In this issue of Blood, Siwaponanan et al provide a potential novel mechanism for the increased infections observed in patients with β-thalassemia.1 The authors find that neutrophils in 6-month-old β-thalassemic mice (Hbbth3/+) and in patients have overall lower baseline levels of the ets-family transcription factor PU.1, and in mice lack upregulated Pu.1 expression in response to bacterial infection. This aberrant Pu.1 expression in mouse Hbbth3/+ neutrophils is accompanied by defects in chemotaxis, phagocytosis, and production of reactive oxygen species (ROS).
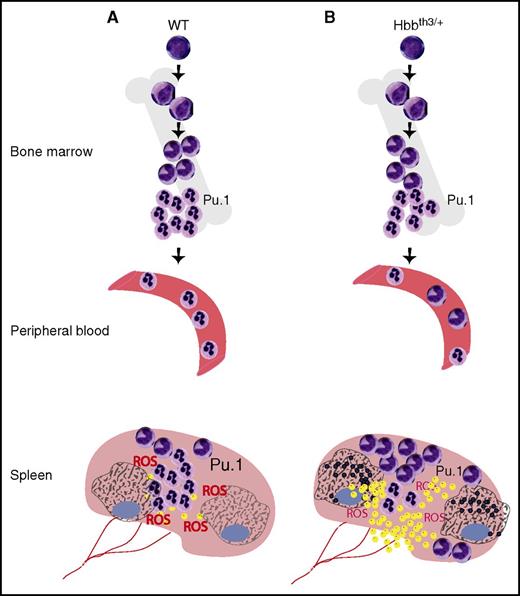
Neutrophil dysfunction in β-thalassemia. In WT mice (A), neutrophils mature normally and are released into peripheral blood. Similarly, in the spleen, the majority of neutrophils are mature, and efficiently phagocytose and kill bacteria (yellow dots), along with production and release of abundant ROS. Macrophages intricately interact with neutrophils to resolve the infection. In older mice with β-thalassemia (B) that have developed iron overload, BM neutrophils are normal, but in peripheral blood and spleen, immature neutrophils accumulate. In the spleen, these immature neutrophils have decreased Pu.1 expression, fail to upregulate Pu.1 upon activation by bacterial infection, and produce deficient levels of ROS. They fail to phagocytose bacteria, and mice succumb to infection. Meanwhile, macrophages in the spleen are iron loaded (indicated by black dots) and may compound the deficiencies in the innate immune system observed in patients with β-thalassemia.9
Neutrophil dysfunction in β-thalassemia. In WT mice (A), neutrophils mature normally and are released into peripheral blood. Similarly, in the spleen, the majority of neutrophils are mature, and efficiently phagocytose and kill bacteria (yellow dots), along with production and release of abundant ROS. Macrophages intricately interact with neutrophils to resolve the infection. In older mice with β-thalassemia (B) that have developed iron overload, BM neutrophils are normal, but in peripheral blood and spleen, immature neutrophils accumulate. In the spleen, these immature neutrophils have decreased Pu.1 expression, fail to upregulate Pu.1 upon activation by bacterial infection, and produce deficient levels of ROS. They fail to phagocytose bacteria, and mice succumb to infection. Meanwhile, macrophages in the spleen are iron loaded (indicated by black dots) and may compound the deficiencies in the innate immune system observed in patients with β-thalassemia.9
It has long been recognized that patients with β-thalassemia suffer from increased infection.2,3 Granulocyte dysfunction has been described among other predisposing factors that include splenectomy, iron overload, and treatment with deferoxamine. But the underlying molecular cause(s) of neutrophil dysfunction in β-thalassemic patients has yet to be elucidated. To determine whether neutrophil dysfunction is directly linked to the β-thalassemic genetic disorder, Siwaponanan et al closely examine distinct neutrophil populations in the bone marrow (BM), spleen, and peripheral blood in Hbbth3/+ mice based on the commonly used criteria of cell surface Ly6G vs Ly6C expression (eg, Ly6Ghigh/Ly6Clow). Although they find that BM-derived neutrophils in Hbbth3/+ mice do not differ from their wild-type (WT) counterparts, peripheral blood and spleen neutrophils exhibit nuclear hypolobulation and deficient chemotaxis in response to CXCL2 due to reduced expression of CXCR2, the receptor for CXCL2. Splenic neutrophils in Hbbth3/+ mice also express lower levels of the integrin CD11b, explaining at least in part their reduced phagocytic capacity. Finally, splenic neutrophils from Hbbth3/+ mice display reduced ROS production secondary to reduced expression of all essential components of the NAD phosphate-oxidase machinery.
Terminal neutrophil differentiation and maturation is a tightly controlled process directed by several key transcription factors, including C/EBPα, Pu.1, and C/EBPε.4,5 Given the broad defects observed in neutrophils from Hbbth3/+ mice, Siwaponanan et al explore whether these defects may be due to aberrant maturation caused at the level of transcriptional control. They focus on the ets transcription factor that regulates monocytic-granulocytic lineage choice and maturation, Pu.1. They find not only reduced expression at baseline, but also lack of upregulation in response to infection, again restricted to spleen-derived neutrophils. When challenged with Streptococcus pneumoniae infection in vivo, all Hbbth3/+ mice succumb with accumulation of bacteria in spleen and liver, although WT mice survive. This suggests that the splenic neutrophil population plays a critical role in S. pneumoniae clearance, which is severely disrupted in β-thalassemia mice (see figure).
To address what factors might lead to the neutrophil defects in β-thalassemia, Siwaponanan et al perform the same studies in young, 6-week-old Hbbth3/+ mice. They find that young Hbbth3/+ mice have normal neutrophil functions and histologies, whereas the aged 6-month-old Hbbth3/+ mice exhibit extensive iron accumulation and disrupted splenic architecture with accumulation of immature myeloid cells. This data is consistent with the observed correlation between iron overload and infection risk in thalassemic patients,2 and is further supported by the increase in hypolobated neutrophils in nonsplenectomized and splenectomized patients with hemoglobin E/β-thalassemic subjects in this study.
Now that Siwaponanan et al have established a link between iron overload and neutrophil dysfunction and have implicated dysregulation of Pu.1 in β-thalassemia, several questions arise. First and foremost: how might iron overload result in dysregulation of Pu.1? Pu.1 is one of the master regulators in hematopoiesis; in conjunction with a versatile array of key transcription factors, Pu.1 directs several lineage choices, including those between the myeloid and lymphoid lineages and between monocytes and granulocytes.5 But is Pu.1 the only factor that controls lineage choice and neutrophil maturation that is affected by β-thalassemia and iron overload? Both Pu.1 and the neutrophil-specific factor C/EBPε cooperate with additional regulators (eg, Gabp) to control neutrophil-expressed genes such as CD11b and granulocyte-colony stimulating factor, among others; might they or additional factors such as Sp1 or retinoid receptors also be involved in the observed defects?4,6,7 How would iron overload uniquely affect neutrophil maturation without affecting lineage choice? Are other cells of the innate immune system affected, in particular macrophages that take up the majority of the iron and are also regulated by Pu.1?
Iron chelation has come a long way. Although parenteral administration of deferoxamine was the sole option only a few years ago, various oral chelators are now available, making prevention of significant iron overload more feasible.8 It will be interesting to see whether neutrophil abnormalities as described here are prevented as well, both in Hbbth3/+ mice and in patients. The authors find an interesting difference between BM- and spleen-derived neutrophils in Hbbth3/+ mice. What is the underlying mechanism, and would one expect the same differences in patients? What is the effect of splenectomy on neutrophil function in thalassemic patients? Red blood cell transfusions with the risk for iron overload are not unique to thalassemia, but are part of the treatment of several inherited and acquired anemias. Studies to determine whether the same neutrophil defect is present in other diseases and models thereof, such as sickle cell disease or hemochromatosis, may shed light on whether this defect in innate immunity is a universal consequence of iron overload and make prevention even more compelling.
Conflict-of-interest disclosure: The authors declare no competing financial interests.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal