Introduction: Therapy-related myeloid neoplasms (t-MNs) are among late complications of chemotherapy and/or radiotherapy. So far, the genetic landscape of t-MNs is not yet defined as there has been few reports for their comprehensive genomic analysis. Recently, in the field of hematological malignancies, accumulating evidence supported that tumor derived fragmentary DNA in serum, known as circulating tumor DNA (ctDNA), has the potential to serve as an alternative for conventional bone marrow (BM) analysis (Nakamura and Yokoyama et al, Blood 2019). However, no studies are available to support the utility of ctDNA to evaluate the clonal kinetics in t-MNs. In the present study, by using retrospective tracking of driver mutations in BM or available serum samples, we tried to elucidate when the founder clones had appeared and how they had evolved pre-, during, and post-cytotoxic chemotherapy for prior hematological malignancies.
Methods: We retrospectively collected tumor samples, including BM, tumor-rich peripheral blood (PB), or alternatively, serum samples, at diagnosis and before diagnosis from 15 t-MNs patients in our hospital. We subjected tumor DNA and control buccal swab DNA to comparative whole-exome sequencing (WES, n=13) and/or whole-genome sequencing (WGS, n=2). After identifying somatic driver mutations, we designed droplet digital PCR (ddPCR) assays for each mutation identified.
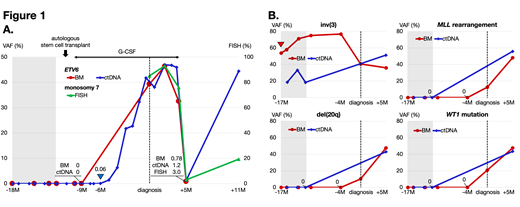
Results: All 15 patients had a history of primary hematological malignancies (malignant lymphoma, n=9; acute leukemia, n=4; multiple myeloma, n=2) and had received prior chemotherapy and/or radiotherapy with or without autologous stem cell transplantation (ASCT). The median age at presentation of t-MNs was 53 years (range, 6-74), and the median latent period between prior malignancy and t-MNs was 45 months (range, 10-161). Conventional cytogenetic analysis revealed high incidence of complex karyotype (38.4%) and MLL rearrangement (30.7%). WES and/or WGS revealed that 93.3% (n=14/15) of the cases contained at least one putative driver mutation in 17 genes (median of 1 mutation per patient [range 1-4]). We found the most frequent mutations in TP53 and epigenetic modifier gene (KMT2D/KDM6A/ASXL1/ASXL2), mutated in 33% of the samples, followed by signal transduction proteins (MPL/BRAF/FLT3-TKD/KRAS, 26.7%). Together, the spectrums of driver mutations and cytogenetic alterations in our cohort were consistent with previous reports in t-MNs. Most importantly, we could trace back mutant clone using BM and/or serum before diagnosis of t-MNs in 7 patients. Particularly, in UPN-5 who developed MDS-EB1 after ASCT for lymphoma, ETV6 p.E153fs, a putative founder mutation of t-MNs, was applied to liquid biopsy to trace back. ETV6 ctDNA could be detected as early as 7 months prior to the development of MDS with variant allele frequency (VAF) of 0.06% (blue arrowhead in figure 1A). Most intriguingly, the proportion of ETV6 ctDNA varied with or without G-CSF administration during the clinical course; VAF increase from 0 to 47.0% on G-CSF and decrease from 47.0 to 1.2% off G-CSF. In UPN-10 who had been clinically diagnosed as t-MNs (MDS-EB2) after intensive chemotherapy for prior AML, not otherwise specified with normal karyotype, WGS identified 4 driver mutations in BM at diagnosis of t-MNs. Then, 4 driver mutations, WT1 p.A365fs, MLL rearrangement, inv(3), and del(20q) were all applied to combined analysis of ctDNA and BM as well. Unexpectedly, we could find the presence of the founder clone, inv(3), with high allele burden in BM at initial diagnosis of AML-NOS with normal karyotype (red arrowhead in figure 1B). On the contrary, we could not detect other 3 gene alterations until 4 months before diagnosis of t-MNs.
Conclusions: These findings would contribute to outline the genetic landscape of t-MNs, and especially suggest the role of cytokine-related selective pressures after chemotherapy and of the potential pre-t-MNs conditions in the pathogenesis of t-MNs.
Figure 1: Serial mutation and cytogenetic status of BM and/or ctDNA in two patients with t-MNs (UPN-5 and -10, in figure 1A and in 1B, respectively). Shaded areas indicate the period of cytotoxic chemotherapies. Abbreviations: M, months; VAF, variant allele frequency.
Nagamura-Inoue:AMED: Research Funding. Uchimaru:Daiichi Sankyo Co., Ltd..: Research Funding. Tojo:Torii Pharmaceutical: Research Funding; AMED: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal