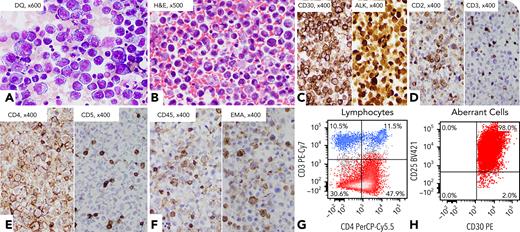
A 42-year-old woman with a history of marginal zone lymphoma (8 years ago) with diffuse large B-cell lymphoma transformation (4 years ago) was admitted with shortness of breath, bilateral pleural effusions, and ascites. A paracentesis of ascites was performed, and cytology smears showed many large-sized atypical cells with abundant basophilic cytoplasm and cytoplasmic vacuoles, resembling erythroblasts (panel A; objective 600×). Cell block hematoxylin and eosin staining showed numerous large atypical cells, some having horseshoe-like nuclei (panel B; objective 500×). By immunohistochemistry, the neoplastic cells were positive for CD30, anaplastic lymphoma kinase (ALK) (nuclear and cytoplasmic, indicating ALK rearrangement, likely NPM1::ALK translocation), CD2 (partial), CD4, CD45 (subset), and epithelial membrane antigen (subset), whereas they were negative for CD3, CD5, CD19, paired box 5, CD138, Epstein-Barr virus–encoded small RNA, and human herpesvirus 8 (panels C-F; objective 400×). Flow cytometric analysis showed no monotypic B cells; instead, a large population of aberrant T cells was detected: positive for CD4, CD25, and CD30, and negative for CD3, CD5, CD7, and CD8 (panels G-H). She was diagnosed with ALK-positive anaplastic large-cell lymphoma (ALK+ ALCL), which was later confirmed with lymph node involvement.
ALK+ ALCL with erythroblast-like cytology first diagnosed in body fluid is highly unusual, especially in a patient with a previous history of B-cell lymphomas. Lack of history of ALCL with such an unusual morphology is diagnostically challenging. Careful morphologic examination and extensive immunophenotypic workup are critical in reaching the correct diagnosis.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit https://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal