Pegylated interferon (Peg-IFN) increases molecular response rates when used in combination with imatinib (IM) and dasatinib compared with tyrosine kinase inhibitor (TKI) monotherapy in de novo chronic phase chronic myeloid leukemia (CP-CML). (Preudhomme NEJM 2010, Hjorth-Hansen Leukemia 2016). The phase II Pinnacle (ALLG CML 11) study evaluated the tolerability and molecular response rate of nilotinib (NIL) with Peg-IFN alfa-2B (PegIntron, MSD) in CP-CML patients. Co-primary end points were MMR (BCR-ABL1 ≤ 0.1%) at 12 mths and MR4.5 (BCR-ABL1 ≤ 0.0032%) at 24 mths. Key secondary end points were survival and overall molecular response.
Patients were screened for cardiac / vascular disease and associated risk factors at baseline (EKG, left ventricular ejection fraction, arterial duplex of carotids and lower limbs, blood HbA1c and lipid profiles). Those with uncontrolled vascular risk factors (diabetes, hypertension, dyslipidemia) or a history of vascular events were excluded. Eligible pts received NIL 300mg BID alone for the first 3 months (mths). PegIntron was then added at 30mcg/week in pts without persistent hematological toxicities, increasing to 50mcg/week as tolerated over the following mth. Combination therapy continued until 24 mths, when pts reverted to TKI monotherapy. Switching to IM 400-600mg QD was allowed for pts with persistent grade II or any grade III/IV toxicity from NIL.
Sixty pts were enrolled from 12 Australian centres. Median age was 48.5 years (range 19-72); 45% were female. Sokal risk was low in 43% and high in 18%. Median follow up (FU) was 34 mths (24-60). Data is presented on an intention to treat basis.
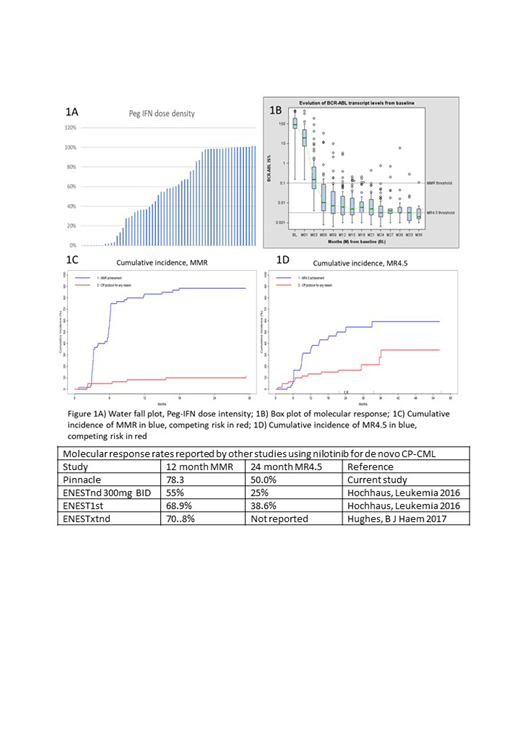
Eight pts (13%) did not commence Pegintron (2 due to persistent haem toxicities, 4 from GI disturbance, liver/pancreatic enzyme derangements, and 2 from pt preference). Considering Pegintron as a product of protocol assigned dose and duration, adjusted for time from study entry, 21 pts (35%) received >85% of their assigned dose, 13 (22%) received between 50-84% and 18 pts (30%) received <50% (Fig 1A). There was no difference between patients who had >85% of their assigned dose versus those wwho took <85% with respect to age or sex. The median duration of Pegintron exposure was 15 mths (Range 1-21 months).
Adverse events (AE) are reported at a similar frequency compared to the interim analysis. Grade III/IV AEs attributed to NIL were increased lipase and neutropenia (each 12%), pancreatitis (6%), thrombocytopenia and rash (each 5%). Grade III/IV AEs attributed to Pegintron were neutropenia (10%), atrial fibrillation (6%), and myalgia, depression and rash (4% each). Three vascular revents occurred: one case each of ischaemic colitis, femoral artery occlusion, coronary artery disease. The former occurred on imaitnib and the latter 2 occurred after 2.5 and 4 years of niloitnib respectively; both patient have since switched to imatinib.
Eighteen pts (30%) have withdrawn from study: 2 withdrew consent, 6 due to intolerance (diarrhoea, pancreatitis, GI upset, rash, high amylase and LFT derangements), 4 for failing to consistently achieve BCR-ABL MMR, 2 for loss of response; 4 pts withdrew for other reasons.
Fig 1B shows BCR-ABL1 transcript levels over time. At 3 mths, 22 (37%) have achieved MMR, 23 (38%) had BCR-ABL between 0.1-1%, and 6 (10%) had BCR-ABL between 1-10%; 3 have already withdrawn. Six pts (10%) had BCR-ABL1 ≥10%; 3 subsequently achieved and maintained MMR, 1 has BCR-ABL <1% at 24 mos, 1 transformed to AP after study withdrawal, and 1 was refractory to all TKIs and received an allograft. At 12 mths, MMR (BCR-ABL ≤ 0.1%) and MR4.5 (BCR-ABL ≤ 0.0032%) rates were 78.3% (95% CI 65.3-88.2; Fig 1C) and 43.3% (95% CI 30.1-57.3%; Fig 1D), respectively. At 24 mths, MR4.5 was 50% (95% CI 36.6-63.4%). No BCR-ABL mutations were reported on study. Three pts lost MMR - 2 were transient; the other was associated with non-compliance. Current TKI treatment for pts on study is NIL (n=37; 62%) and IM (n=5; 8%).
Combination therapy with NIL and Peg-IFN leads to favourable rates of molecular responses that may be superior to NIL monotherapy (Table). While the majority of patients did not durably tolerate full dose Pegintron, there was minimal interference with TKI dose intensity. Such strategies may maximise achievement of deep molecular response, allowing a trial of TKI cessation and the benefit of treatment free remission to an increased number of patients.
Yeung:BMS: Honoraria, Research Funding; Pfizer: Honoraria; Amgen: Honoraria; Novartis: Honoraria, Research Funding. Shanmuganathan:Gilead: Other: Travel Support; Janssen: Other: Travel Support; Amgen: Other: Travel Support; Bristol-Myers Squibb: Honoraria, Other: Travel Support; Novartis: Honoraria, Other: Travel Support. Grigg:Abbvie: Membership on an entity's Board of Directors or advisory committees; Roche: Other: Travel; Janssen: Membership on an entity's Board of Directors or advisory committees; MSD: Membership on an entity's Board of Directors or advisory committees. Reynolds:AUSTRALASIAN LEUKAEMIA & LYMPHOMA GROUP (ALLG): Consultancy; Novartis AG: Equity Ownership; Novartis Australia: Honoraria; Alfred Health: Employment, Other: Biostatistician for trials funded by the Australian government and Abbvie, Amgen, Celgene, GSK, Janssen-Cilag, Merck, Novartis, Takeda, but sponsored by Alfred Health.. Harrup:Cooperative Trial Group for NeuroOncolog: Other: Collaborative Clinical Trials Group; Cancer Council of Tasmania: Membership on an entity's Board of Directors or advisory committees. Ross:BMS: Honoraria, Membership on an entity's Board of Directors or advisory committees; Celgene: Honoraria, Research Funding; Novartis: Consultancy, Honoraria, Research Funding. Mills:Novartis: Other: Speaker Fees; Specialised Therapeutics: Honoraria; Abbvie: Membership on an entity's Board of Directors or advisory committees; Amgen: Other: Conference Sponsorship; MSD: Membership on an entity's Board of Directors or advisory committees. Yong:BMS: Honoraria, Research Funding; Celgene: Research Funding; Novartis: Honoraria, Research Funding. White:BMS: Honoraria, Research Funding; AMGEN: Honoraria, Speakers Bureau. Branford:Qiagen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Cepheid: Honoraria; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; BMS: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Hughes:Novartis, Bristol-Myers Squibb, Celgene: Research Funding; Novartis, Bristol-Myers Squibb: Consultancy, Other: Travel.
Pegylated interferon is not registered for use in chronic phase CML
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal