Abstract
The central nervous system (CNS) is the most important site of extramedullary disease in adults with acute lymphoblastic leukemia (ALL). Although CNS disease is identified only in a minority of patients at the time of diagnosis, subsequent CNS relapses (either isolated or concurrent with other sites) occur in some patients even after the delivery of prophylactic therapy targeted to the CNS. Historically, prophylaxis against CNS disease has included intrathecal (IT) chemotherapy and radiotherapy (RT), although the latter is being used with decreasing frequency. Treatment of a CNS relapse usually involves intensive systemic therapy and cranial or craniospinal RT along with IT therapy and consideration of allogeneic hematopoietic cell transplant. However, short- and long-term toxicities can make these interventions prohibitively risky, particularly for older adults. As new antibody-based immunotherapy agents have been approved for relapsed/refractory B-cell ALL, their use specifically for patients with CNS disease is an area of keen interest not only because of the potential for efficacy but also concerns of unique toxicity to the CNS. In this review, we discuss data-driven approaches for these common and challenging clinical scenarios as well as highlight how recent findings potentially support the use of novel immunotherapeutic strategies for CNS disease.
Introduction
In adults with acute lymphoblastic leukemia (ALL), the incidence of central nervous system (CNS) involvement at the time of diagnosis has ranged from 5% to 11% in the largest clinical trials of the last 25 years (Table 1).1-6 The MRC UKALL12/ECOG 2993 trial found that this was associated with an inferior overall survival (OS), with a 5-year OS of 29% for those with CNS disease at diagnosis vs 38% for those without.5 CNS disease is likely present but undetectable in some patients at diagnosis. Without CNS-directed prophylaxis, the rates of CNS relapse range from 30% to 40%, justifying the routine use of CNS-directed prophylaxis as a standard component in ALL management since the 1980s.7,8 With modern prophylaxis techniques, rates of CNS relapses range from 4% to 15%1,9,10; these relapses can either be isolated to the CNS or combined with other sites. Data from the French Groupe d'Etude et de Traitement de la Leucémie Aiguë Lymphoblastique de l'Adulte (GET-LALA) describe a CNS relapse rate of 15% across 2 large adult trials, with ∼75% of these CNS relapses combined with other sites, and 25% isolated to the CNS.9 Historically, outcomes for adults after CNS relapse are poor, with a median OS of <1 year.11
Examples of common regimens used for adults with ALL, schedule of CNS-directed therapy, and rates of relapse in the CNS
| Study . | Enrollment period . | CNS involvement at diagnosis (%) . | CNS-directed therapy . | CNS relapse rates (%) . |
|---|---|---|---|---|
| Hyper-CVAD1 | 1992-1998 | 7 | CNS-negative: between 4-16 doses of IT chemotherapy (alternating MTX and ARA-C) over ∼6 mo, depending on risk category∗ CNS-positive: twice weekly IT chemotherapy until CSF cleared (then IT prophylaxis per risk category), followed by remaining prophylaxis schedule plus 24-30 Gy cranial RT, if cranial nerve involvement Systemic therapy: dexamethasone, high-dose MTX, and high-dose ARA-C | 4 |
| MRC UKALL XII/ECOG E29932 | 1993-2003 | 5 | CNS-negative: IT MTX × 5 given through phase 2 (∼2 mo) CNS-positive: weekly IT MTX until CSF cleared plus 24 Gy cranial RT and 12 Gy spinal RT Systemic therapy: l-asparaginase, 6-MP, and high-dose MTX | 4 |
| GRAALL 20053 | 2006-2014 | 5 | CNS-negative: IT MTX × 1 in prephase; ITT × 6 through late intensification (∼6 mo) ± 18 Gy cranial RT† CNS-positive: ITT × 14 through first consolidation (∼2 mo) plus 15 to 24 Gy cranial RT† Systemic therapy: l-asparaginase, high-dose ARA-C, dexamethasone, high-dose MTX, and 6-MP | 5 |
| CALGB 104034 | 2007-2012 | 10.5 | CNS-negative: IT ARA-C × 1 and IT MTX × 11 during the first 4 courses (∼7 mo) of therapy, then continued during prolonged maintenance‡ CNS-positive: same total doses of IT chemotherapy but weekly during remission induction plus 18 Gy cranial RT Systemic therapy: pegaspargase, 6-MP, dexamethasone, and thioguanine | Not reported |
| Study . | Enrollment period . | CNS involvement at diagnosis (%) . | CNS-directed therapy . | CNS relapse rates (%) . |
|---|---|---|---|---|
| Hyper-CVAD1 | 1992-1998 | 7 | CNS-negative: between 4-16 doses of IT chemotherapy (alternating MTX and ARA-C) over ∼6 mo, depending on risk category∗ CNS-positive: twice weekly IT chemotherapy until CSF cleared (then IT prophylaxis per risk category), followed by remaining prophylaxis schedule plus 24-30 Gy cranial RT, if cranial nerve involvement Systemic therapy: dexamethasone, high-dose MTX, and high-dose ARA-C | 4 |
| MRC UKALL XII/ECOG E29932 | 1993-2003 | 5 | CNS-negative: IT MTX × 5 given through phase 2 (∼2 mo) CNS-positive: weekly IT MTX until CSF cleared plus 24 Gy cranial RT and 12 Gy spinal RT Systemic therapy: l-asparaginase, 6-MP, and high-dose MTX | 4 |
| GRAALL 20053 | 2006-2014 | 5 | CNS-negative: IT MTX × 1 in prephase; ITT × 6 through late intensification (∼6 mo) ± 18 Gy cranial RT† CNS-positive: ITT × 14 through first consolidation (∼2 mo) plus 15 to 24 Gy cranial RT† Systemic therapy: l-asparaginase, high-dose ARA-C, dexamethasone, high-dose MTX, and 6-MP | 5 |
| CALGB 104034 | 2007-2012 | 10.5 | CNS-negative: IT ARA-C × 1 and IT MTX × 11 during the first 4 courses (∼7 mo) of therapy, then continued during prolonged maintenance‡ CNS-positive: same total doses of IT chemotherapy but weekly during remission induction plus 18 Gy cranial RT Systemic therapy: pegaspargase, 6-MP, dexamethasone, and thioguanine | Not reported |
ARA-C, cytarabine; MTX, methotrexate; 6-MP, 6-mercaptopurine.
Patients were considered at high risk if LDH levels were >600 units per L or with a proliferative index >14%.
RT treatment was based on candidacy for HCT: patients who had CNS-negative results and were candidates for HCT were not given prophylactic RT, whereas patients who were not eligible for HCT received 18 Gy cranial RT; patients who had CNS-positive results and were candidates for HCT received 15 Gy cranial RT, whereas patients who were not eligible for HCT were given 24 Gy.
Patients with T-cell phenotype also received 24 Gy cranial RT during first maintenance cycle.
There have been few studies among adult patients focused on CNS disease; hence, some of the recommendations discussed herein are derived from pediatric studies. Furthermore, in part because of the relative paucity of clinical data, a diverse range of clinical practice patterns have emerged surrounding this topic. In this review, we attempt to highlight areas in which clinical trials and retrospective analyses have helped develop our approaches. Ultimately, our approaches have been shaped by the regimens used for different clinical scenarios at our center, a topic that is outside our scope here. It is not our intention to imply that these strategies are superior; instead, readers may take this information and apply it to their own practice or research, as feasible.
Pathophysiology, presentation, and diagnosis
The pathophysiology underlying CNS involvement in ALL is a complex process involving leukemic migration from the marrow space into the CNS (an immune-privileged space) and survival in the CNS microenvironment. Recent publications have highlighted unique mechanisms via which this occurs, including leukemic migration along the outside of emissary vessels, relying on α-integrin receptors similar to early neural progenitors.12 There is also leukemic metabolic adaptation to the CNS microenvironment to promote survival and proliferation.13 Although these studies have yet to affect current treatment practices, they have provided the rationale for ongoing clinical investigation by identifying targetable pathways (eg, phosphatidylinositol 3-kinase; #NCT04803123). Although a more in-depth discussion on this topic is beyond the scope of this article, several reviews provide a comprehensive overview of our current understanding of this process.14-17
Risk factors for CNS involvement at the time of diagnosis include high white blood cell (WBC) count (>30 000/μL in B-cell ALL [B-ALL] and >100 000/μL in T-cell ALL [T-ALL]), lactate dehydrogenase (LDH) >3 × the upper limit of normal (ULN), adverse-risk cytogenetics (including t[9;22] and t[4;11]), and T lineage.5,8,18,19 Risk factors for CNS relapse are similar, and include a history of CNS disease. Older measurements of proliferative index (eg, S + G2M phase), which were used to risk stratify patients in earlier trials, are no longer used commonly.1,18
Most patients with CNS disease are asymptomatic or mildly symptomatic at presentation. Neurologic manifestations can vary because the specific affected neuroanatomic structures can differ. For diagnosis, cerebrospinal fluid (CSF) is removed via lumbar puncture (LP). An LP is the minimum protocol needed to evaluate CNS involvement. We also obtain CNS imaging (typically magnetic resonance imaging with contrast) in patients with neurologic symptoms or signs, because CNS involvement in ALL can present with cranial nerve infiltration, leptomeningeal involvement, and/or (far less commonly) parenchymal lesions. Such involvement can also be complicated with the presence of CNS hemorrhage and/or elevated intracranial pressure, which could necessitate urgent surgical intervention and potentially lead to a risk of uncal herniation during LP.
In practice, the first LP is usually done on or around the time of the first scheduled intrathecal (IT) chemotherapy, unless the patient has neurologic findings that would prompt earlier diagnostics. Debate remains whether the first LP should not be performed until the patient no longer has circulating peripheral blasts, given the theoretical concern for CSF contamination. From pediatric experience, contamination of the first or second LP by blasts (via a traumatic LP) is associated with an inferior event-free survival (EFS).20,21 This emphasizes that an LP should always include IT chemotherapy, even before the presence of CNS leukemia is confirmed. Our practice, however, is to defer the first LP until there are no circulating blasts; traumatic LP in this context may not affect the outcome.22
Management of thrombocytopenia and coagulopathy when performing LPs in patients with ALL is controversial, with no prospective data to guide this practice. Retrospective data suggest that performing LPs on patients with platelet counts of <50 000/μL does not increase hemorrhagic complications but does increase traumatic LPs.23,24 Therefore, we recommend a correction level to be >50 000/μL, given the association of traumatic LPs with inferior outcomes among children.20,21 We also favor correcting coagulopathy around the time of an LP, again, because of its association with traumatic LP.25 An exception would be when these laboratory abnormalities are due to the presence of asparaginase, in which case, correction may increase the risk of thrombosis.26
Historically, the diagnosis of CNS leukemia relied on the microscopic examination of the CSF after centrifugation and Wright-Giemsa staining, a method known as conventional cytospin (CC). As a result, studies have largely focused on this method to distinguish between schedules of CNS-directed prophylaxis vs treatment. A grading system generated by the Children’s Oncology Group (COG) exists to quantify the degree of CNS involvement (Table 2). These categories correlated very closely with EFS and OS when validated in a cohort of >8000 pediatric patients.21 Recent studies have established multiparameter flow cytometry (MFC) as superior to CC, allowing for more sensitive detection of CNS leukemia and improved risk stratification for CNS relapse after treatment.19,22,27-29 However, these analyses did not present the survival differences between MFC and CC; MFC has limitations when cell counts are low, which is typical of CSF. Nonetheless, microscopic evaluation (either as a dichotomous “present” vs “absent” result or similar to that used by the COG) and/or MFC may be used for routine evaluation of CSF.
Grading of CNS disease per the COG classification system
| Grade of CNS disease at diagnosis . | Definition . |
|---|---|
| CNS-1 | No blasts in the CSF (regardless of WBC or RBC count in CSF) |
| CNS-2 | |
| a | <5 WBC per μL + blasts + <10 RBC per μL∗ |
| b | <5 WBC per μL + blasts + >10 RBC per μL |
| c | ≥5 WBC per μL + blasts + ≥10 RBC per μL; CSF WBC <2 × peripheral blood WBC |
| CNS-3 | |
| a | ≥5 WBC per μL + blasts + <10 RBC per μL |
| b | ≥5 WBC per μL + blasts + ≥10 RBC per μL; CSF WBC >2 × peripheral blood WBC |
| c | Clinical evidence of CNS disease† |
| Grade of CNS disease at diagnosis . | Definition . |
|---|---|
| CNS-1 | No blasts in the CSF (regardless of WBC or RBC count in CSF) |
| CNS-2 | |
| a | <5 WBC per μL + blasts + <10 RBC per μL∗ |
| b | <5 WBC per μL + blasts + >10 RBC per μL |
| c | ≥5 WBC per μL + blasts + ≥10 RBC per μL; CSF WBC <2 × peripheral blood WBC |
| CNS-3 | |
| a | ≥5 WBC per μL + blasts + <10 RBC per μL |
| b | ≥5 WBC per μL + blasts + ≥10 RBC per μL; CSF WBC >2 × peripheral blood WBC |
| c | Clinical evidence of CNS disease† |
Table adapted from Winick et al.21
Constitutes a traumatic LP.
Includes cranial nerve palsies or other overt neurologic deficits not attributable to other causes.
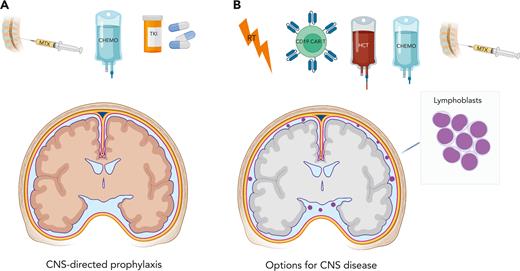
Next, we use 4 clinical cases to explore common scenarios that pertain to the prevention and treatment of CNS disease in adults with ALL (Figure 1).
Modalities for CNS prophylaxis and treatment of active CNS disease. (A) In most patients, there is no evidence of CNS disease at diagnosis. Here, prevention of CNS relapse depends primarily on IT therapy (most commonly with MTX) and CNS-penetrating systemic therapy (traditional cytotoxic chemotherapy [CHEMO] as well as the ABL TKI dasatinib, the latter for use in Ph+ disease). (B) In cases of overt CNS disease at diagnosis or of a CNS relapse, many of the same tools used in the prophylaxis setting, such as IT and systemic chemotherapy, are used. Additional tools include RT, CD19 CAR-modified T-cells, and consolidative HCT. Figure created with BioRender.com.
Modalities for CNS prophylaxis and treatment of active CNS disease. (A) In most patients, there is no evidence of CNS disease at diagnosis. Here, prevention of CNS relapse depends primarily on IT therapy (most commonly with MTX) and CNS-penetrating systemic therapy (traditional cytotoxic chemotherapy [CHEMO] as well as the ABL TKI dasatinib, the latter for use in Ph+ disease). (B) In cases of overt CNS disease at diagnosis or of a CNS relapse, many of the same tools used in the prophylaxis setting, such as IT and systemic chemotherapy, are used. Additional tools include RT, CD19 CAR-modified T-cells, and consolidative HCT. Figure created with BioRender.com.
Case 1
A 54-year-old woman presented with pancytopenia, with a WBC count of 1300/μL and an LDH level of 372 units per L (ULN: 210 units per L). A bone marrow exam showed B lymphoblasts representing 80% of cellularity. Fluorescence in situ hybridization showed negative results for the BCR::ABL1 fusion. An LP was performed, and the following data were recorded: 9 red blood cells (RBCs) per μL, 2 nucleated cells per μL, and no blasts on CC (CNS-1) or MFC.
What is your standard approach to CNS-directed prophylaxis in an adult with newly diagnosed Philadelphia chromosome–negative (Ph−) B-ALL without CNS involvement?
Like most adults at diagnosis, this patient has no detectable CNS disease. At our center, the standard approach for this patient would be administering hyper-CVAD (hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone alternating with high-dose methotrexate and cytarabine), although there are many acceptable regimens (Table 1). In most regimens, the schedule of IT therapy differs depending on whether CNS disease is present.
All adult ALL regimens include varying combinations of CNS-penetrating systemic agents plus other CNS-directed therapies. Agents that cross the blood-brain barrier (BBB) include methotrexate, cytarabine, dexamethasone, asparaginase, 6-mercaptopurine, and dasatinib. High-dose methotrexate is included in many adult regimens. The COG AALL0232 in children and young adults with B-ALL showed that interim maintenance based on high-dose methotrexate (5000 mg/m2) yielded superior EFS with CNS relapse rates below historical values (<5%).30 However, the parallel COG AALL0434 study among patients with T-ALL showed that Capizzi escalating dose methotrexate (100-300 mg/m2) plus pegaspargase interim maintenance provides superior disease-free survival and significantly fewer isolated CNS relapses (0.4% vs 3.0% for high-dose methotrexate).31 Thus, when multiple CNS-penetrating agents are used, high-dose methotrexate per se may not be critical.
These CNS-penetrating systemic agents found in adult ALL regimens are augmented by other CNS-directed prophylaxis. Although the specifics may vary; all of them include IT methotrexate at varying doses and frequencies (Table 1). Hyper-CVAD is unique because the protocol alternates between IT methotrexate and cytarabine, and it risk stratifies patients based on the presenting WBC and LDH levels. Using data from 2 Hyper-CVAD–based studies,1,32 we devised the following approach, which yields relatively low CNS relapse rates (∼5%):22 in patients without CNS disease, we administer 8 IT treatments to patients with neither WBC levels >30 000/μL nor LDH levels >3 × ULN (ie, low risk) vs 10 IT treatments when either of these characteristics exist. For patients treated with other regimens, we recommend adhering to the protocol-specific guidelines for CNS-directed prophylaxis.
Importantly, most adult regimens do not include radiotherapy (RT) for those without CNS disease at diagnosis. Historically, cranial RT (usually as a dose between 18 and 24 Gy) and IT therapy were fundamental for the treatment of CNS-directed prophylaxis. Concerns arising from the pediatric community surrounding the delayed toxicity of cranial RT, including neurocognitive defects, endocrinopathy, and secondary cancers, generated evidence that RT can be omitted from treatment routine for prophylaxis without compromising CNS relapse rates.33-35 Currently, RT is typically reserved for cases of overt CNS disease at diagnosis or relapse and in certain high-risk cases for prophylaxis; for example, patients with T-ALL on CALGB 10403 (C10403) received 24 Gy of prophylactic cranial RT.4
As noted, standard prophylaxis still yields CNS relapse rates of ∼10%. Other methods have been considered to further mitigate this risk, but results have been unconvincing. The use of intrathecal triple therapy (ITT), a combination of methotrexate, cytarabine, and a corticosteroid (often hydrocortisone), was not found to improve 5-year disease-free survival in children at high risk when compared with the use of the conventional single-agent IT methotrexate.36 Similarly, older data showed that ITT may actually yield an inferior OS.37 Therefore, single-agent IT methotrexate (sometimes alternating with cytarabine) remains the IT backbone for all adult protocols.
Case 2
A 65-year-old man with constitutional symptoms and cytopenias underwent a bone marrow examination, which demonstrated 85% B lymphoblasts. Fluorescence in situ hybridization was used to identify a BCR::ABL1 fusion (p190 isoform using reverse transcription polymerase chain reaction), confirming a diagnosis of Ph+ B-ALL. Performing an LP showed 4 RBCs per μL and 32 nucleated cells per μL, with blasts present using CC (CNS-3) and MFC. The patient did not have any neurologic signs or symptoms.
How do you manage a patient with newly diagnosed Ph+ B-ALL with CNS involvement?
For this patient, and other similar patients, our typical approach consists of administering IT therapy twice weekly until the CSF is clear, usually with alternating doses of 12 mg IT methotrexate and 100 mg IT cytarabine (unless the selected treatment regimen uses a different strategy). Other experts recommend once-a-week IT therapy during remission induction.38 If the blasts are cleared from the CSF (preferably negative with MFC), we then transition to the protocol-specific schedule of CNS-directed prophylaxis, using the CNS-3 schedule, if one exists. We also consider allogeneic hematopoietic cell transplant (HCT), if not already planned, based on other features of the patient's presentation.
There are several important considerations in this setting. The first is whether to include cranial or craniospinal RT in the upfront management. Some experts recommend the use of cranial RT during first remission for all patients with CNS-3 disease, regardless of the symptoms.38 We would typically consider a CNS-directed RT if the patient had presented with cranial nerve deficits, parenchymal involvement (which, again, is rare), and/or persistent disease in CSF despite intensified IT therapy, an approach derived from the original hyper-CVAD study.1 When RT is used, the specifics require careful consideration; knowledge of future HCT plans (in which total body irradiation [TBI]–based conditioning may be used) could affect the total radiation dose recommended.39 There is also the theoretical risk of increased toxicity if IT chemotherapy is administered shortly after RT, although this is not well described in the published literature. Such decisions should be made in close coordination with a radiation oncologist, with expertise on these issues.
With respect to the systemic therapy for this patient, the optimal regimen in this setting is uncertain. Although most approaches use CNS-penetrating chemotherapy (eg, methotrexate, cytarabine, and asparaginase), newer chemotherapy-free approaches for Ph+ ALL do not.40,41 It is unknown how well these chemotherapy-free strategies fare against CNS disease, because published results do not describe this population.40,41 As for the choice of tyrosine kinase inhibitor (TKI), we generally recommend dasatinib in this setting; imatinib does not cross the BBB,42 but dasatinib is effective in preclinical models and in patients with Ph+ ALL with CNS disease.43 In a recent trial comparing the effect of intensive chemotherapy plus imatinib vs dasatinib in children with Ph+ B-ALL, the 4-year cumulative CNS relapse risk was significantly lower in the dasatinib arm (2.7%) vs in the imatinib arm (8.4%).44 Similar CNS relapse rates were observed with chemotherapy-free trials involving dasatinib.40,41 Less is known about the CNS activity of the newer-generation ABL TKIs; therefore, their use in this setting is more controversial. Ponatinib crosses the BBB and may achieve higher CSF concentrations than dasatinib in preclinical models.45 However, CNS relapse rates were not reported from the 2 largest trials investigating ponatinib in ALL (either as monotherapy for relapsed/refractory disease, or frontline therapy combined with hyper-CVAD).46-48 Therefore, the CNS-specific efficacy of ponatinib compared with other TKIs is unknown.
For patients whose CSF does not clear, alternative approaches for CNS-directed therapy are considered. An Ommaya reservoir is a surgically placed intraventricular catheter intended to facilitate easier, repeat drug delivery into the CSF. There are potential pharmacokinetic benefits of delivering chemotherapy intraventricularly via this device.49 Data from pediatric patients support dose reductions of 50% when agents are delivered via an Ommaya reservoir,50 a practice we usually follow. An Ommaya reservoir can also be useful in cases in which repeat LP might prove challenging, such as in patients with obesity or with prior lumbar surgery. We typically only advocate for the placement of this device in patients for whom intensive IT and systemic therapy did not help in clearing out the CSF or those with anatomic limitations, as described previously.
Other IT agents may be considered, although data supporting their use are limited. Thiotepa and topotecan have been used for treating CNS disease.51,52 A liposomal formulation of cytarabine was produced with purported benefits of longer duration of action. Unfortunately, partially because of toxicity concerns, it is no longer manufactured.53,54 Several small series reported favorable results with IT rituximab for CNS relapse.55,56 Apart from the multiply refractory setting, it is rare to use any agents apart from methotrexate, cytarabine, and hydrocortisone; alternative drugs are usually used under the direction of an experienced hematologist and/or neuro-oncologist, and they may be prohibited in some jurisdictions. Lastly, it bears emphasis that vincristine is almost always fatal when given IT. Risk-mitigation measures endorsed by the Joint Commission and World Health Organization include providing vincristine in an IV “minibag” (and never in a syringe), prohibiting IV vincristine in areas where IT medications are administered and/or stored, and confirming whether any IT medications have been given before administering IV vincristine.57,58 One report described a patient who survived accidental IT vincristine, likely because of a prompt neurosurgical intervention using CSF irrigation combined with antineurotoxic therapy.59
The final, and perhaps the most important, consideration in this case is that of HCT. For all patients with Ph+ disease (regardless of CNS status), the historical standard has been to receive an HCT in first remission.60-62 Although this paradigm is shifting as we see improvements in the TKI-based therapy and risk stratification,63 we would still recommend an HCT in first remission for this patient if the CSF was void of detectable disease. An important consideration for this patient would be his age (65 years), which would likely preclude myeloablative conditioning (MAC). MAC is usually given as ≥12 Gy TBI in this disease; no prospective data exist to favor this approach over chemotherapy-based conditioning in adults, but eradication of disease in sanctuary sites via TBI is one of the main considerations driving this use.64 Reduced-intensity conditioning is commonly used in older patients; several retrospective studies have shown higher relapse rates with reduced-intensity conditioning compared with MAC, but similar OS rates in both.65-67 Other important transplant-specific considerations that pertain to CNS disease in ALL are discussed subsequently.
Case 3
A 23-year-old woman was found to have leukocytosis. Peripheral blood flow cytometry disclosed an abnormal, immature T-cell population consistent with that observed in T-ALL patients. Her first LP reports showed 8 RBCs per μL and 1 nucleated cell per μL and was negative using CC and MFC. She was treated with C10403 and received CNS-directed prophylaxis in accordance with the CNS-1 schedule. She achieved a measurable residual disease–negative remission with negative CSF levels after remission induction. She was referred to a radiation oncologist to discuss the role of prophylactic cranial RT, but this was deferred. Three months after completing prolonged maintenance, she developed headaches; an LP result was positive for CNS disease recurrence via both CC and MFC. A concurrent bone marrow exam showed no evidence of leukemia.
How do you treat a young adult with an isolated CNS relapse of T-ALL?
This patient has a late (ie, >18 months from diagnosis), isolated CNS relapse. The prognosis of an isolated CNS relapse is better than that of a combined CNS and marrow relapse, and similarly, a late relapse is more favorable than early relapse.68-70 That said, an isolated CNS relapse portends a systemic relapse and requires, at a minimum, intensive systemic therapy in addition to CNS-directed treatment. Our approach to any CNS relapse (either isolated or accompanied by a marrow relapse) involves 3 facets: (1) intensive CNS-directed therapy including IT and RT modalities, (2) multiagent systemic therapy with CNS-active agents, and (3) consideration of HCT if the CSF clears.
Regarding systemic therapy, the most informative studies in this setting come from the pediatric population (eg, POG 9412 and ALL R3).69,71 They use prolonged, intensified treatment schedules, including dexamethasone, asparaginase, and high-dose methotrexate and cytarabine as well as intra-CSF therapy. Because these treatment schedules were studied primarily among children, these approaches are likely only suitable for adolescents and young adults (AYAs), borrowing from the experience of treating AYAs in the frontline setting.72 For some of the reasons noted earlier, we consider the placement of an Ommaya reservoir in such cases to facilitate frequent intra-CSF therapy.
In cases such as this, we would consider POG 9412 or a similar regimen that uses intensified CNS-directed systemic chemotherapy. The dose and schedule of intra-CSF chemotherapy typically should follow those used in the published regimen, which (as in the case of POG 9412) may include ITT. Unlike prophylaxis, treatment of relapsed disease in the CNS justifies the toxicity observed with ITT in the frontline setting. Consideration also needs to be given to the radiation strategy; RT is a fundamental component of the management of CNS relapse but knowledge of anticipated HCT is important (often involving 12 Gy TBI conditioning). Again, the typical adult dose of RT is 24 Gy given in a fractionated dose schedule.39
Furthermore, the RT modalities used in this setting have evolved. “Cranial boost” in conjunction with TBI-based MAC has gained traction in ALL. The addition of low-dose (usually 6 Gy) cranial boost before TBI improves CNS relapse-free survival after HCT and has a trend toward improved progression-free survival and OS.73,74 This lower dose is felt to have reduced toxicity compared with historic doses of 12 Gy, while still retaining the therapeutic benefit. That said, cranial boost is typically not offered to those who have received prior cranial or craniospinal RT (given concerns of cumulative neurotoxicity), underscoring the importance of early treatment planning for patients in whom HCT is being considered. Proton-beam therapy to the CNS is another approach, which may reduce toxicity because of its physical properties while potentially allowing more liberal dosing to the craniospinal axis.39
In this patient, HCT should be considered, given her young age, relapsed disease, and T-cell phenotype. The approach to HCT in this setting remains challenging because no consensus exists regarding optimal management of adults with CNS relapse. Data from the pediatric population support the notion that HCT can be deferred without compromising the outcomes in those with isolated CNS relapses and favorable prognostic features (eg, longer first remission),69 whereas those with early relapses and high-risk features (eg, older age) may benefit from HCT.75 Historically, adult patients with a history of CNS disease have higher rates of post-HCT CNS relapse and inferior survival.76,77 Because of this, some have advocated for the routine use of post-HCT CNS-directed prophylaxis; however, this was not endorsed by the American Society for Transplantation and Cellular Therapy.78
Case 4
A 32-year-old man with Ph− B-ALL was treated using hyper-CVAD as well as CNS-directed prophylaxis. He achieved a measurable residual disease–negative complete remission, but he tolerated therapy poorly and was lost to follow-up. Several months later, he returned with relapsed disease involving his bone marrow and CNS. He achieved a second remission with POG 9412, but subsequent treatment plans (including RT and HCT) were delayed because of infectious complications. Unfortunately, after this delay, his bone marrow showed 48% B lymphoblasts with a normal expression of CD19 and CD22. An LP report also showed CNS recurrence with a similar immunophenotype.
What strategies would you use in this patient with Ph− B-ALL with multiply relapsed disease involving the bone marrow and CNS?
In recent years, we have seen the introduction of several novel therapies, including CD19-directed chimeric antigen receptor (CAR)–modified T-cell therapy (tisagenlecleucel and brexucabtagene autoleucel), the CD3-CD19 bispecific T-cell engager blinatumomab, and the CD22-directed antibody-drug conjugate inotuzumab ozogamicin (InO).79-83 Details about these agents and their potential role in the management of CNS disease in ALL are included in Table 3. Because of concerns regarding the unknown efficacy and treatment-related neurotoxicity, patients with a history of CNS disease were excluded outright or were required to have an adequate understanding of their CNS disease to enroll in the pivotal studies. As with our patient in case 4, treatment outcomes for CNS disease refractory to conventional therapies are historically dismal, so the importance of establishing the role of these novel therapies in this setting cannot be overstated.
Evidence of CNS activity of antibody-based therapeutics for relapsed/refractory B-ALL
| Agent . | Mechanism of action . | Evidence of CNS activity∗ . |
|---|---|---|
| Blinatumomab | CD3-CD19 bispecific T-cell engager | Limited: 1 retrospective series84 |
| Inotuzumab ozogamicin | CD22 antibody-drug conjugate | None |
| Tisagenlecleucel | CD19 CAR T cells | Moderate: pooled post hoc analysis of prospective studies and multiple retrospective series85-87 |
| Brexucabtagene autoleucel | CD19 CAR T cells | Limited: extrapolated from experience with other CAR T-cell therapies |
| Agent . | Mechanism of action . | Evidence of CNS activity∗ . |
|---|---|---|
| Blinatumomab | CD3-CD19 bispecific T-cell engager | Limited: 1 retrospective series84 |
| Inotuzumab ozogamicin | CD22 antibody-drug conjugate | None |
| Tisagenlecleucel | CD19 CAR T cells | Moderate: pooled post hoc analysis of prospective studies and multiple retrospective series85-87 |
| Brexucabtagene autoleucel | CD19 CAR T cells | Limited: extrapolated from experience with other CAR T-cell therapies |
Please see text and references cited for additional details.
CAR T-cell therapy may be safe and effective in the management of CNS relapse. Recently, the outcomes of 154 children and AYAs with relapsed/refractory B-ALL and a history of CNS involvement were examined in a post hoc analysis of 5 CD19 CAR T-cell therapy trials. The authors found no difference in relapse-free survival, OS, or toxicity rates (cytokine release syndrome and immune effector cell–associated neurotoxicity syndrome) between those with CNS disease and those without. This suggests that CAR T-cell therapy is effective and safe in the setting of CNS disease (either with or without concurrent medullary relapse).85 Another retrospective analysis described the outcomes of children and AYAs treated with CD19 CAR T-cell therapy for active CNS disease; unlike the aforementioned study, all patients had active CNS disease at enrollment, although after bridging therapy, 30% of patients had active CNS disease at lymphodepletion. Although they reported a 94% complete response rate, CAR T-cell therapy did not appear to effectively mitigate systemic or CNS relapse, which occurred in 40% and 22% of children and AYAs, respectively.86 Another smaller retrospective study yielded similar findings.87 Importantly, results from the first prospective trial specifically designed to address the efficacy and safety of CD19-directed CAR T-cell therapy in the treatment of active CNS disease were reported recently.88 CAR T-cell therapy resulted in 85.4% clearance of CNS disease, and survival and toxicity results were comparable with those of previous experiences.
Regarding the 2 other novel therapies (ie, blinatumomab and InO), data regarding their safety and efficacy in the treatment of CNS disease are limited, primarily because of minimal, if not absent, representation of patients with active CNS disease in most clinical trials. There is no available evidence to suggest that blinatumomab crosses the BBB, although, based upon its molecular size (55 kilodaltons), it is speculated that it could.14 One retrospective report described an experience with blinatumomab in 11 patients with CNS-positive relapsed/refractory B-ALL.84 Blinatumomab was generally well tolerated, although severe neurotoxicity occurred in 2 patients. Interestingly, rates of CNS relapse after blinatumomab were relatively high in a separate study.89 InO does not cross the BBB, and, as such, would be unlikely to have single-agent CNS-directed activity. Rates of CNS relapse after single-agent InO have not (to our knowledge) been reported.79,90
Conclusion
Prevention and management of CNS disease are integral components of adult ALL care. Our understanding of and approach to this entity have evolved with respect to the strategies we use to treat and prevent CNS disease and mitigate treatment-related toxicities. Although IT and systemic therapy remain the foundation of our treatment approach, the introduction of CAR T-cell therapy represents a promising treatment strategy for those with CNS relapses. However, more definitive trials are needed, and this therapy is not available globally. New approaches are needed for patients with T-cell phenotype and others with high-risk disease features.
Acknowledgments
The authors thank Aaron C. Logan (University of California, San Francisco, San Francisco, CA) for his feedback on an initial draft of the manuscript.
This work was supported by grants from the National Institutes of Health, National Heart, Lung, and Blood Institute (grant T32HL007093-47) (N.E.K.).
Authorship
Contribution: All authors conceptualized and wrote the manuscript and produced the figures and tables.
Conflict-of-interest disclosure: R.D.C. has received research funding from Amgen, Kite/Gilead, Merck, Pfizer, Servier, and Vanda Pharmaceuticals; has reported consultancy/honoraria from Amgen, Jazz, Kite/Gilead, and Pfizer; has reported membership on the boards or advisory committees for Autolus and PeproMene Bio; and spouse-owned stock in Seagen. N.E.K. declares no competing financial interests.
Correspondence: Ryan D. Cassaday, Division of Hematology, Department of Medicine, University of Washington School of Medicine, University of Washington, 825 Eastlake Ave E, Mailstop LG-700, Seattle, WA 98109-1023; e-mail: cassaday@uw.edu.

![Modalities for CNS prophylaxis and treatment of active CNS disease. (A) In most patients, there is no evidence of CNS disease at diagnosis. Here, prevention of CNS relapse depends primarily on IT therapy (most commonly with MTX) and CNS-penetrating systemic therapy (traditional cytotoxic chemotherapy [CHEMO] as well as the ABL TKI dasatinib, the latter for use in Ph+ disease). (B) In cases of overt CNS disease at diagnosis or of a CNS relapse, many of the same tools used in the prophylaxis setting, such as IT and systemic chemotherapy, are used. Additional tools include RT, CD19 CAR-modified T-cells, and consolidative HCT. Figure created with BioRender.com.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/141/12/10.1182_blood.2022017035/8/m_blood_bld-2022-017035-c-gr1.jpeg?Expires=1765882983&Signature=cLg4BUW9MIomO1T40N5xwOLuOj4tnoYXgHbtnGup5w0XMY8SKhKK4V5Gg-tXg1Z7D4TIkgF1NaA1NPPyFl~r8okgjZiWba6mSzmOtQbNzB6ON3tJw80yqx9-h43w5-blFx6ShSiGk3mvGoCNlw6AWuSe4lsE0cgMUaQwBBcpNwUror~DRwVHEuE23L-~BhufqtcGqtoFFyoMJPsJaNdJqeH8vTeFGuS9~MwXJRVhNxtdPQn2xX1XOPjaW9vABAHQjV1ooWj33YTYZ6qT2LT-78sMUENSCC8dcPW~4aqQl61TAUqGxq1vRtfX~Pxn~NibgmM7fNszUtm6tgtJGVMZIQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
This feature is available to Subscribers Only
Sign In or Create an Account Close Modal