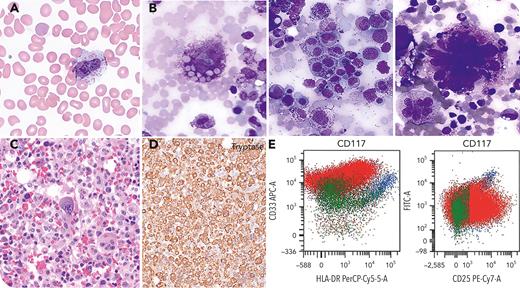
A 63-year-old man presented with fever, splenomegaly, hyperferritinemia (10 798 ng/dL), elevated soluble interleukin-2R (6644 pg/mL), anemia (hemoglobin 6.9 g/dL), and thrombocytopenia (42 000/μL). Atypical cells were seen on the blood smear (panel A; Wright-Giemsa stain, 50× objective). Bone marrow aspirate showed large pleomorphic tumor cells with metachromatic granules and hemophagocytosis (panel B; Wright-Giemsa stain, 40× objective). Bone marrow biopsy showed a destructive growth pattern (panel C; hematoxylin and eosin stain, 40× objective) with tumor cells expressing tryptase and CD30 (panel D; tryptase stain, 10× objective). Flow cytometry showed aberrant expression of CD25 and negative CD2 (panel E). Serum tryptase was elevated (>200 μg/L) and clinically significant alterations were detected in the KIT and TP53 genes. The patient was diagnosed with mast cell sarcoma and met criteria for hemophagocytic lymphohistocytosis.
Mast cell sarcoma is an aggressive neoplasm with a poor clinical outcome. A diagnosis of mast cell sarcoma is challenging due to unusual symptoms with frequent marrow involvement, pleomorphic morphology, and immunophenotype that overlaps with other more common hematologic neoplasms. Degree of high-grade cytology with localized invasive growth pattern distinguishes mast cell leukemia from mast cell sarcoma. An in-frame deletion in the KIT gene (D419del) was detected in this patient. The incidence of the canonical KIT D816V mutation in mast cell sarcoma is low when compared with other subtypes of systemic mastocytosis, although it can harbor other KIT mutations.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit https://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal