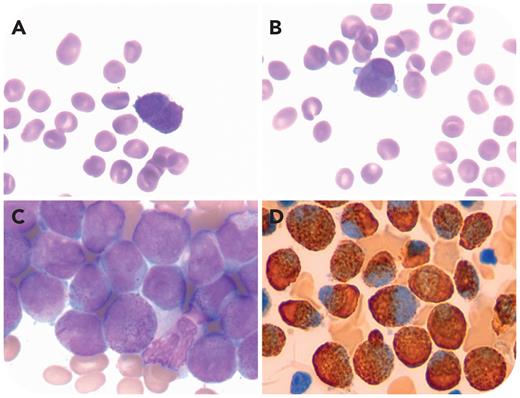
A 55-year-old woman presented with a 1-day history of dizziness; white blood cell count, 3.2 × 109/L; hemoglobin concentration, 66 g/L; platelet count, 13 × 109/L; prothrombin time, 9.9 seconds; activated partial thromboplastin time, 23.9 seconds; and fibrinogen level, 1.52 g/L. The blood film showed 45% abnormal cells with hypergranular cytoplasm and irregular nuclei (panels A-B; Wright-Giemsa stain, 100× objective). Bone marrow aspirate films showed 69% abnormal cells with prominent hypergranular cytoplasm and kidney-shaped or bilobed nuclei, suggesting acute promyelocytic leukemia (APL). Auer rods and faggot cells were seen (panel C; Wright-Giemsa stain, 100× objective). Myeloperoxidase was strong positive (panel D; myeloperoxidase stain, 100× objective). Flow cytometry analysis showed side scatter of these promyelocytes was high. Moreover, 80.37% promyelocytes were positive for CD117, CD13 (moderate), CD33, CD123, CD99, myeloperoxidase (bright), CD64 (moderate), and CD56 (partial), and were negative for CD34, human leukocyte antigen-DR, CD19, cytoplasmic (c)CD3, and cCD79a. However, the diagnosis of APL was ruled out by the absence of the PML::RARA gene fusion detected by real-time polymerase chain reaction, the absence of PML::RARA gene fusion, as detected by fluorescence in situ hybridization, and normal karyotype (46, XX)[20]. Next-generation sequencing identified mutations in GATA2 and WT1.
Finally, a diagnosis of acute myeloid leukemia with GATA2 and WT1 mutations was made.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit https://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal