Treatment of polycythemia vera (PV) with the Murine Double Minute 2 (MDM2) antagonist, idasanutlin, in a phase 1 trial was reported by our group to be well tolerated with a high overall response rate (Mascarenhas et al, Blood. 2019 Jun 5). A global, phase 2 trial is currently underway evaluating idasanutlin in hydroxyurea (HU) resistant/intolerant PV patients (NCT03287245). MDM2, a negative regulator of TP53 is upregulated in PV CD34+ cells and inhibition of MDM2 targets PV hematopoietic stem/progenitor cells (HSPC) (Lu et al, Blood. 2014;124(5):771-90). Additional trials of MDM2 antagonists have shown promise, however, there is concern that these agents have the potential to induce TP53 mutations or promote expansion of TP53 mutated clones. Resistance to MDM2 inhibitors has been evaluated in solid tumor cell lines and attributed to either the emergence of de novoTP53 mutations or the selection of TP53 mutated clones. (Michaelis et al, Cell Death Dis. 2011;2:e243; Skalniak et al, Cancers. 2018;10(11)).
The effect of MDM2 inhibition on TP53 mutant clones is of particular interest in myeloproliferative neoplasms (MPNs). TP53 mutations have been reported with a low allele burden in ~15% of chronic MPN patients (Kubesova et al, Leukemia. 2018;32(2):450-61), however, TP53 loss of heterozygosity and rapid expansion of TP53 mutant clones is associated with transformation to blast phase (Lundberg et al, Blood 2014,123:2220-8).
As reported, in the idasanutlin PV trial, 1/13 patients were identified to have a baseline pathogenic TP53 mutation in hematopoietic cells (VAF 5.5%), using a deep sequencing assay with a limit of detection (LOD) of VAF 0.5%. This patient was a non-responder to idasanutlin and upon treatment had an increasing JAK2V617F and TP53 mutant VAF.
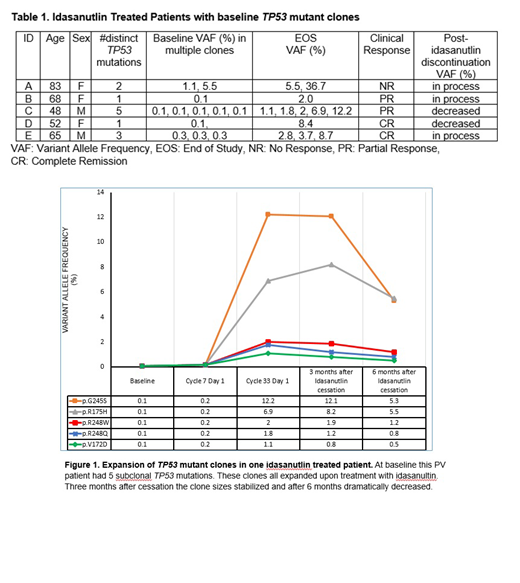
End of study hematopoietic cell specimens of all patients were deep sequenced (LOD 0.1%) and revealed that 4 additional patients harbored detectable TP53 mutations after idasanutlin treatment with VAF ranging from 1-12%. In each sample, 1-5 unique TP53 mutations were identified, all within the hotspot domain of the TP53 gene. Deeper sequencing of baseline and follow-up samples revealed these mutations were present at a subclonal level (VAF 0.1-5.5%) and increased over time, indicating that treatment with the MDM2 antagonist promoted expansion of already existing TP53 mutant clones (Table 1, Figure 1). None of the patients who lacked a TP53 mutation at baseline developed a TP53 mutant clone with idasanutlin treatment. There was no clear association of presence of TP53 mutations with prior HU, anagrelide or interferon exposure.
There has been careful monitoring of patients to determine whether the expanding TP53 clone has clinical ramifications. Patients were on study for a median of 54 weeks (23-131). The only patient who exemplified resistance to idasanutlin was the single patient with a high burden TP53 mutation (37%). All other patients were taken off study due to patient choice/toxicity. Furthermore, all TP53 mutant and non-mutant patients have had stable disease with no evidence of progression to MF or AML. Sequencing of 2 patients post-discontinuation of idasanutlin revealed that the VAF of the TP53 mutant clones decreased since the agent was discontinued. Updated patient molecular data post-treatment discontinuation will be reported at the meeting.
To investigate whether idasanutlin induces de novo TP53 mutations in PV myeloid cells we performed long term HSPC cultures. Mononuclear cells from 6 distinct PV patients were treated continuously with idasanutlin (500 nM) over ~6 weeks and DNA from both treated and untreated colonies were analyzed using next generation sequencing with a LOD of 2% VAF and no TP53 mutations were detected.
The combined in vitro and clinical data reveals that treatment with an MDM2 antagonist is not associated with the emergence of de novoTP53 mutations but rather the expansion of prior existing TP53 clones. This does not appear to have clinical repercussions, however, close monitoring of these patients is essential. We recommend that patients be screened for TP53 mutations prior to treatment with an MDM2 antagonist and that if present the TP53 mutant VAF be followed during their treatment course. Resistance to MDM2 inhibition is likely dependent on the TP53 mutant VAF and further studies will need to clarify the ideal dosing schedule of MDM2 antagonists and/or combinatorial therapy to prohibit TP53 mutant clonal expansion.
Houldsworth:Cancer Genertics: Other: stock in; Sema4: Employment. Rossi:Sema4: Employment. Kiladjian:AOP Orphan: Honoraria, Research Funding; Celgene: Consultancy; Novartis: Honoraria, Research Funding. Rampal:Agios, Apexx, Blueprint Medicines, Celgene, Constellation, and Jazz: Consultancy; Constellation, Incyte, and Stemline Therapeutics: Research Funding. Mascarenhas:Incyte: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Research Funding; Roche: Consultancy, Research Funding; Merck: Research Funding; Celgene: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; CTI Biopharma: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Janssen: Research Funding; Promedior: Research Funding; Merus: Research Funding; Pharmaessentia: Consultancy, Membership on an entity's Board of Directors or advisory committees. Hoffman:Merus: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal