB1*1501. Table 1 summarizes clinical characteristics of the patients. Patients no. 1 to 9 improved with CyA therapy. Patients no. 1 to 4 achieved unmaintained remission after CyA therapy for 10 to 20 months, whereas CyA could not be withdrawn within 3 years due to the recurrence of pancytopenia after dose reduction or cessation of CyA in patients no. 5 to 9; in these patients, AA was thus designated CyA-dependent. All patients with CyA-dependent AA possessed HLA-DRB1*1501, which is strongly associated with this type of AA.23 24 Patients no. 10 to 13 improved with ATG after failure with CyA therapy. Patients no. 14 to 18 did not respond to CyA therapy; three (no. 14, 16, and 18) underwent BM transplantation from HLA-identical siblings after treatment failure with CyA. BM was obtained before treatment from all but one patient (no. 5), who underwent sampling at the time of exacerbation of AA in association with the dose reduction of CyA. All patients provided informed consent prior to sampling, and the study was approved by the institutional human research committee.
Patient Characteristics
| Patient No. . | Age (yr)/ Sex . | Diagnosis . | Response to Therapy . | CyA Dependency . | HLA-DRB1 Allele . |
|---|---|---|---|---|---|
| 1 | 60/F | MAA | CyA | − | 1302/1502 |
| 2 | 46/M | SAA | CyA | − | 0101405 |
| 3 | 58/M | SAA | CyA | − | 1502801 |
| 4 | 78/M | SAA | CyA | − | 0405601 |
| 5 | 65/M | MAA | CyA | + | 1501405 |
| 6 | 17/M | SAA | CyA | + | 1501/1405 |
| 7 | 43/M | SAA | CyA | + | 1501/1302 |
| 8 | 32/M | MAA | CyA | + | 1501/1501 |
| 9 | 60/F | MAA | CyA | + | 1501/1201 |
| 10 | 49/F | SAA | ATG | − | 1401/1502 |
| 11 | 65/F | MAA | ATG | − | 1502/1402 |
| 12 | 63/F | SAA | ATG | − | 1502802 |
| 13 | 20/M | SAA | ATG | − | 0801405 |
| 14 | 23/M | SAA | — | − | 1301803 |
| 15 | 61/F | SAA | — | − | 0405405 |
| 16 | 24/F | MAA | — | − | 1502/1301 |
| 17 | 19/M | MAA | — | − | 1501/1201 |
| 18 | 15/F | SAA | — | − | 1502405 |
| Patient No. . | Age (yr)/ Sex . | Diagnosis . | Response to Therapy . | CyA Dependency . | HLA-DRB1 Allele . |
|---|---|---|---|---|---|
| 1 | 60/F | MAA | CyA | − | 1302/1502 |
| 2 | 46/M | SAA | CyA | − | 0101405 |
| 3 | 58/M | SAA | CyA | − | 1502801 |
| 4 | 78/M | SAA | CyA | − | 0405601 |
| 5 | 65/M | MAA | CyA | + | 1501405 |
| 6 | 17/M | SAA | CyA | + | 1501/1405 |
| 7 | 43/M | SAA | CyA | + | 1501/1302 |
| 8 | 32/M | MAA | CyA | + | 1501/1501 |
| 9 | 60/F | MAA | CyA | + | 1501/1201 |
| 10 | 49/F | SAA | ATG | − | 1401/1502 |
| 11 | 65/F | MAA | ATG | − | 1502/1402 |
| 12 | 63/F | SAA | ATG | − | 1502802 |
| 13 | 20/M | SAA | ATG | − | 0801405 |
| 14 | 23/M | SAA | — | − | 1301803 |
| 15 | 61/F | SAA | — | − | 0405405 |
| 16 | 24/F | MAA | — | − | 1502/1301 |
| 17 | 19/M | MAA | — | − | 1501/1201 |
| 18 | 15/F | SAA | — | − | 1502405 |
Abbreviations: SAA, severe AA; MAA, moderate AA.
RNA extraction and cDNA preparation.
BM mononuclear cells (BMMCs) were isolated using density gradient centrifugation. For the BMMCs of patient no. 5, CD4+ and CD8+ cells were sorted using monoclonal antibodies (Becton-Dickinson, Mountain View, CA) and an Epics C cell sorter (Coulter Electronic Inc, Hialeah, FL). Total RNA was extracted from BMMCs and the T-cell subset using a technique described elsewhere,25 and then reverse-transcribed into cDNA in a reaction primed with oligo(dT)12-18 using SuperScript II reverse transcriptase as recommended by the manufacturer (GIBCO-BRL, Bethesda, MD).
CDR3 size distribution analysis.
Conditions for the CDR3 size distribution analysis have been reported elsewhere.21,26,27 Briefly, cDNA was polymerase chain reaction (PCR)-amplified through 35 cycles (94°C for 1 minute, 55°C for 1 minute, and 72°C for 1 minute) with a primer specific to 24 different BV subfamilies (BVs1-2028 and BVs21-2429) and a fluorescent BC primer.28 The analysis of BV10 and BV19 was excluded from this study because these are pseudogenes.30 One microliter of amplified products was mixed with 1.5 μL 100% formamide and 0.5 μL size standard (Genescan-500 ROX,ABI 373; Perkin-Elmer, Urayasu, Japan), heated at 90°C for 3 minutes, and electrophoresed in a 6.75% denaturing polyacrylamide gel. The distribution of CDR3 size within the amplified product of each BV subfamily was analyzed using an automatic sequencer (Applied Biosystems, Foster City, CA) equipped with a computer program allowing determination of the fluorescence intensity of each band. The results are depicted as peaks corresponding to the intensity of the fluorescence. CDR3 size patterns that failed to exhibit a bell-shaped distribution due to the appearance of prominent peaks with or without a reduced peak number (< five peaks) were judged to be abnormal. This judgment was made by three different investigators to minimize interindividual differences. The frequency of BV subfamilies displaying an abnormal CDR3 size profile was determined for each subject.
Given the BV-NDN-BJ sequence of the most dominant clone characterized in patient no. 5, a more specific primer covering both CDR3 and BJ2.2 (5′-TGTTCGGCCCGCTAGTCAGGTCACT-3′) was designed specifically to amplify cDNA of the BV15-positive (BV15+) T-cell clone in different T-cell subsets. The BV15+ amplified products from patient no. 5 were submitted to five cycles of primer extension using the fluorescent clonotypic primer under the same PCR conditions and analyzed in the same way as before.31
SSCP analysis.
cDNA amplified by PCR with a combination of BC and BV primers after 35 cycles of PCR was diluted in the SSCP loading buffer (95% formamide, 10 mmol/L EDTA, 0.1% bromophenol blue, and 0.1% xylene cyanol), heated at 90°C for 2 minutes to denature, and then subjected to nondenaturing 5% polyacrylamide gel electrophoresis at constant power and temperature.32 The DNA was then transferred to Immobilon-S (Millipore Intertech, Bedford, MA) and hybridized with a biotinylated BC probe (5′-AACAAGCGTGTTCCCGAGGTCGCTGTGTT-3′) at 42°C overnight. The membrane was washed with 0.2X SSPE and 0.5% sodium dodecyl sulfate for 10 minutes at 55°C and visualized by subsequent incubation of streptoavidin, biotinylated alkaline phosphatase, and a chemiluminescent substrate system (Plex Luminescence kit, Millipore).
Cloning and sequencing of PCR-amplified cDNA.
PCR products of BV15 cDNA were electrophoresed on an agarose gel. The amplified fragment of expected size was purified using DEAE paper and cloned into a pGEM-T Vector system (Promega Corp, Madison, WI). Eighteen to 40 colonies containing the insert fragment were randomly selected and sequenced using an ABI pRISM cycle Sequencing Kit (Perkin-Elmer) and an automatic DNA sequencer (ABI 373; Perkin-Elmer). The amino acid sequence of CDR3 was deduced using DNASIS-Mac Version 3.6 software (Hitachi Software, Yokohama, Japan).
Statistical methods.
Differences in the frequency of BV subfamilies displaying an abnormal CDR3 size profile and in the frequency of clones exhibiting the identical CDR3 sequence among all cDNA clones sequenced between control and patient groups were tested using the unpaired Student’st-test and Mann-Whitney U test, respectively.
RESULTS
CDR3 size distribution of TCR BV cDNA of BM T cells.
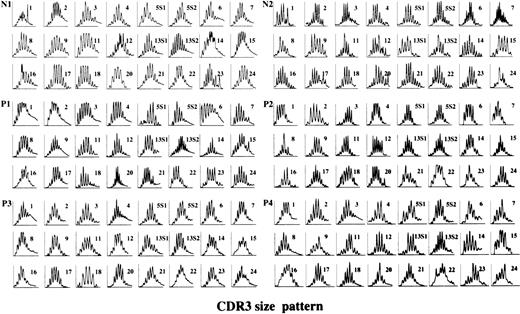
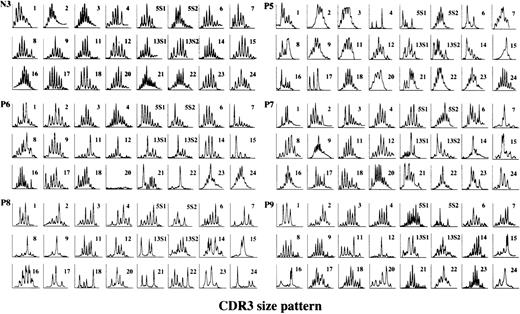
The cDNA of 24 different BV subfamilies was amplified using a fluorescent BC primer, and the CDR3 size distribution of each BV subfamily was compared among normal individuals and AA patients responsive to immunosuppressive therapy. CDR3 patterns of two normal individuals possessing HLA-DRB1*1501 (normals no. 1 and 2) and four AA patients (no. 1 to 4) who obtained unmaintained remission early after CyA therapy are shown in Fig 1. In normal individuals, some BV subfamilies exhibited skewed CDR3 size distribution; the frequency of BV subfamilies displaying an abnormal CDR3 size profile in relation to all BV subfamilies was 11.0% ± 6.4% (mean ± SD). The majority of the amplified products of AA patients (4.2% ± 5.9%, P = .1) displayed a bell-shaped size pattern, with more than five peaks as well, indicating the predominance of polyclonal T cells. In contrast, a number of BV subfamilies in patients with CyA-dependent AA (54.2% ± 14.0%,P < .0001) displayed an apparently skewed distribution of CDR3 size, indicating clonal or oligoclonal proliferation of T cells (Fig 2). Figure3 illustrates CDR3 size profiles of four patients who did not respond to CyA but improved with subsequent ATG therapy. Although several BV families exhibited skewed CDR3 patterns, the frequency of BV families displaying abnormal CDR3 size patterns was comparable to the frequency for normal controls (16.7% ± 4.8%,P = .1). Its frequency in the other five patients refractory to CyA therapy (no. 14 to 18) was also comparable to the frequency for normal controls (10.1% ± 7.6%, P = .8). Table2 summarizes the number of BV subfamilies and the proportion of abnormal BV families in all patients. These results suggest that among AA patients responsive to immunosuppressive therapy, clonal proliferation of a limited number of T cells in the BM might occur primarily in those characterized by the CyA-dependent response.
CDR3 size distribution of TCR BV derived from BM T cells of AA patients who obtained unmaintained remission early after CyA therapy. cDNA that was amplified using primers specific for 24 different BV subfamilies and coupled with a fluorescent BC primer was analyzed for size with the gene scan program. N1 and N2, normals no. 1 and 2 possessing HLA-DRB1*1501; P1-P4, patients no. 1-4. Most BV subfamilies of the patients and normal controls displayed a bell-shaped size pattern with >5 peaks, indicating the predominance of polyclonal T cells.
CDR3 size distribution of TCR BV derived from BM T cells of AA patients who obtained unmaintained remission early after CyA therapy. cDNA that was amplified using primers specific for 24 different BV subfamilies and coupled with a fluorescent BC primer was analyzed for size with the gene scan program. N1 and N2, normals no. 1 and 2 possessing HLA-DRB1*1501; P1-P4, patients no. 1-4. Most BV subfamilies of the patients and normal controls displayed a bell-shaped size pattern with >5 peaks, indicating the predominance of polyclonal T cells.
CDR3 size distribution of TCR BV derived from BM T cells of CyA-dependent AA patients. TCR cDNA of another normal individual with HLA-DRB1*1501 (N3, normal no. 3) and patients no. 5-9 (P5-P9) whose hematopoietic function depended on continuous administration of CyA was analyzed. A large number of BV subfamilies (> 40%) of the patients displayed a skewed or collapsed pattern with a reduced peak number, indicating clonal or oligoclonal proliferation of T cells.
CDR3 size distribution of TCR BV derived from BM T cells of CyA-dependent AA patients. TCR cDNA of another normal individual with HLA-DRB1*1501 (N3, normal no. 3) and patients no. 5-9 (P5-P9) whose hematopoietic function depended on continuous administration of CyA was analyzed. A large number of BV subfamilies (> 40%) of the patients displayed a skewed or collapsed pattern with a reduced peak number, indicating clonal or oligoclonal proliferation of T cells.
CDR3 size distribution of TCR BV derived from BM T cells of AA patients who responded to ATG after treatment failure with CyA. TCR cDNA of patients no. 10-13 (P10-P13) was analyzed. Although several BV families exhibited skewed CDR3 patterns, the frequency of BV families displaying abnormal CDR3 size patterns was comparable to normal controls.
CDR3 size distribution of TCR BV derived from BM T cells of AA patients who responded to ATG after treatment failure with CyA. TCR cDNA of patients no. 10-13 (P10-P13) was analyzed. Although several BV families exhibited skewed CDR3 patterns, the frequency of BV families displaying abnormal CDR3 size patterns was comparable to normal controls.
BV Subfamilies Showing Abnormal CDR3 Size Pattern
| Patient No. . | BV No. With Abnormal CDR3 Size Pattern . | BV Subfamilies With CDR3 Abnormalities (%) . |
|---|---|---|
| 1 | — | 0 |
| 2 | 8 | 4.2 |
| 3 | — | 0 |
| 4 | 15, 22, 24 | 12.5 |
| 5 | 1, 4, 5S1, 6, 8, 13S1, 13S2, 14, 15, 16, 17, 21 | 50.0 |
| 6 | 5S2, 7, 11, 12, 13S1, 13S2, 14, 15, 20, 21, 22 | 45.8 |
| 7 | 1, 6, 7, 13S1, 13S2, 14, 15, 21, 22, 23, 24 | 45.8 |
| 8 | 1, 2, 3, 4, 5S2, 7, 8, 9, 13S1, 14, 15, 16, 17, 18, 21, 22, 23, 24 | 75.0 |
| 9 | 1, 2, 5S2, 11, 12, 13S1, 15, 16, 20, 24 | 41.7 |
| 10 | 14, 22, 23 | 12.5 |
| 11 | 3, 7, 21 | 12.5 |
| 12 | 9, 11, 22, 23, 24 | 20.8 |
| 13 | 3, 5S1, 7, 14, 21 | 20.8 |
| 14 | — | 0 |
| 15 | 8, 9, 24 | 12.5 |
| 16 | 5S2 | 4.2 |
| 17 | 7, 21, 23, 24 | 16.7 |
| 18 | 6, 7, 15, 23 | 16.7 |
| Patient No. . | BV No. With Abnormal CDR3 Size Pattern . | BV Subfamilies With CDR3 Abnormalities (%) . |
|---|---|---|
| 1 | — | 0 |
| 2 | 8 | 4.2 |
| 3 | — | 0 |
| 4 | 15, 22, 24 | 12.5 |
| 5 | 1, 4, 5S1, 6, 8, 13S1, 13S2, 14, 15, 16, 17, 21 | 50.0 |
| 6 | 5S2, 7, 11, 12, 13S1, 13S2, 14, 15, 20, 21, 22 | 45.8 |
| 7 | 1, 6, 7, 13S1, 13S2, 14, 15, 21, 22, 23, 24 | 45.8 |
| 8 | 1, 2, 3, 4, 5S2, 7, 8, 9, 13S1, 14, 15, 16, 17, 18, 21, 22, 23, 24 | 75.0 |
| 9 | 1, 2, 5S2, 11, 12, 13S1, 15, 16, 20, 24 | 41.7 |
| 10 | 14, 22, 23 | 12.5 |
| 11 | 3, 7, 21 | 12.5 |
| 12 | 9, 11, 22, 23, 24 | 20.8 |
| 13 | 3, 5S1, 7, 14, 21 | 20.8 |
| 14 | — | 0 |
| 15 | 8, 9, 24 | 12.5 |
| 16 | 5S2 | 4.2 |
| 17 | 7, 21, 23, 24 | 16.7 |
| 18 | 6, 7, 15, 23 | 16.7 |
SSCP analysis of amplified BV cDNA of BM T cells.
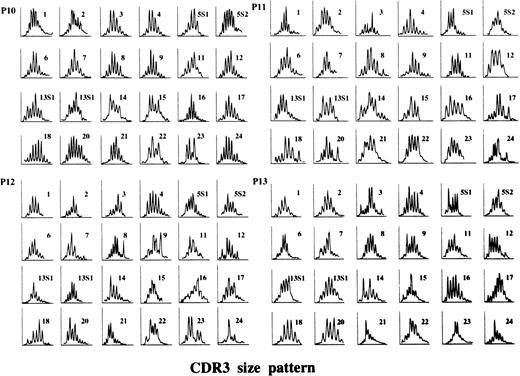
The skewed CDR3 size distribution does not necessarily indicate the presence of clonally proliferating T cells, since a prominent peak in the histogram may represent the presence of polyclonal T cells with the same CDR3 size. To confirm clonal proliferation of T cells with several BVs in the BM of AA patients, amplified BV cDNA products were subjected to SSCP analysis. Figure 4 shows the results for selected BV families. The amplified products of BV cDNA of a normal individual exhibited a smear, indicating a predominance of polyclonal T cells. In contrast, the amplified products derived from three CyA-dependent patients (no. 5, 6, and 9) exhibited distinct bands in these BVs, indicating clonal expansion of a limited number of T cells. Although the amplified products of BV14 and BV15 of patient no. 11 produced discernible bands, the intensity of the bands was much lower than for patients no. 5, 6, and 9.
SSCP analysis of TCR BV cDNA derived from BM of AA patients. Amplified BV cDNA from a normal individual (N3, normal no. 3), P5 (patient no. 5), P6, P9, and P11 was subjected to SSCP analysis.
SSCP analysis of TCR BV cDNA derived from BM of AA patients. Amplified BV cDNA from a normal individual (N3, normal no. 3), P5 (patient no. 5), P6, P9, and P11 was subjected to SSCP analysis.
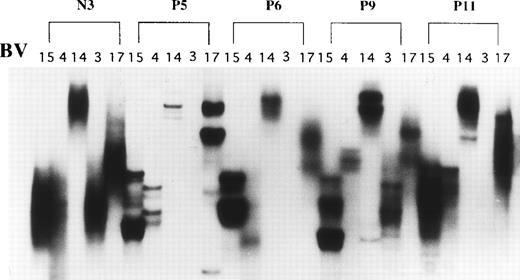
Changes in CDR3 size pattern associated with achievement of stable remission off CyA therapy.
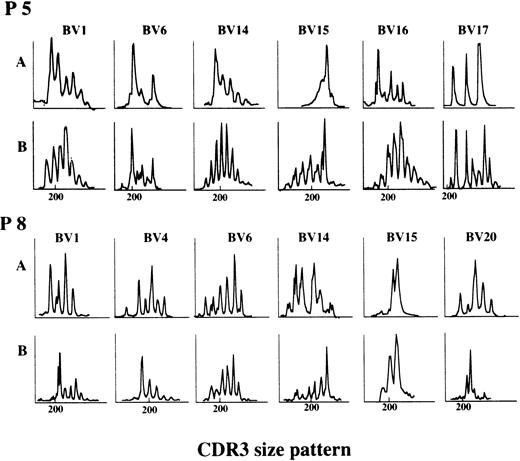
CyA could be withdrawn from patient no. 5 without aggravation of the pancytopenia 4 years after initiating the therapy. The CDR3 size distribution in BM T cells at the time of unmaintained remission, as well as that in patient no. 8, who required low-dose CyA to maintain stable hematopoiesis for more than 7 years after therapy, was analyzed and compared with the distribution obtained at the time the disease was active. Figure 5 illustrates the changes in the CDR3 size pattern of representative BV subfamilies. Although some showed a slightly skewed pattern, most BVs of patient no. 5 obtained at the time of remission exhibited more than five peaks, suggesting the recovery of polyclonal predominance associated with resolution of CyA-dependent AA (Fig5A). In contrast, skewed CDR3 size patterns of several BV families of patient no. 8 persisted after 7 years (Fig5B) despite the fact that the patient was in remission with 2 mg/kg/d CyA.
Changes in CDR3 size patterns associated with achievement of stable remission off CyA therapy. CDR3 size patterns of patient no. 5 (P5) at the time of unmaintained remission after 4 years of CyA therapy and patient no. 8 (P8) in CyA-dependent remission after 7 years of therapy were compared with patterns at the time the disease was active. A, before CyA therapy; B, after CyA therapy.
Changes in CDR3 size patterns associated with achievement of stable remission off CyA therapy. CDR3 size patterns of patient no. 5 (P5) at the time of unmaintained remission after 4 years of CyA therapy and patient no. 8 (P8) in CyA-dependent remission after 7 years of therapy were compared with patterns at the time the disease was active. A, before CyA therapy; B, after CyA therapy.
Deduced amino acid sequence of CDR3 of BV15 cDNA.
These findings indicate that oligoclonal expansion of a limited number of T cells was a feature common to the BM of CyA-dependent AA patients possessing HLA-DRB1*1501. To demonstrate directly the clonal expansion of a limited number of T cells, we cloned the amplified products of BV15 cDNA derived from the BM of three normal individuals with HLA-DRB1*1501 and five CyA-dependent patients (no. 5 to 9) and determined the nucleotide sequence of CDR3 of cDNA clones that were randomly selected. BV15 was chosen because the clonal predominance of this BV family was detected in all CyA-dependent AA patients (Table 2), and the intensity of the band in the SSCP gel appeared to be the strongest (Fig 4). Tables 3 and4 summarize the deduced amino acid sequence of each clone from three normal individuals and from CyA-dependent AA patients, respectively. In normals no. 1 to 3, some sequences were detected repeatedly, although their frequency was four in 30 at most. In contrast, a large number of clones proved identical in each AA patient. The most frequent amino acid (nucleotide) sequence of the N-D-N region and its frequency in the total clones of each patient was DLTSGP (GACCTGACTAGCGGGCCG, 21 of 30) in patient no. 5, GSP (GGCTCCCCC, 14 of 38) in patient no. 6, PRDRR (CCTAGAGACAGAAGG, 18 of 30) in patient no. 7, DLTNGP (GACCTGACTAACGGGCCG, seven of 40) in patient no. 8, and DESY (GATGAGTCGTAT, seven of 18) in patient no. 9. The frequency of identical N-D-N sequences was significantly higher in CyA-dependent AA patients versus normal individuals with HLA-DRB1*1501 (P = .025, Mann-Whitney U test). Such high frequencies of certain clones were compatible with the results of the CDR3 size distribution and SSCP analysis showing clonal predominance in BV15+ T cells. Furthermore, N-D-N sequences of patients no. 5 and 8 were identical to those of the BV15 cDNA extracted from the strongest band in the SSCP gel (Fig 4 and data not shown). Interestingly, the amino acid sequence of the DLTSGP of patient no. 5 differed from the DLTNGP of patient no. 8 by only one amino acid.
Junctional Amino Acid Sequences of TCR BV15 From Normal Individuals With HLA-DRB1*1501
| Subject No. . | ||||
|---|---|---|---|---|
| BV15 . | N-D-N . | BJ . | . | Frequency . |
| Normal 1 | ||||
| CATS | DAGGD | QPQHFGDGTRLSIL | 1S5 | 4/30 |
| CATS | DLAGFH | NEQFFGPGTRLTV | 2S1 | 2/30 |
| CATS | DSKRTS | GETYEQYFGPGTRLTVT | 2S5 | 2/30 |
| CATS | DYRS | GEQYFGPGTRLTVT | 2S5 | 1/30 |
| CATS | GLAGS | QETQYFGPGTRLLVL | 2S5 | 1/30 |
| CATS | DMTGPA | YNEQFFGPGTRLTVL | 2S1 | 1/30 |
| CATS | DFKGD | NEQFFGPGTRLTVL | 2S1 | 1/30 |
| CATS | VAGGD | EQFFGPGTRLTVL | 2S1 | 1/30 |
| CATS | TDRGH | GDTQYFGPGTRLTVL | 2S3 | 1/30 |
| CATS | VRVG | DEQFFGPGTRLTVL | 2S1 | 1/30 |
| CAT | LELAGS | YNEQFFGPGTRLTVL | 2S1 | 1/30 |
| CAT | RR | TGLDFGAGTRLSVL | 1/30 | |
| CATS | DPTSGI | YNEQFFGPGTRLTVL | 2S1 | 1/30 |
| CAT | RGTGS | NTEAFFGQGTRLTVV | 1S1 | 1/30 |
| CATS | DRTS | GANVLTFGAGSRLTVL | 2S6 | 1/30 |
| CATS | TRHAG | TGELFFGEGSRLTVL | 2S2 | 1/30 |
| CATS | DGHVG | QETQYFGPGTRLLVL | 2S5 | 1/30 |
| CATS | DASGRI | EQFFGPGTRLTVL | 2S1 | 1/30 |
| CATS | DGVS | GDTQYFGPGTRLTVL | 2S3 | 1/30 |
| CATS | VHAGS | QETQYFGPGTRLLVL | 2S5 | 1/30 |
| CATS | GPH | NTEAFFGQGTRLTVV | 1S1 | 1/30 |
| CATS | RSVG | NEQFFGPGTRLTVL | 2S1 | 1/30 |
| CATS | DHVSLE | GDTQYFGPGTRLTVL | 2S3 | 1/30 |
| CATS | QYLAGS | TGELFFGEGSRLTVL | 2S2 | 1/30 |
| CATS | APSHG | YNEQFFGPGTRLTVL | 2S1 | 1/30 |
| CATS | EWKDHSA | YNEQFFGPGTRLTVL | 2S1 | 1/30 |
| Normal 2 | ||||
| CATS | RAKG | ETQYFGPGTRKKVL | 2S5 | 2/26 |
| CATS | AEGSG | TQYFGPGTRLTVL | 2S3 | 2/26 |
| CATS | AEAGSPS | GANVLTFGAGSRLTVL | 2S6 | 2/26 |
| CATS | DPDR | YQETQYFGPGTRLLVL | 2S5 | 2/26 |
| CATS | EAGID | GANVLTFGAGSRLTVL | 2S6 | 1/26 |
| CATS | DASGRI | EQFFGPGTRLTVL | 2S1 | 1/26 |
| CATS | IPNQ | ALQPHFGDGTRLSIL | 1S5 | 1/26 |
| CATS | DYGTGG | YNEQFFGPGTRLTVL | 2S1 | 1/26 |
| CATS | YFWRIP | YNEQFFGPGTRLTVL | 2S1 | 1/26 |
| CATS | DHGQGE | ETQYFGPGTRLLVL | 2S5 | 1/26 |
| CATS | DYRS | GEQYFGPGTRLTV | 2S5 | 1/26 |
| CATS | DRAG | TDTQYFGPGTRLTVL | 2S3 | 1/26 |
| CATS | DRAG | TDTQYFGPGTRLTVL | 2S3 | 1/26 |
| CATS | DSGTSIG | TQYFGPGTRLLVL | 2S3 | 1/26 |
| CATS | DGGTA | EQFFGPGTRLTVL | 2S1 | 1/26 |
| CATS | AKGTV | ALQPHFGDGTRLSIL | 1S5 | 1/26 |
| CATS | RGDTA | GANVLTFGAGSRLTVL | 2S6 | 1/26 |
| CATS | DKQSG | ETQYFGPGTRKKVL | 2S5 | 1/26 |
| CATS | VGKAP | EQFFGPGTRLTVL | 2S1 | 1/26 |
| CATS | DAGSTWS | YNEQFFGPGTRLTVL | 2S1 | 1/26 |
| CATS | DGSHK | GANVLTFGAGSRLTVL | 2S6 | 1/26 |
| CATS | SGPG | TQYFGPGTRLLVL | 2S3 | 1/26 |
| CATS | DLHK | TQYFGPGTRLLVL | 2S3 | 1/26 |
| Normal 3 | ||||
| CATS | DGHQ | ETQYFGPGTRLLVL | 2S5 | 1/20 |
| CAT | GATG | TDTQYFGPGTRLTVL | 2S3 | 1/20 |
| CATS | DNRAS | DTQYFGPGTRLTVL | 2S3 | 1/20 |
| CATS | EGSY | YGYTFGSGTRLTVL | 1/20 | |
| CATS | DPRPGG | TDTQYFGPGTRLTVL | 2S3 | 1/20 |
| CATS | DSVSS | YNEQFFGPGTRL | 2S1 | 1/20 |
| CATS | DPYH | EQFFGPGTRLTVL | 2S1 | 1/20 |
| CATS | DIGT | TDTQYFGPGTRLTVL | 2S3 | 1/20 |
| CATS | LGASTS | YNEQFFGPGTRLTVL | 2S1 | 1/20 |
| CATS | DWVGMRSGKP | NEQFFGPGTRLTVL | 2S1 | 1/20 |
| CATS | DLF | EAFFGQGTRLTVV | 1S1 | 1/20 |
| CATS | DPPG | NEQFFGPGTRLTVL | 2S1 | 1/20 |
| CAT | RARQGGS | EQFFGPGTRLTVL | 2S1 | 1/20 |
| CAT | PRTSGAPT | EQFFGPGTRLTVL | 2S1 | 1/20 |
| CATS | DSRHTSGS | EQFFGPGTRLTVL | 2S1 | 1/20 |
| CATS | DGQGAHDA | EAFFGQGTRLTVV | 1S1 | 1/20 |
| CATS | DAGGD | QPQHFGDGTRLSIL | 1S5 | 1/20 |
| CATS | EPTGNPN | QPQGFGDGTRLSIL | 1S5 | 1/20 |
| CATS | DTGTG | TDTQYGPGTRLTVL | 2S3 | 1/20 |
| CATS | GRDWSS | YNEQFFGPGTRLTVL | 2S1 | 1/20 |
| Subject No. . | ||||
|---|---|---|---|---|
| BV15 . | N-D-N . | BJ . | . | Frequency . |
| Normal 1 | ||||
| CATS | DAGGD | QPQHFGDGTRLSIL | 1S5 | 4/30 |
| CATS | DLAGFH | NEQFFGPGTRLTV | 2S1 | 2/30 |
| CATS | DSKRTS | GETYEQYFGPGTRLTVT | 2S5 | 2/30 |
| CATS | DYRS | GEQYFGPGTRLTVT | 2S5 | 1/30 |
| CATS | GLAGS | QETQYFGPGTRLLVL | 2S5 | 1/30 |
| CATS | DMTGPA | YNEQFFGPGTRLTVL | 2S1 | 1/30 |
| CATS | DFKGD | NEQFFGPGTRLTVL | 2S1 | 1/30 |
| CATS | VAGGD | EQFFGPGTRLTVL | 2S1 | 1/30 |
| CATS | TDRGH | GDTQYFGPGTRLTVL | 2S3 | 1/30 |
| CATS | VRVG | DEQFFGPGTRLTVL | 2S1 | 1/30 |
| CAT | LELAGS | YNEQFFGPGTRLTVL | 2S1 | 1/30 |
| CAT | RR | TGLDFGAGTRLSVL | 1/30 | |
| CATS | DPTSGI | YNEQFFGPGTRLTVL | 2S1 | 1/30 |
| CAT | RGTGS | NTEAFFGQGTRLTVV | 1S1 | 1/30 |
| CATS | DRTS | GANVLTFGAGSRLTVL | 2S6 | 1/30 |
| CATS | TRHAG | TGELFFGEGSRLTVL | 2S2 | 1/30 |
| CATS | DGHVG | QETQYFGPGTRLLVL | 2S5 | 1/30 |
| CATS | DASGRI | EQFFGPGTRLTVL | 2S1 | 1/30 |
| CATS | DGVS | GDTQYFGPGTRLTVL | 2S3 | 1/30 |
| CATS | VHAGS | QETQYFGPGTRLLVL | 2S5 | 1/30 |
| CATS | GPH | NTEAFFGQGTRLTVV | 1S1 | 1/30 |
| CATS | RSVG | NEQFFGPGTRLTVL | 2S1 | 1/30 |
| CATS | DHVSLE | GDTQYFGPGTRLTVL | 2S3 | 1/30 |
| CATS | QYLAGS | TGELFFGEGSRLTVL | 2S2 | 1/30 |
| CATS | APSHG | YNEQFFGPGTRLTVL | 2S1 | 1/30 |
| CATS | EWKDHSA | YNEQFFGPGTRLTVL | 2S1 | 1/30 |
| Normal 2 | ||||
| CATS | RAKG | ETQYFGPGTRKKVL | 2S5 | 2/26 |
| CATS | AEGSG | TQYFGPGTRLTVL | 2S3 | 2/26 |
| CATS | AEAGSPS | GANVLTFGAGSRLTVL | 2S6 | 2/26 |
| CATS | DPDR | YQETQYFGPGTRLLVL | 2S5 | 2/26 |
| CATS | EAGID | GANVLTFGAGSRLTVL | 2S6 | 1/26 |
| CATS | DASGRI | EQFFGPGTRLTVL | 2S1 | 1/26 |
| CATS | IPNQ | ALQPHFGDGTRLSIL | 1S5 | 1/26 |
| CATS | DYGTGG | YNEQFFGPGTRLTVL | 2S1 | 1/26 |
| CATS | YFWRIP | YNEQFFGPGTRLTVL | 2S1 | 1/26 |
| CATS | DHGQGE | ETQYFGPGTRLLVL | 2S5 | 1/26 |
| CATS | DYRS | GEQYFGPGTRLTV | 2S5 | 1/26 |
| CATS | DRAG | TDTQYFGPGTRLTVL | 2S3 | 1/26 |
| CATS | DRAG | TDTQYFGPGTRLTVL | 2S3 | 1/26 |
| CATS | DSGTSIG | TQYFGPGTRLLVL | 2S3 | 1/26 |
| CATS | DGGTA | EQFFGPGTRLTVL | 2S1 | 1/26 |
| CATS | AKGTV | ALQPHFGDGTRLSIL | 1S5 | 1/26 |
| CATS | RGDTA | GANVLTFGAGSRLTVL | 2S6 | 1/26 |
| CATS | DKQSG | ETQYFGPGTRKKVL | 2S5 | 1/26 |
| CATS | VGKAP | EQFFGPGTRLTVL | 2S1 | 1/26 |
| CATS | DAGSTWS | YNEQFFGPGTRLTVL | 2S1 | 1/26 |
| CATS | DGSHK | GANVLTFGAGSRLTVL | 2S6 | 1/26 |
| CATS | SGPG | TQYFGPGTRLLVL | 2S3 | 1/26 |
| CATS | DLHK | TQYFGPGTRLLVL | 2S3 | 1/26 |
| Normal 3 | ||||
| CATS | DGHQ | ETQYFGPGTRLLVL | 2S5 | 1/20 |
| CAT | GATG | TDTQYFGPGTRLTVL | 2S3 | 1/20 |
| CATS | DNRAS | DTQYFGPGTRLTVL | 2S3 | 1/20 |
| CATS | EGSY | YGYTFGSGTRLTVL | 1/20 | |
| CATS | DPRPGG | TDTQYFGPGTRLTVL | 2S3 | 1/20 |
| CATS | DSVSS | YNEQFFGPGTRL | 2S1 | 1/20 |
| CATS | DPYH | EQFFGPGTRLTVL | 2S1 | 1/20 |
| CATS | DIGT | TDTQYFGPGTRLTVL | 2S3 | 1/20 |
| CATS | LGASTS | YNEQFFGPGTRLTVL | 2S1 | 1/20 |
| CATS | DWVGMRSGKP | NEQFFGPGTRLTVL | 2S1 | 1/20 |
| CATS | DLF | EAFFGQGTRLTVV | 1S1 | 1/20 |
| CATS | DPPG | NEQFFGPGTRLTVL | 2S1 | 1/20 |
| CAT | RARQGGS | EQFFGPGTRLTVL | 2S1 | 1/20 |
| CAT | PRTSGAPT | EQFFGPGTRLTVL | 2S1 | 1/20 |
| CATS | DSRHTSGS | EQFFGPGTRLTVL | 2S1 | 1/20 |
| CATS | DGQGAHDA | EAFFGQGTRLTVV | 1S1 | 1/20 |
| CATS | DAGGD | QPQHFGDGTRLSIL | 1S5 | 1/20 |
| CATS | EPTGNPN | QPQGFGDGTRLSIL | 1S5 | 1/20 |
| CATS | DTGTG | TDTQYGPGTRLTVL | 2S3 | 1/20 |
| CATS | GRDWSS | YNEQFFGPGTRLTVL | 2S1 | 1/20 |
Junctional Amino Acid Sequences of TCR BV15 From CyA-Dependent AA Patients
| Subject No. . | ||||
|---|---|---|---|---|
| BV15 . | N-D-N . | BJ . | . | Frequency . |
| Patient 5 | ||||
| CATS | DLTSGP | NTGELFFGEGSRLTVL | 2S2 | 21/30 |
| CATS | DLRLAG | YTDTQYEGPGTRLTVL | 2S3 | 3/30 |
| CATS | DPDR | YQETQYFGPGTRLLVL | 2S5 | 3/30 |
| CATS | AAGGT | YNEQFFGPGTRLTVL | 2S1 | 1/30 |
| CATS | DRPDS | EQFFGPGTRLTVL | 2S1 | 1/30 |
| CATS | DASGRI | EQFFGPGTRLTVL | 2S1 | 1/30 |
| Patient 6 | ||||
| CATG | GSP | QETQYFGPGTRLLVL | 2S5 | 14/38 |
| CATS | EPTGAN | TGELFFGEGSRLTVL | 2S2 | 3/38 |
| CATS | EAGID | GANVLTFGAGSRLTVL | 2S6 | 3/38 |
| CATS | DAGTSG | ETQYFGPGTRLLVL | 2S5 | 2/38 |
| CAA | QGAPH | QPQHFGDGTRLSIL | 1S5 | 2/38 |
| CATT | ESRSG | TDTQYFGPGTRLTVL | 2S3 | 2/38 |
| CATS | DRQ | TGELFFGEGSRLTVL | 2S2 | 2/38 |
| CATS | DLELY | TGELFFGEGSRLTVL | 2S2 | 2/38 |
| CATS | DQRDL | GELFFGEGSRLTVL | 2S2 | 1/38 |
| CATS | DPGIL | YNEQFFGPGTRLTVL | 2S1 | 1/38 |
| CATS | DPSGA | YNEQFFGPGTRLTVL | 2S1 | 1/38 |
| CATS | DRLAEA | YNEQFFGPGTRLTVL | 2S1 | 1/38 |
| CATR | QGHN | EQFFGPGTRLTVL | 2S1 | 1/38 |
| CATS | DPGIL | YNEQFFGPGTRLTVL | 2S1 | 1/38 |
| CATS | AQTGS | YNEQFFGPGSRLTVL | 2S1 | 1/38 |
| CATS | GPLS | QETQYFGPGTRLLVL | 2S5 | 1/38 |
| Patient 7 | ||||
| CATS | PRDRR | NTGELFLGEGSRLTVL | 2S2 | 18/30 |
| CATS | RGGTSV | NTGELFFGEGSRLTVL | 2S2 | 2/30 |
| CATS | DTTSG | YNEQFFGPGTRLTVL | 2S1 | 2/30 |
| CA | TRGRGP | TGELFFGEGSRLTVL | 2S2 | 2/30 |
| CATS | DPGRP | YNEQFFGPGTRLTVL | 2S1 | 1/30 |
| CATS | GPGG | QETQYFGPGTRLLVL | 2S5 | 1/30 |
| CATS | NPGA | TDTQYFGPGTRLTVL | 2S3 | 1/30 |
| CATS | DSPGLGR | YNEQFFGPGTRLTVL | 2S1 | 1/30 |
| CATS | DSQGSA | DTQYFGPGTRLTVL | 2S3 | 1/30 |
| CATS | SPPS | YNEQFFGPGTRLTVL | 2S1 | 1/30 |
| Patient 8 | ||||
| CATS | DLTNGP | NTGELFFGEGSRLTVL | 2S2 | 7/40 |
| CATS | DRTWS | EQFFGPGTRLTVL | 2S1 | 6/40 |
| CAT | D | SYNEQFFGPGTRLTVL | 2S1 | 5/40 |
| CATS | DPS | STDTQYFGPGTRLTVL | 2S3 | 5/40 |
| CATS | DFSA | STDTQYFGPGTRLTVL | 2S3 | 4/40 |
| CATS | PGG | SYEQYFGPGTRLTVT | 2S7 | 3/40 |
| CATS | TG | SYEQYFGPGTRLTVT | 2S7 | 2/40 |
| CATS | DFTGRGH | NEQFFGPGTRLTVL | 2S1 | 1/40 |
| CATS | DSW | NEQFFGPGTRLTVL | 2S1 | 1/40 |
| CATS | DMDTRTG | NTEAFFGQGTRLTVV | 1S1 | 1/40 |
| CATS | DMDTG | NTEAFFGQGTRLTVV | 1S1 | 1/40 |
| CATS | DLQFG | QTETQYFGPGTRLLVL | 2S5 | 1/40 |
| CATS | DPGTGY | NQPQHFGPGTRLSIL | 1S5 | 1/40 |
| CATS | DAGVE | EQFFGPGTRLTVL | 2S1 | 1/40 |
| CATS | DRPRTG | NEQFFGPGTRLTVL | 2S1 | 1/40 |
| Patient 9 | ||||
| CATS | DESY | EQFFGPGTRLTVL | 2S1 | 7/18 |
| CATS | DLRES | NEQFFGPGTRLTVL | 2S1 | 4/18 |
| CATS | VAGSG | ETQYFGPGTRLLVL | 2S5 | 3/18 |
| CATS | DAGTSG | ETQYFGPGTRLLVL | 2S5 | 2/18 |
| CATS | GEG | SDTQYFGPGTRLTVL | 2S3 | 2/18 |
| Subject No. . | ||||
|---|---|---|---|---|
| BV15 . | N-D-N . | BJ . | . | Frequency . |
| Patient 5 | ||||
| CATS | DLTSGP | NTGELFFGEGSRLTVL | 2S2 | 21/30 |
| CATS | DLRLAG | YTDTQYEGPGTRLTVL | 2S3 | 3/30 |
| CATS | DPDR | YQETQYFGPGTRLLVL | 2S5 | 3/30 |
| CATS | AAGGT | YNEQFFGPGTRLTVL | 2S1 | 1/30 |
| CATS | DRPDS | EQFFGPGTRLTVL | 2S1 | 1/30 |
| CATS | DASGRI | EQFFGPGTRLTVL | 2S1 | 1/30 |
| Patient 6 | ||||
| CATG | GSP | QETQYFGPGTRLLVL | 2S5 | 14/38 |
| CATS | EPTGAN | TGELFFGEGSRLTVL | 2S2 | 3/38 |
| CATS | EAGID | GANVLTFGAGSRLTVL | 2S6 | 3/38 |
| CATS | DAGTSG | ETQYFGPGTRLLVL | 2S5 | 2/38 |
| CAA | QGAPH | QPQHFGDGTRLSIL | 1S5 | 2/38 |
| CATT | ESRSG | TDTQYFGPGTRLTVL | 2S3 | 2/38 |
| CATS | DRQ | TGELFFGEGSRLTVL | 2S2 | 2/38 |
| CATS | DLELY | TGELFFGEGSRLTVL | 2S2 | 2/38 |
| CATS | DQRDL | GELFFGEGSRLTVL | 2S2 | 1/38 |
| CATS | DPGIL | YNEQFFGPGTRLTVL | 2S1 | 1/38 |
| CATS | DPSGA | YNEQFFGPGTRLTVL | 2S1 | 1/38 |
| CATS | DRLAEA | YNEQFFGPGTRLTVL | 2S1 | 1/38 |
| CATR | QGHN | EQFFGPGTRLTVL | 2S1 | 1/38 |
| CATS | DPGIL | YNEQFFGPGTRLTVL | 2S1 | 1/38 |
| CATS | AQTGS | YNEQFFGPGSRLTVL | 2S1 | 1/38 |
| CATS | GPLS | QETQYFGPGTRLLVL | 2S5 | 1/38 |
| Patient 7 | ||||
| CATS | PRDRR | NTGELFLGEGSRLTVL | 2S2 | 18/30 |
| CATS | RGGTSV | NTGELFFGEGSRLTVL | 2S2 | 2/30 |
| CATS | DTTSG | YNEQFFGPGTRLTVL | 2S1 | 2/30 |
| CA | TRGRGP | TGELFFGEGSRLTVL | 2S2 | 2/30 |
| CATS | DPGRP | YNEQFFGPGTRLTVL | 2S1 | 1/30 |
| CATS | GPGG | QETQYFGPGTRLLVL | 2S5 | 1/30 |
| CATS | NPGA | TDTQYFGPGTRLTVL | 2S3 | 1/30 |
| CATS | DSPGLGR | YNEQFFGPGTRLTVL | 2S1 | 1/30 |
| CATS | DSQGSA | DTQYFGPGTRLTVL | 2S3 | 1/30 |
| CATS | SPPS | YNEQFFGPGTRLTVL | 2S1 | 1/30 |
| Patient 8 | ||||
| CATS | DLTNGP | NTGELFFGEGSRLTVL | 2S2 | 7/40 |
| CATS | DRTWS | EQFFGPGTRLTVL | 2S1 | 6/40 |
| CAT | D | SYNEQFFGPGTRLTVL | 2S1 | 5/40 |
| CATS | DPS | STDTQYFGPGTRLTVL | 2S3 | 5/40 |
| CATS | DFSA | STDTQYFGPGTRLTVL | 2S3 | 4/40 |
| CATS | PGG | SYEQYFGPGTRLTVT | 2S7 | 3/40 |
| CATS | TG | SYEQYFGPGTRLTVT | 2S7 | 2/40 |
| CATS | DFTGRGH | NEQFFGPGTRLTVL | 2S1 | 1/40 |
| CATS | DSW | NEQFFGPGTRLTVL | 2S1 | 1/40 |
| CATS | DMDTRTG | NTEAFFGQGTRLTVV | 1S1 | 1/40 |
| CATS | DMDTG | NTEAFFGQGTRLTVV | 1S1 | 1/40 |
| CATS | DLQFG | QTETQYFGPGTRLLVL | 2S5 | 1/40 |
| CATS | DPGTGY | NQPQHFGPGTRLSIL | 1S5 | 1/40 |
| CATS | DAGVE | EQFFGPGTRLTVL | 2S1 | 1/40 |
| CATS | DRPRTG | NEQFFGPGTRLTVL | 2S1 | 1/40 |
| Patient 9 | ||||
| CATS | DESY | EQFFGPGTRLTVL | 2S1 | 7/18 |
| CATS | DLRES | NEQFFGPGTRLTVL | 2S1 | 4/18 |
| CATS | VAGSG | ETQYFGPGTRLLVL | 2S5 | 3/18 |
| CATS | DAGTSG | ETQYFGPGTRLLVL | 2S5 | 2/18 |
| CATS | GEG | SDTQYFGPGTRLTVL | 2S3 | 2/18 |
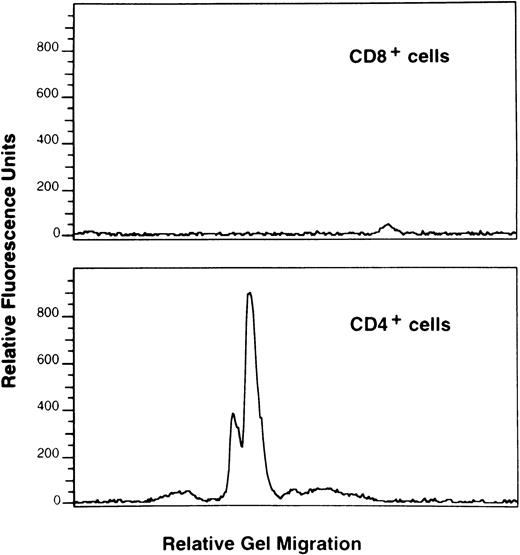
Phenotype of the predominant BV15+ T-cell clone in patient no. 5.
To characterize the BV15+ T-cell clone with the CDR3 sequence of DLTSGP in patient no. 5, CD4+ and CD8+ cells were sorted from the patient’s BMMCs, cDNA derived from each T-cell population was amplified using a primer specific to BV15 coupled with a BC primer, and the amplified products were submitted to primer extension using the fluorescent clonotypic primer specific to the CDR3 sequence. A discernible peak of fluorescence was detected only in CD4+ cells, indicating that the T cells bearing BV15 with this sequence were CD4+(Fig 6).
Phenotype of BV15+ T-cell clone with CDR3 sequence of DLTSGP in patient no. 5. cDNA derived from CD4+ and CD8+ T cells of BM from patient no. 5 was amplified using a primer specific to BV15 coupled with a BC primer, and the amplified products were submitted to primer extension using the fluorescent clonotypic primer containing the DLTSGP motif. Amplified BV15 cDNA was analyzed for size with the gene scan program.
Phenotype of BV15+ T-cell clone with CDR3 sequence of DLTSGP in patient no. 5. cDNA derived from CD4+ and CD8+ T cells of BM from patient no. 5 was amplified using a primer specific to BV15 coupled with a BC primer, and the amplified products were submitted to primer extension using the fluorescent clonotypic primer containing the DLTSGP motif. Amplified BV15 cDNA was analyzed for size with the gene scan program.
DISCUSSION
The present analysis of the T-cell repertoire in the BM of AA patients treated with immunosuppressive therapy reveals several new findings regarding the role of T cells in the pathophysiology of AA. We expected that for patients no. 1 to 13 the BM would exhibit more or less abnormality in the T-cell repertoire, since all of them had shown a relative lymphocytosis in the BM and eventually improved with CyA or ATG, both of which selectively inhibit T-cell function. However, in addition to the patients who were refractory to CyA therapy (patients no. 14 to 18), neither the patients who obtained unmaintained remission early after CyA therapy nor those who responded to ATG after treatment failure with CyA exhibited an apparently high frequency of CDR3 size abnormalities suggestive of clonal predominance as compared with normal individuals. The results are in agreement with reports by Melenhorst et al.33 and Manz et al.34documenting that BV families of BM T cells from AA patients are predominantly polyclonal. Although it cannot be excluded that a small expansion of T cells within limited BV families contributes to suppression of hematopoiesis, it seems unlikely that antigen-driven T-cell expansion plays an essential role in the pathophysiology of AA in these patients. BM aplasia in these patients may have been caused instead by polyclonal T-cell activation leading to excessive production of myelosuppressive cytokines such as interferon gamma7,35and tumor necrosis factor.35 In ATG-responsive patients who were refractory to CyA, immunostimulatory effects rather than immunosuppressive effects of ATG may have worked to improve hematopoietic function.36
In contrast to the above two patient groups that responded to immunosuppressive therapy, the frequency of BV families with abnormal CDR3 size patterns was apparently higher in CyA-dependent AA patients versus normal controls. Forty-one percent to 75% of BV subfamilies exhibited CDR3 size patterns with a decreased peak number and/or skewed shape suggestive of clonal predominance. Although all of the CyA-dependent AA patients shared HLA-DRB1*1501, the abnormal CDR3 patterns were not due to the physiologic skewing associated with the particular HLA-DRB1 allele, because CDR3 patterns of three normal individuals possessing this DRB1 allele were not skewed.37The abnormal CDR3 size pattern of patient no. 5 is not attributable to his age as previously reported, since it was no longer detected after the patient achieved unmaintained remission after 4 years of CyA therapy.38 Moreover, abnormal CDR3 size patterns could not be corrected by long-term CyA therapy in patient no. 8, who still depended on CyA more than 7 years after therapy. It is possible that the skewed T-cell repertoire is not involved in the pathogenesis of CyA-dependent AA, but is only the consequence of the AA disease process. However, the disappearance and persistence of clonal predominance associated with each disease activity of patients no. 5 and 8 strongly suggest that clonally proliferating T cells play a role in the development of CyA-dependent AA. In this particular subset of AA patients, some antigens that elicit proliferation of a limited number of T cells may persist in the BM, and resultant antigen-specific T cells may inhibit hematopoiesis directly or indirectly via secretion of myelosuppressive cytokines.
In support of this hypothesis is the high homology between patients no. 5 and 8 for the CDR3 motif of the most dominant BV15+T-cell clone in the BM. The deduced amino acid sequence of the N-D-N region differed for patient no. 5 (DLTSGP) versus patient no. 8 (DLTNGP) by only one amino acid. Such similarities within the hypervariable region of the β chain of T cells in different patients have been demonstrated in other immune-mediated diseases, including multiple sclerosis16,18 and sarcoidosis.39 In multiple sclerosis patients, an LR motif in the VDJ region was shared by T cells infiltrating the brain tissue of different patients and by T cells reacting to the myelin basic protein.16 Similarly, an RJR sequence was detected in T cells in the bronchoalveolar lavage fluid from different patients with sarcoidosis.39 However, the high homology of the CDR3 motif covering the whole CDR3 sequence as detected in patients no. 5 and 8 has never been demonstrated in any T-cell–mediated diseases of undefined etiology. It has been established that the CDR3 motif of TCR BV corresponds to an epitope structure of the target peptide. In viral infections, T-cell clones with the same CDR3 motif have been shown to proliferate and persist in different patients.40 Hence, the two T-cell clones expressing BV15 with the similar CDR3 motif probably recognize a common peptide that is possibly related to the pathophysiology of AA.
AA patients possessing HLA-DRB1*1501 form a distinct subset of immune-mediated AA cases. This subset is likely to improve with CyA but also to relapse in association with a dose reduction of CyA, and therefore immune mechanisms through T cells most likely operate in these patients.23 The frequency of AA patients requiring continuous CyA therapy among all AA patients is estimated to be approximately 15% based on our experience of CyA therapy for 40 patients with AA (S.N., unpublished observation, November 1998). It is tempting to hypothesize that some antigens that are likely to be presented by HLA-DR15 sensitize CD4+T cells to attack hematopoietic cells in these patients. The fact that the PCR using a clonotypic primer complementary to the CDR3 sequence of DLTSGP only amplified the cDNA of CD4+ T cells in patient no. 5 supports this hypothesis. We recently isolated the CD4+ T-cell clone with this CDR3 motif from the BM of patient no. 5. Although this clone showed a proliferative response to autologous BMMCs containing antigen-presenting cells, it did not respond to purified CD34+ cells (data not shown). Since it is possible that the CD4+ T-cell clone may recognize a peptide derived from hematopoietic progenitors that can be presented by antigen-presenting cells, we are currently screening a peptide library to identify the target molecule of the T cells.
The present study reveals heterogeneity in the immune mechanisms of AA for the first time. The finding that antigen-driven expansion of T cells is primarily involved in the pathophysiology of a limited number of cases characterized by a repetitive response to CyA therapy and HLA-DRB1*1501 is of significance to basic studies on the immune mechanisms of AA. This subset of AA is considered a suitable subject of epidemiologic and immunologic approaches to identify the etiologic mechanisms of AA. The results of this study also appear to be of significance in choosing appropriate therapy for AA: patients displaying abnormal CDR3 size patterns in greater than 40% of BV families are likely to benefit from CyA therapy but will probably require long-term treatment with the immunosuppressive agent. Characterization of the T-cell repertoire in the BM as in the present study may facilitate individualized therapy depending on the immune mechanism of each AA patient.
Supported by a Grant-in-Aid for Scientific Research from the Ministry of Education, Science and Culture, Japan (08671223), and a Grant-in-Aid for Immunologic Research for Intractable Diseases from the Ministry of Health and Welfare, Japan.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to Shinji Nakao, MD, Third Department of Medicine, Kanazawa University School of Medicine, 13-1 Takaramachi, Kanazawa, Ishikawa 920-8641, Japan; e-mail: snakao@med.kanazawa-u.ac.jp.