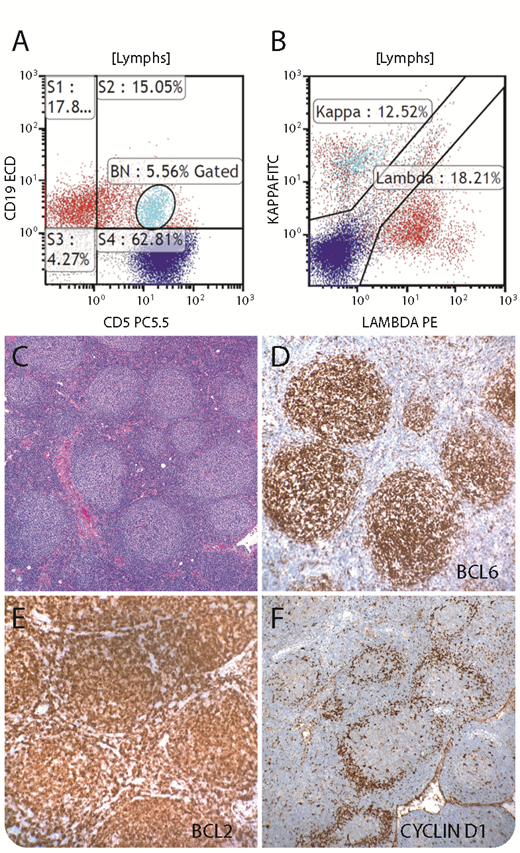
A 76-year-old man with a recent diagnosis of prostate carcinoma was found to have extensive lymphadenopathy, including the axillary region and mediastinum. Flow cytometry of axillary lymph node (LN) demonstrated 2 clonal B-cell populations: 1 small population was CD19+/κ+/CD5+/dim CD20+/CD23−/ FMC7−/CD10− (light blue, panels A-B), and a larger population was CD19+/λ+/CD5−/FMC7−/CD23+/CD20+/CD38+/CD10− (red, panels A-B). The LN showed effacement of the architecture by a nodular infiltrate of small cleaved lymphocytes with extracapsular extension (panel C; original magnification ×100; hematoxylin and eosin stain). Centroblasts were rare. CD21 stain highlighted the prominent follicular pattern of the infiltrate, and the infiltrate was CD20+/CD79a+/PAX5+/CD10 weak+/BCL6+ (panel D; original magnification ×200)/BCL2+ (panel E; original magnification ×200)/CD5−/CD23 weak+/cyclin D1−/Ki-67 (20%), consistent with follicular lymphoma, grade 1-2. Interestingly, rare lymphoid follicles showed a population of cyclin D1+ cells colonizing the mantle zone (panel F; original magnification ×100), consistent with in situ mantle cell neoplasia. Bone marrow and gastric biopsies showed involvement by follicular lymphoma. Evidence of mantle cell lymphoma was not identified.
In situ mantle cell neoplasia is rare and can be associated with other lymphomas. It is usually an incidental finding that is only unveiled by flow cytometry and immunohistochemistry studies. The course is indolent. Only rare cases progress to overt lymphoma. This case emphasizes the importance of utilizing multiple tools in the lymphoma diagnosis.
A 76-year-old man with a recent diagnosis of prostate carcinoma was found to have extensive lymphadenopathy, including the axillary region and mediastinum. Flow cytometry of axillary lymph node (LN) demonstrated 2 clonal B-cell populations: 1 small population was CD19+/κ+/CD5+/dim CD20+/CD23−/ FMC7−/CD10− (light blue, panels A-B), and a larger population was CD19+/λ+/CD5−/FMC7−/CD23+/CD20+/CD38+/CD10− (red, panels A-B). The LN showed effacement of the architecture by a nodular infiltrate of small cleaved lymphocytes with extracapsular extension (panel C; original magnification ×100; hematoxylin and eosin stain). Centroblasts were rare. CD21 stain highlighted the prominent follicular pattern of the infiltrate, and the infiltrate was CD20+/CD79a+/PAX5+/CD10 weak+/BCL6+ (panel D; original magnification ×200)/BCL2+ (panel E; original magnification ×200)/CD5−/CD23 weak+/cyclin D1−/Ki-67 (20%), consistent with follicular lymphoma, grade 1-2. Interestingly, rare lymphoid follicles showed a population of cyclin D1+ cells colonizing the mantle zone (panel F; original magnification ×100), consistent with in situ mantle cell neoplasia. Bone marrow and gastric biopsies showed involvement by follicular lymphoma. Evidence of mantle cell lymphoma was not identified.
In situ mantle cell neoplasia is rare and can be associated with other lymphomas. It is usually an incidental finding that is only unveiled by flow cytometry and immunohistochemistry studies. The course is indolent. Only rare cases progress to overt lymphoma. This case emphasizes the importance of utilizing multiple tools in the lymphoma diagnosis.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal