Background: Multiple myeloma (MM) is an incurable plasma cell malignancies despite the advent of numerously new drugs especially for high risk patients. Our previous study showed good response for the de novo high risk patients who received CD19 and BCMA-specific CART cell therapy after ASCT in the front line with mild CRS and other side effects (reported on the 2018 ASH meeting). To determine the best time to do ASCT and CART cell treatment for those patients, we retrospectively analyzed the patients' outcome according to their time to do autologous transplantation (NCT 03455972).
Methods:The high risk MM patients defined in this study were in R-ISS stage III, IgD/IgE type, or with measurable EMD,or who only achieved PR or less after 4 cycles of triplet induction or relapsed. Lymphocytes were collected from PBSCs and cultured with an anti-CD3 monoclonal antibody to activate T-cell proliferation after stem cell collection. The cells were transduced with recombinant lentiviral verctors which respectively contained the anti-BCMA or anti-CD19 single chain variable fragment (scFv), the cytoplasmic portion of the OX40 and CD28 costimulatory moiety, and the CD3z T-cell activation domain. This is the new third generation CAR technique applied in clinic. BuCy or Melphalan were used as conditioning, followed by infusion of autologous stem cells. CART-19 (1×107/kg on d0) and CART-BCMA cells as split-dose (40% on d1 and 60% on d2) were infused directly on d14 to d20 after transplantation. The cytokine release syndrome (CRS) was graded according to the UPen cytokine release syndrome grading system. Neurotoxic side effects and other toxicities were assessed according to the CARTOX and CTCAE v 4.03. Plasma levels of IL-2, IL-4, IL-6, IL-10, TNF-alpha, IFN-gamma, and IL-17A proteins were determined with a cytokine kit. IMiDs alone were given as maintenance therapy. Responses were assessed by IMWG criteria. 10-color flow cytometry was used to monitor MRD regularly after CART treatment. The median of follow-up was 13 (1~23) months.
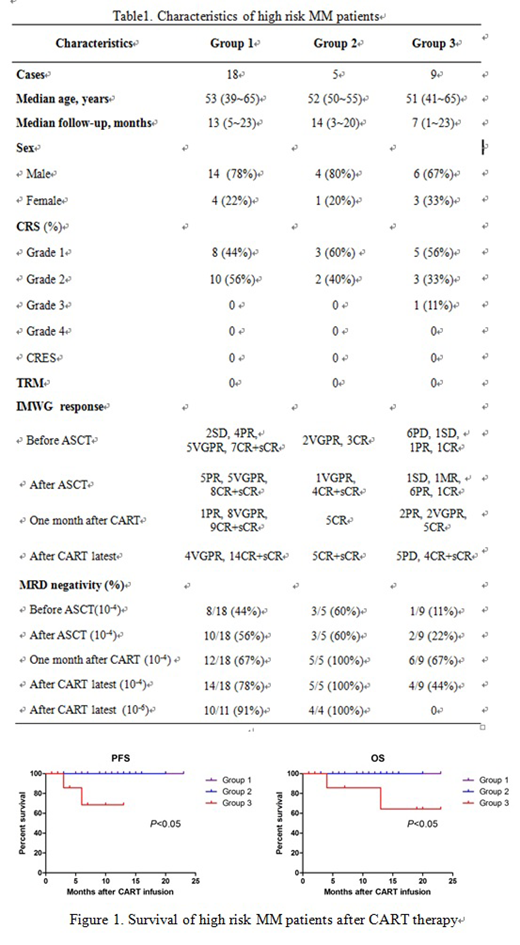
Results: To date, 32 patients have completed the CART cells infusion (Table 1). The median age was 53 years with 24 male and 8 female. CRS occurred in 31 patients (97%) with grade 1 or 2 and just 1 patient (3%) with grade 3. Tocilizumab was used to treating only one patient with grade 3 CRS. Six patients needed to use low-dose vascular active drugs. Other acute and chronic toxicities were slight and reversible. The ORR was 100% (32/32) in this study, with 72% of patients achieved CR or above. There was no TRM or neurologic complications or administration of corticosteroid.
All patients were divided into three groups according to their time to transplant. Group 1 underwent ASCT and CART cell treatment as first line therapy; Group 2 underwent ASCT and CART cell treatment at second line because of induction failure or re-induction after PD or relapse; Group 3 underwent salvage ASCT and CART treatment at third line or more after disease progress or relapse.With a median follow-up of 13 months, the latest response of CR and above were 78% in group 1, 100% in group 2 and 44% in group 3. Except the group 3 patients, MRD negativity in BM of the other two groups increased continuously after CART therapy, and some patients achieved MRD negativity at the level 10-6 (shown in Table 1). Patients in group 1 and 2 were in continuous response but 5/9 (56%) patients relapsed in group 3 and 2 patients died of disease. The median PFS and OS of the patients in three groups were all not reached but 1-year PFS was 100%, 100%, 68% for group1, 2, 3 respectively (p<0.05); 2-year OS was 100%, 100%, 64% for each group (p<0.05) (Figure 1).
Conclusions: Combined infusion of anti-CD19 and anti-BCMA CART cells after ASCT for high risk MM was safe and effective, especially as conjunction therapy to early or later transplant at front line even with primary resistant disease or early disease progress. For those RRMM patients, CART cell therapy followed by ASCT seems to be better to prolong patients' PFS than CART treatment alone with FC chemotherapy reported in our another study (NCT 03196414).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal