
Background: The Japan Adult Leukemia Study Group (JALSG) conducted the Ph+ALL202 and Ph+ALL208 studies for newly diagnosed (ND) Philadelphia-chromosome (Ph)-positive acute lymphoblastic leukemia (ALL), and successfully introduced imatinib into intensive chemotherapy followed by allogeneic hematopoietic cell transplantation (alloHCT). However, 30-40% of patients could not undergo alloHCT at CR1 because of older age, early relapse, or therapy-related death. We report the outcome of the Ph+ALL213 study, which introduced dasatinib (DA) to improve the efficacy and two-step combination to minimize the toxicity of treatments prior to alloHCT.
Methods: The Ph+ALL213 study was a single-arm, multicenter phase II study for ND Ph+ALL. The protocol was reviewed and approved by the institutional review board of each hospital and registered in the UMIN Clinical Trials Registry (#UMIN000012173) and the Japan Registry of Clinical Trials (#jRCTs041180136). Patients with ND BCR/ABL1-positive ALL aged 16-64 years with PS 0-3 and sufficient organ function were included. All patients provided written informed consent before enrollment. The first step of treatment was induction (IND) targeting hematological complete remission (HCR) by 28 days of 140-mg DA and 14 days of 60-mg/m2 prednisone (PSL). IND was preceded by 7 days of PSL pre-phase treatment, during which BCR/ABL1 was confirmed by multiplex RQ-PCR. The second step was intensive consolidation (IC) targeting molecular CR (MCR), which was defined as no BCR/ABL1 signal by RQ-PCR, by 28 days of 100-mg DA in combination with CALGB BFM-like intensive chemotherapy. Consolidation comprised 4 cycles alternating between two regimens: high-dose methotrexate/cytarabine followed by 21 days of 100-mg DA (C1) and a CHOP-like regimen using vincristine (VCR)/cyclophosphamide/daunorubicin followed by 21 days of 100-mg DA (C2). The maintenance regimen was 12 cycles of 24 days of 100-mg DA with VCR /PSL. Patients who achieved HCR and had an appropriate donor proceeded to alloHCT after the first C1 consolidation (C1-1). DA was started after alloHCT only when the BCR/ABL1 signal was positive by RQ-PCR just before transplantation. The primary endpoint was event-free survival (EFS) from the induction at 3 years. Major secondary endpoints were hematological and molecular responses, adverse events (AEs), hematological relapse, non-relapse mortality (NRM), and overall survival (OS) from the induction at 3 years.
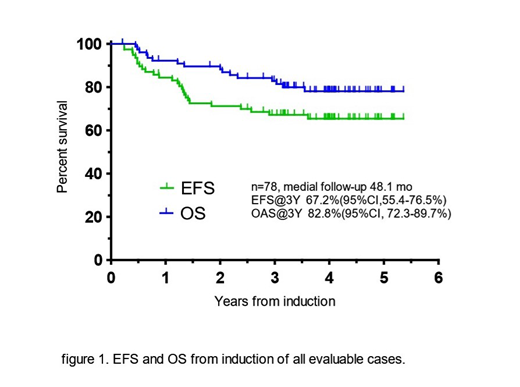
Results: Of the 81 patients enrolled between Feb 2014 and April 2016 from 46 hospitals, 78 were evaluable, and the median age was 45 years (range, 16-64 years). Hematological response after IND were 73 (93.6%) CR, 4 (5.1%) CRi, and 1 (1.3%) PD, and 40 (56%) patients achieved MCR after IC. Grade 4 neutropenia/ thrombocytopenia in IND, IC, and C1-1 was reported in 51.3%/ 48.7%, 93.5%/ 5.2%, and 97.2%/ 70.8%, respectively, whereas grade 4 non-hematological AEs were noted in 2.6%, 9.1%, and 8.5%, respectively. No patients died during the course of IND, IC, or C1-1. All of 4 patients who relapsed before alloHCT had T315I mutations. One pt relapsed only in the CNS. Six patients completed the planned chemotherapy, and 8 patients discontinued the planned treatment because of AEs (4), physician's decision (2), and transfer (2) to non-registered hospitals. AlloHCT at CR1 was performed for 58 patients (74.4%). Forty-one patients (70.7%) had CMR just before transplantation. MAC and RIC conditioning was intensified for 69.0% and 31.0%, respectively, and the donor type was related, unrelated, and cord blood for 29.3%, 48.3%, and 20.7%, respectively. Eleven of 13 patients who discontinued the treatment underwent alloHCT afterwards. Three patients had NRM, but 7 patients survived with CR. At the median follow-up of 48.1 months, the 3-year EFS and OS were 67.2% (95%CI, 55.4-76.5%) and 82.8% (95%CI, 72.3-89.7%), respectively (figure 1). Of the patients who transplanted at CR1, the 3-year EFS and OS were 74.1% (95%CI, 60.8-83.5%) and 86.1% (95%CI, 74.2-92.8%), respectively. Among these patients, hematological relapse, relapse mortality, and NRM were noted in 10 (17.2%), 5 (8.6%), and 6 (10.3%), respectively.
Conclusions: In this study, we reduced the relapse and toxicity before alloHCT, and improved the EFS and OS at 3 years. JALSG is starting a Ph+ALL219 phase II study to introduce ponatinib for patients who did not achieve CMR after INC following the schedule in the Ph+ALL213 study.
Kako:Pfizer Japan Inc.: Honoraria; Bristol-Myers Squibb: Honoraria. Yokoyama:Astellas: Other: Travel expenses. Onishi:Pfizer Japan Inc.: Honoraria; MSD: Honoraria, Research Funding; Novartis Pharma: Honoraria; Bristol-Myers Squibb: Honoraria, Research Funding; Janssen Pharmaceutical K.K.: Honoraria; Astellas Pharma Inc.: Honoraria; Celgene: Honoraria; ONO PHARMACEUTICAL CO., LTD.: Honoraria; Otsuka Pharmaceutical Co., Ltd.: Honoraria; Nippon Shinyaku: Honoraria; Takeda Pharmaceutical Co., Ltd.: Research Funding; Chugai Pharmaceutical Co., Ltd.: Honoraria; Sumitomo Dainippon Pharma: Honoraria; Kyowa-Hakko Kirin: Honoraria. Shiro:Bristol-Myers Squibb: Honoraria. Atsuta:CHUGAI PHARMACEUTICAL CO., LTD.: Honoraria; Kyowa Kirin Co., Ltd: Honoraria. Miyazaki:Chugai: Research Funding; Otsuka: Honoraria; Novartis: Honoraria; Nippon-Shinyaku: Honoraria; Dainippon-Sumitomo: Honoraria; Kyowa-Kirin: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal