
BACKGROUND: Despite advancements in medical therapy and supportive care for sickle cell disease (SCD) over the last several decades, disease morbidity and mortality remain unacceptably high. Allogeneic hematopoietic stem cell transplant (HSCT) is a curative therapy for SCD, but is associated with significant risks: conditioning regimen toxicity, graft failure, graft-versus-host disease (GVHD), and death are all potential sequelae, particularly when hematopoietic stem cells (HSC) originate from sources other than HLA-matched related donors (MRD). Gene therapy (GT), which involves ex vivo gene addition or editing of autologous HSCs, has recently emerged as an alternative curative approach for SCD. While GT still carries the risk of conditioning regimen-associated toxicity, the use of autologous over allogeneic HSCT eliminates the risk of GVHD as well as the need for an available HLA-matched donor. Both allogeneic HSCT and GT have demonstrated efficacy against SCD in clinical trials, yet these curative strategies have never been compared. Here, we present preliminary data from a systematic review comparing allogeneic HSCT and GT outcomes in SCD.
METHODS: We searched the MEDLINE and EMBASE databases (including American Society of Hematology and European Hematology Association meeting abstracts) for studies evaluating outcomes following allogeneic HSCT and GT in SCD. The references of included studies were screened for additional relevant studies. We included phase I, II, and III clinical trials, retrospective reviews, case reports, and case series involving SCD patients of all ages undergoing allogeneic HSCT or GT. All HSC donor sources (MRD, matched unrelated donors (MUD), haploidentical, autologous) and conditioning regimens were included. Case reports with <2 SCD patients, non-English studies, and pre-clinical studies were excluded. Studies including both SCD and thalassemia patients were included if SCD outcomes were reported separately. We assessed the primary outcomes of overall survival (OS) and event-free survival (EFS)-defined as stable donor erythropoiesis or transgene expression, absence of new or worsening SCD complications, graft rejection, GVHD, or graft failure-at 2 and 5 years post-transplant. All titles and abstracts were screened for full text retrieval. Data on study characteristics, quality, and effects were extracted and analyzed using descriptive statistics. Risk of bias was assessed using the Newcastle-Ottawa Scale. Heterogeneity of outcomes was assessed using sensitivity and subgroup analyses, and publication bias was assessed using funnel plot, where applicable.
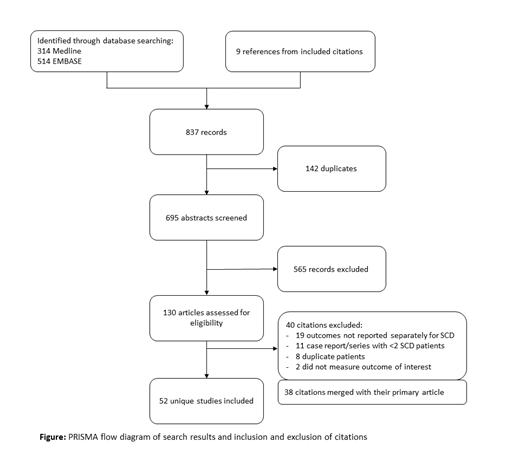
RESULTS: We identified 828 titles through database searching and 9 titles from references of included studies (Figure). Following removal of duplicate citations (n=142), exclusion of records not meeting eligibility criteria (n=605), and merging 38 studies with their primary article, 52 unique studies were included for data extraction. Of these 52 studies, 49 reported outcomes for allogeneic HSCT and 3 reported outcomes for GT, representing 1026 and 19 unique patients, respectively. Donor HSC source was MRD (n=24), MUD (n=5), haploidentical (n=5), or a combination thereof (n=10) in 44/49 allogeneic HSCT studies which reported these data. Length of follow-up was 3249.5 patient-years in the allogeneic HSCT group versus 24 patient-years in the GT group. Transplant-related mortality was 60/1026 (5.8%) and 0/19 in the allogeneic HSCT and GT groups, respectively. Graft failure was 83/1026 (8.1%) for allogeneic HSCT patients. In the GT group, 1/19 (5.3%) failed to achieve clinically significant anti-sickling globin levels. OS for allogeneic HSCT patients at 2 years was 91% among 158 patients from 8 studies, and 93% at 5 years among 162 patients from 4 studies. EFS for allogeneic HSCT patients at 2 years was 86% among 126 patients from 6 studies, and 89% at 5 years among 192 patients from 5 studies. OS and EFS were not reported for GT studies. Rates of GVHD could not be calculated due to heterogeneity of reporting.
CONCLUSIONS: Although data for both allogeneic HSCT and GT in SCD are encouraging, longer follow-up is needed for GT patients in order to better assess regimen efficacy. Furthermore, outcomes reporting is highly heterogeneous both within and between treatment groups, underscoring the need for standardized reporting. Additional outcomes will be reported during the meeting.
Kuo:Agios: Consultancy; Alexion: Consultancy, Honoraria; Apellis: Consultancy; Bioverativ: Other: Data Safety Monitoring Board; Bluebird Bio: Consultancy; Celgene: Consultancy; Novartis: Consultancy, Honoraria; Pfizer: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal