Background: The FDA approved hydroxyurea (HU) for the treatment of sickle cell disease (SCD) in children because it was deemed a safe and efficacious treatment. HU modifies the course of the disease, reduces complications, improves survival, and has few long-term side effects. Despite these benefits, HU uptake remains low for young children. Over 75% of patients who could benefit from HU do not receive the treatment. NHLBI clinical practice guidelines recommend use of shared decision making for HU initiation but currently, there is no "gold standard" for hematology providers to follow when beginning their discussion about HU. Thus, there is likely a gap between care guidelines and clinical practice. A first step in closing this gap is to better understand the current practice utilized by hematology providers when discussing HU as a therapeutic option.
Objectives: The goal of the present study is to describe current practice used by hematology providers when discussing HU with parents of young children with SCD (0 - 5 years of age), Our primary aims are: 1) Map the process of offering HU to identify common themes, overlaps, and variations, 2) Examine the impact of a brief video presentation about the NHLBI HU guidelines on provider knowledge and comfort levels.
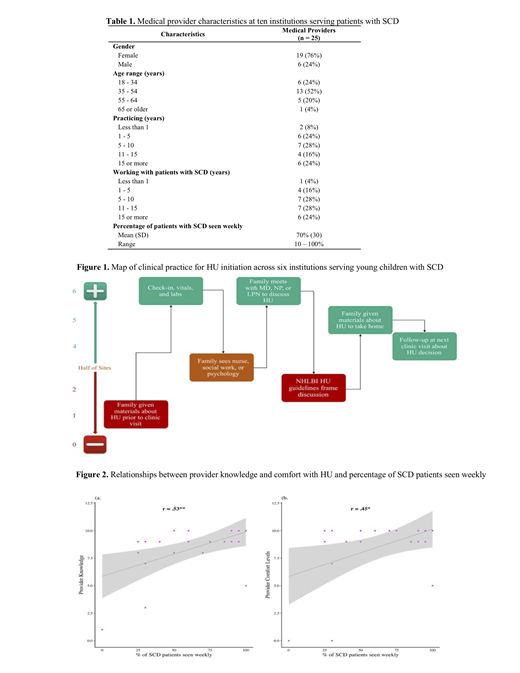
Methods: The dissemination of methods to increase adherence to NHLBI HU guidelines are being evaluated as part of a clinical trial (NCT03442114). Hematology providers at 6 children's hospitals serving young patients with SCD completed process maps that described their current practice for discussing HU initiation with parents. Twenty five hematology providers at 10 institutions across the United States viewed a video didactic presentation on the NHLBI HU guidelines for SCD. Knowledge and comfort regarding discussing HU was assessed using a 10-point scale before and after the video. We also collected data on provider demographics, years practicing, and percentage of patients seen with SCD each week in their practice.
Results: Preliminary analyses identified common themes (see Table 1 for provider characteristics). All 6 sites reported that labs and vitals were taken prior to the visit so they could be reviewed with the family. A medical doctor, nurse practitioner, or licensed practical nurse (LPN) led the HU initiation discussion. The majority of sites give their families HU-related materials to take home after the discussion and followed-up regarding the family's decision at the next clinic visit (i.e. planned for a two-visit HU initiation process). Variations identified included providing HU-related materials to the family prior to the visit, when the discussion would occur, and whether NHLBI HU guidelines framed the discussion (Figure 1).
Paired samples t-tests assessed for change in medical provider reported HU knowledge and comfort before and after the SCD didactic presentation. Data revealed that there were no differences in provider comfort,t(21) = .77, p = .45, d = .03. In contrast, there was a trend towards a significant increase in medical provider knowledge from before (M = 8.4, SD = 2.3) to after (M = 8.7, SD = 2.1) the presentation, t(21) = 1.8, p = .08, d = .11, small effect. Correlation analyses determined that higher baseline provider knowledge and comfort with HU were significantly correlated with seeing more SCD patients on a weekly basis (Figure 2).
Discussion: This study identified common elements of clinical practice for HU initiation in young children with SCD, but variations were also revealed. All institutions in the study obtained lab work prior to the discussion with the family; however the provider initiating the discussion varied by site (e.g., 1 site used an LPN). Most institutions plan for a two-visit discussion as families may not be ready to make a decision during the first visit but feel more supported over time. It is critical that patients and families make their decision based on SCD-specific HU information. Study data indicated that a brief didactic presentation elicited a small improvement provider HU knowledge. Moreover, exposure to the SCD population was strongly related to knowledge and comfort with HU, suggesting that hematology providers with more experience working with patients with SCD may be in the best position to initiate discussions about HU. The incorporation of decision support tools might help to support hematology providers and reduce the variation across institutions observed in our study.
King:Tioma Therapeutics (formerly Vasculox, Inc.):: Consultancy; RiverVest: Consultancy; Novimmune: Research Funding; WUGEN: Equity Ownership; Celgene: Consultancy; Cell Works: Consultancy; Magenta Therapeutics: Membership on an entity's Board of Directors or advisory committees; Amphivena Therapeutics: Research Funding; Bioline: Consultancy; Incyte: Consultancy. Piccone:Hemex Health, Inc.: Patents & Royalties. Neumayr:Terumo: Research Funding; Apopharma: Consultancy; PCORI: Research Funding; NHLBI: Research Funding; Bluebird Bio: Research Funding; Sancillo: Research Funding; Seattle Children's Research Grants: Research Funding; Doris Duke Foundation: Research Funding; Novartis: Research Funding; Bayer: Consultancy; Celgene: Research Funding; Imara: Research Funding; Sangamo: Research Funding; Silarus: Research Funding; Pfizer: Consultancy, Research Funding; Emmaus: Consultancy; CTD Holdings: Consultancy; GBT: Research Funding; La Jolla Pharmaceuticals: Research Funding; HRSA: Research Funding; CDC: Research Funding. Meier:CVS Caremark: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal