Background: Allogeneic transplant (alloHCT) is a curative therapy for patients with acute lymphocytic leukemia (ALL). However, the curative potential of alloHCT is hampered by relapse, which is the major cause of treatment failure. Risk factors for relapse include minimal residual disease (MRD) before or after allogeneic transplantation, patients transplanted in second complete remission or beyond, and reduced intensity conditioning (RIC) regimens. Overall, relapse rates for these patients are in the range of 30% to 50% with the majority of these relapses occurring within the first year after alloHCT. After relapse, the options for disease control are limited and overall survival rates are poor. Currently, there are no standard post-transplant therapy for patients with ALL to reduce the likelihood of relapse. Post alloHCT maintenance approaches may provide time for the graft-versus-leukemia effect to develop, while possibly treating minimal-residual disease, prolonging leukemia-free-survival and decreasing relapse rates.
Inotuzumab ozogamicin (INO) is a CD22 monoclonal antibody bound to calicheamicin which has been shown to have significant activity against relapsed ALL. INO has also been used in patients with relapsed / refractory ALL in a phase 3 randomized clinical trial with an overall CR rate of 81% in the INO arm compared to 29% in the standard arm. We hypothesize that low dose post-alloHCT maintenance therapy of INO will be safe and will reduce relapse rates after alloHCT for ALL. Once the appropriate dose has been found, the study will expand to a phase II.
Methods: Eligibility included patients aged 16-75 who have undergone all-HCT for CD22+ALL in complete remission, have a high risk for relapse after alloHCT, have adequate graft and organ function, are between day 40 and 100 post-transplant, do not have active grade III/IV GVHD or any active GVHD of the liver, and have no history of VOD. The primary objective of this phase I clinical trial is to define a post-alloHCT maximum tolerated dose (MTD) of INO. Secondary objectives include describing the safety profile of INO post-alloHCT, determining the rate of veno-occlusive disease in this setting, evaluating non-relapse mortality (NRM), disease free survival (DFS) and overall survival (OS) at 1 year post-alloHCT, determining the incidence of myeloid toxicity and secondary graft failure, and determining if INO at these doses are effective at eradicating MRD in this cohort of patients.
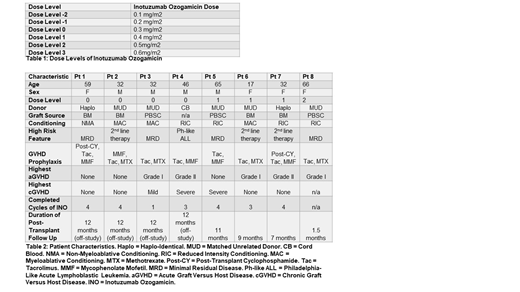
Pre-treatment tests include a bone marrow biopsy and aspirate to assess disease state and MRD. The trial design is a 3+3 model. The study treatment consists of a total of four 28 day cycles of INO starting at dose level 0 (0.3mg/m2) given on day 1. The first cycle must be initiated between day 40 and 100 after alloHCT. Dose limiting toxicities (DLT) include VOD, prolonged cytopenia (more than 28 days), and death. If there are no DLTs experienced in a cohort, patients may be enrolled in the next highest dose level (Table 1). Patients will be monitored with routine blood work during each cycle. At 1 year after alloHCT, patients will be assessed by restaging bone marrow biopsy and aspirate.
Results: As of July 29th, 2019, 8 patients have been treated. One patient went off treatment after 1 cycle of INO (patient choice) and two went off treatment after 3 cycles of INO (patient choice and physician choice). All continued to be followed for safety. We have completed 1 year post-transplant follow up on 4 patients. All patients are alive and in CR. No patients experienced VOD or other DLTs. Significant side effects include thrombocytopenia and neutropenia. The percentage of any aGVHD is 62.5% and the rate of grade III/IV aGVHD is 0%. The percentage of any cGVHD is 42.8%. Patient characteristics are described below (Table 2).
Conclusions: In this phase 1 study, INO at doses of 0.3 and 0.4mg/m2 was well tolerated. Thrombocytopenia may be the dose limiting toxicity. The absence of disease recurrence in this small cohort of high risk ALL patients is very promising.
Metheny:Takeda: Speakers Bureau; Incyte: Speakers Bureau. Majhail:Anthem, Inc.: Consultancy; Mallinckrodt: Honoraria; Nkarta: Consultancy; Incyte: Consultancy; Atara Bio: Consultancy. Malek:Adaptive: Consultancy; Amgen: Speakers Bureau; Celgene: Consultancy; Takeda: Consultancy; Sanofi: Consultancy; Medpacto: Research Funding; Janssen: Speakers Bureau. Gerds:Roche: Research Funding; Pfizer: Consultancy; CTI Biopharma: Consultancy, Research Funding; Celgene Corporation: Consultancy, Research Funding; Imago Biosciences: Research Funding; Incyte: Consultancy, Research Funding; Sierra Oncology: Research Funding.
Low dose inotuzuamb ozogamicin in the post-allogeneic transplant setting for patients with ALL.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal