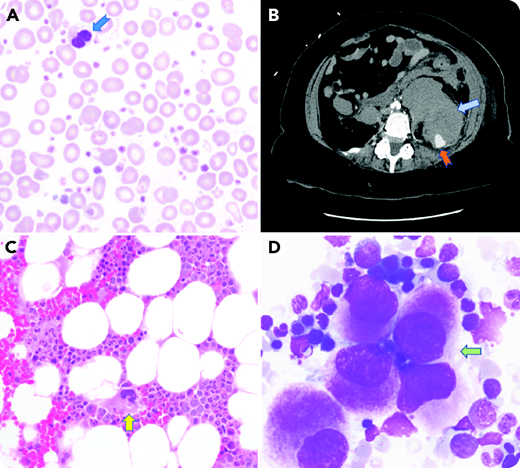
A 65-year-old woman underwent a bone marrow aspiration and biopsy of the left iliac crest for evaluation of macrocytic anemia and elevated platelet count of 1 257 000/μL (panel A: Wright-Giemsa stain; ×1000 magnification; anisopoikilocytosis; dysplastic bilobated neutrophil). After the procedure, she reported weakness in her left leg and severe pain around the site without external bleeding. A few hours later, she was found to have a blood pressure of 95/46 mmHg and a heart rate of 101 beats per minute. Repeat laboratory studies showed a decrease in hemoglobin from 7.8 g/dL before the procedure to 5.5 g/dL after the procedure along with acute renal failure. A computed tomography scan of the abdomen and pelvis showed a large retroperitoneal hemorrhage (RPH) with active intravascular contrast extravasation (panel B). She was resuscitated with red blood cell transfusions and embolization of the L4 lumbar artery. Biopsy results showed evidence of myelodysplastic/myeloproliferative neoplasm, unclassifiable, with hypercellular bone marrow and dysplastic megakaryocytes (panel C; hematoxylin and eosin stain; ×400 magnification; panel D; Wright-Giemsa stain ×1000 magnification). Molecular testing did not show JAK2, CALR, or MPL gene mutations. Acquired von Willebrand disease was ruled out.
RPH is a rare complication following a bone marrow biopsy, and sudden onset of back pain, hypotension, and lower extremity neurologic symptoms indicate that further evaluation is needed. Obesity, myeloproliferative neoplasms, antiplatelet agents, and thrombocytopenia are some of the additional risk factors outside direct procedure-related trauma. This patient was taking aspirin and likely bled from direct vascular injury that resulted from the anatomical proximity of the lumbar artery to the iliac crest.
A 65-year-old woman underwent a bone marrow aspiration and biopsy of the left iliac crest for evaluation of macrocytic anemia and elevated platelet count of 1 257 000/μL (panel A: Wright-Giemsa stain; ×1000 magnification; anisopoikilocytosis; dysplastic bilobated neutrophil). After the procedure, she reported weakness in her left leg and severe pain around the site without external bleeding. A few hours later, she was found to have a blood pressure of 95/46 mmHg and a heart rate of 101 beats per minute. Repeat laboratory studies showed a decrease in hemoglobin from 7.8 g/dL before the procedure to 5.5 g/dL after the procedure along with acute renal failure. A computed tomography scan of the abdomen and pelvis showed a large retroperitoneal hemorrhage (RPH) with active intravascular contrast extravasation (panel B). She was resuscitated with red blood cell transfusions and embolization of the L4 lumbar artery. Biopsy results showed evidence of myelodysplastic/myeloproliferative neoplasm, unclassifiable, with hypercellular bone marrow and dysplastic megakaryocytes (panel C; hematoxylin and eosin stain; ×400 magnification; panel D; Wright-Giemsa stain ×1000 magnification). Molecular testing did not show JAK2, CALR, or MPL gene mutations. Acquired von Willebrand disease was ruled out.
RPH is a rare complication following a bone marrow biopsy, and sudden onset of back pain, hypotension, and lower extremity neurologic symptoms indicate that further evaluation is needed. Obesity, myeloproliferative neoplasms, antiplatelet agents, and thrombocytopenia are some of the additional risk factors outside direct procedure-related trauma. This patient was taking aspirin and likely bled from direct vascular injury that resulted from the anatomical proximity of the lumbar artery to the iliac crest.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal