Key Points
Monoclonal gammopathy is associated with C3 glomerulopathy.
Specific treatment of the underlying B-cell clone improves renal survival.
Abstract
The high frequency of monoclonal gammopathy in adult patients with C3 glomerulopathy (C3G) emphasizes the role of monoclonal immunoglobulin (MIg) in the occurrence of renal disease and raises the issue of the therapeutic management. The aim of the study was to evaluate the effect of chemotherapy in a large cohort of patients with MIg-associated C3G. Fifty adult patients with MIg and biopsy-proven C3G were extracted from the French national database of C3G. We retrospectively compared renal outcomes in patients who either received or did not receive chemotherapy targeting the underlying B-cell clone. At diagnosis, renal disease was severe, with nephrotic-range proteinuria in 20/46 (43%) patients and chronic kidney disease stage 3 or above in 42/49 (86%) patients. Monoclonal gammopathy was of IgG type in 47 (94%) patients. Hematological diagnosis was monoclonal gammopathy of renal significance in 30 (60%), multiple myeloma in 17 (34%), and chronic lymphocytic leukemia in 3 (6%) patients. Complement studies showed low C3 level in 22/50 (43%) and elevated soluble C5b-9 level in 27/34 (79%) patients. Twenty-nine patients received chemotherapy (including bortezomib in 22), whereas 8 and 13 patients received various immunosuppressive drugs or symptomatic measures alone, respectively. Patients who achieved hematological response after chemotherapy had higher renal response rates (P = .0001) and median renal survival (hazard ratio, 0.22; 95% confidence interval, 0.05-0.92; P = .009) than those receiving conservative/immunosuppressive therapy. In conclusion, our results suggest that chemotherapy adapted to the B-cell clone may constitute an efficient strategy for C3G in the setting of MIg, as rapid achievement of hematological response appears to result in improved renal survival.
Introduction
A wide spectrum of renal manifestations, including glomerular and tubular diseases, may occur in patients with monoclonal gammopathies.1 Except for myeloma cast nephropathy, invariably diagnosed in the setting of symptomatic multiple myeloma (MM), most renal disorders related to deposition or precipitation of a monoclonal immunoglobulin (MIg) occur in patients with indolent B-cell clone, most commonly of plasmocytic origin. The concept of monoclonal gammopathy of renal significance (MGRS) was introduced to depict the spectrum of renal diseases induced by MIg produced by indolent B-cell clones and to highlight the effect of chemotherapy on renal and patient outcomes.1 Trials on MGRS treatment are lacking, and therapeutic recommendations are currently based on consensus expert opinion.2 It has been recently proposed to include C3 glomerulopathy (C3G) in the spectrum of MGRS.1 C3G is a heterogeneous group of rare glomerular diseases characterized by glomerular lesions with predominant complement component C3 fragment deposition without significant Ig deposits.3,4 According to the location and aspect of C3 deposits by immunofluorescence and electron microscopy, 2 different patterns of glomerular diseases, dense deposit disease (DDD), and glomerulonephritis with isolated C3 deposits (C3GN) are distinguished.5,6 Both are associated with dysregulation of complement alternative pathway (AP) because of autoantibodies against complement proteins in most patients.7-10 The association between MIg and C3G has been recently described.11-13 In 2 series, MIg was found in 10/30 and 10/14 patients, indicating that the frequency of MIg in C3G patients older than 50 years largely exceeds that of the age-matched general population, and that the association is probably not fortuitous.11,13 Moreover, improvement of renal parameters after chemotherapy in a few patients suggests MIg could have a pathogenic role in AP activation and that chemotherapy targeting the underlying B-cell clone could favorably influence renal survival.
The aim of the present study was to evaluate renal outcomes after chemotherapy in a large cohort of patients with C3G and MIg.
Subjects and methods
Study population
Between 2000 and 2014, 201 patients older than 18 years were included in the French registry of C3G if complete renal pathological data were available. Patients with positive hepatitis B or C serology and antinuclear or anti-double-stranded DNA antibodies are excluded from the French registry.
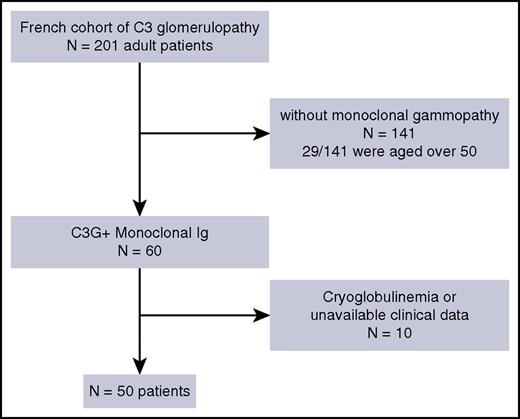
Patients were included in this retrospective study on the basis of the following criteria1 : biopsy-proven C3G on native kidneys or renal allograft without evidence of associated Ig light chain (LC) or heavy chain glomerular deposits, except for trace IgM on glomerular sclerotic lesions by immunofluorescence2 ; detectable serum and/or urine MIg3 ; and availability of clinical data. Patients with cryoglobulinemia were excluded (Figure 1).
Patients’ recruitment. Flowchart of inclusion of patients within the adult population of the French C3G registry (n = 201). A total of 50 patients were eligible for enrollment in the study, based on the presence of monoclonal gammopathy by electrophoresis and immunofixation and the availability of clinical data.
Patients’ recruitment. Flowchart of inclusion of patients within the adult population of the French C3G registry (n = 201). A total of 50 patients were eligible for enrollment in the study, based on the presence of monoclonal gammopathy by electrophoresis and immunofixation and the availability of clinical data.
For analysis, patients were divided into 3 groups according to treatment strategy, which consisted of chemotherapy adapted to the B-cell clone (n = 29), conventional immunosuppressive therapy (n = 8), or blockers of the renin-angiotensin system (n = 13). Demographics and clinical and biological data were recorded at the time of the first kidney biopsy, at initiation of treatment, after completion of first-line treatment, and at last follow-up. Estimated glomerular filtration rate (eGFR) was calculated using the modified MDRD (Modification of Diet in Renal Disease) equation.14 Impaired renal function was defined by an eGFR value of 60 mL/min/m2 or less, and stages of chronic kidney disease (CKD) were assessed according to the US National Kidney Foundation.15 Nephrotic syndrome was defined by urinary protein excretion of 3 g/24 h or more or a urine protein-to-creatinine ratio of 3 g/g or higher and serum albumin levels of 30 g/L or lower.
Pathological studies
All kidney biopsy samples were processed for light and immunofluorescence microscopy. Immunofluorescence study was performed on sections directly frozen in liquid nitrogen (without transport in Michel’s medium), using conjugates specific for α, γ, and µ Ig heavy chains; κ and λ Ig light chains (Dakopatts, Glostrup, Denmark); C3; C4; C1q; and albumin (Morphosys AbD, Düsseldorf, Germany). Electron microscopy was available in 25 cases.
The diagnosis of C3G was assessed by immunofluorescence, according to consensus recommendations, with bright diffuse predominant C3 glomerular staining (≥2+) of at least 2 orders of magnitude greater than any other immune reactant (ie, Ig). Patients with trace or weak amounts of IgM staining on glomerular sclerotic lesions were included, but those with weak staining for IgG, IgA, or Ig light chains were excluded.5 The diagnosis of DDD was confirmed by demonstration of diffuse, highly electron-dense osmiophilic deposits within the lamina densa by electron microscopy. In contrast, the diagnosis of C3GN was established in patients showing deposits of lesser density without the characteristic distribution and “sausage shape” appearance of DDD.
Hematologic studies
Serum MIg were detected and quantified by electrophoresis and characterized by immunofixation. Serum free LCs (FLCs) were monitored in 32 patients (Binding Site, Birmingham, United Kingdom). Abnormal FLC ratio was defined as a κ/λ ratio lower than 0.26 or higher than 1.65. Bone marrow smears and/or biopsy were performed in all cases, and clonality of plasma cells was tested by immunofluorescence (n = 2) or flow cytometry (n = 48). The diagnosis of MGRS, MM and chronic lymphocytic leukemia (CLL) was established according to international criteria.16-18
Local ethics committees approved research, and all patients gave written informed consent.
Definition of renal and hematological responses
Renal response was assessed based on Kidney Disease: Improving Global Outcomes practice guidelines on glomerulonephritis.19 Complete renal response was defined by proteinuria levels of 0.5 g/24 h or less, with albuminemia levels of 30 g/L or more and no more than 10% decrease in eGFR from baseline value. Partial renal response was defined by posttreatment proteinuria between 0.5 and 2.5 g/24 h or by a 50% or more reduction from baseline value, with albuminemia levels of 25 g/L or more and no more than a 10% decrease in eGFR from baseline value.
Hematological response was assessed according to the International Myeloma Working Group for patients with symptomatic MM.20 In patients with MGRS, response criteria were adapted from the 2012 International Society of Amyloidosis criteria21 : complete hematological response was defined by negative immunofixation of serum and urine with normal FLC ratio, very good partial response was defined by a 90% or more reduction of serum MIg and/or a 90% or more decrease in the difference between the concentration of the involved and uninvolved FLC (dFLC), and partial hematological response was defined by a 50% or more reduction of serum MIg and/or a 50% or more dFLC decrease.
Assays for complement component and genetic screening
All immunological and genetic analyses were performed at the reference laboratory for investigation of the complement system (European Hospital Georges Pompidou, France). EDTA plasma samples were obtained from all patients. Plasma C3 and C4 levels were measured as previously described.22 Soluble C5b-9 (sC5b-9) level was determined using the MicroVue sC5b-9 Plus EIA Assay (Quidel, San Diego, CA), according to manufacturer’s instructions. Normal values were evaluated after testing plasma from 100 healthy donors.
C3 nephritic factor activity was determined by assessing the ability of purified plasma IgG to stabilize membrane-bound C3bBb convertase.23 Titers of anti-Factor H (FH) IgG or IgA antibodies were determined by ELISA. Direct sequencing of all CFH, CFI, CD46, and C3 exons was undertaken in 28 patients with available DNA, as previously described.22
Statistical analysis
Data are expressed as median for continuous variables and percentage for categorical variables. Statistical analysis was performed using the Student t test and Mann-Whitney and Kruskal-Wallis tests, as appropriate, for comparison of continuous variables, and using chi-square or Fisher’s exact tests for the comparison of categorical variables. Survival analysis was performed by the Kaplan-Meier method, using the log-rank test for comparison of groups. P values below .05 were considered significant. Results were analyzed using the Graph Pad Prism software.
Contribution to various factors to the probability of renal response was assessed using univariate and multivariate logistic regression model, using the R function glm. The contribution to end-stage renal disease (ESRD) was assessed using Cox proportional hazards models, both univariate and multivariate, computed using the R package survival.
Results
Epidemiological data
In the French cohort of 201 C3G patients, 60 (29.8%) had a monoclonal gammopathy. Among them, 50 patients were included in the study (including 6 patients described in Bridoux et al.)12 (Figure 1). We excluded 10 patients because of positive cryoglobulinemia (n = 4) and/or unavailable clinical data (n = 8). On the remaining 141 C3G patients without monoclonal gammopathy, only 29 were older than 50 years at the time of diagnosis. The prevalence of MIg in patients with C3G older than 50 years was 59% and increased at each decade, reaching 36%, 59%, and 94% of C3G patients within the age ranges of 50 to 59, 60 to 69, and 70 to 79 years, respectively (supplemental Figure 1, available on the Blood web site).
Clinical features and laboratory evaluation of patients at time of kidney biopsy and at onset of treatment
Median serum creatinine was 158 (68-990) μmol/L with eGFR of 37 (3-100) mL/min/1.73 m2. Forty-two patients (86%) presented with CKD, including 15/49 (31%) with CKD stage 3 and 27/49 (55%) with CKD stage 4 or 5. At diagnosis, 20/46 (43%) patients had nephrotic-range proteinuria (Table 1). Renal parameters at diagnosis were similar among patients who received chemotherapy, immunosuppressive therapy, or conservative treatment (Table 1). Comparison of renal parameters in patients who received chemotherapy or immunosuppressive/conservative treatment are detailed in supplemental Table 1.
Main demographic, clinical, and biological data at time of kidney biopsy and at onset of treatment
| . | All patients (N = 50) . | Chemotherapy (N = 29) . | IS therapy (N = 8) . | Conservative treatment (N = 13) . | P value . |
|---|---|---|---|---|---|
| Age, y | 65 (38-82) | 69 (36-83) | 64 (57-70) | 60 (40-77) | .58 |
| Male, n (%) | 33 (66%) | 18 (62%) | 5 (75%) | 10 (77%) | .62 |
| Renal manifestations at diagnosis | |||||
| Serum creatinine, µmol/L | 158 (68-990) | 158 (68-990) | 168 (135-280) | 150 (70-317) | .59 |
| eGFR, ml/min/1.73 m2 | 37 (3-100) | 37 (3-94) | 32 (20-49) | 39 (16-100) | .51 |
| CKD stage 1-2 | 8/49 (16%) | 10/28 (36%) | 0 (0%) | 2 (15%) | .07 |
| CKD stage 3 | 15/49 (31%) | 5 /28 (18%) | 3 (37%) | 7 (54%) | .06 |
| CKD stage 4-5 | 27/49 (55%) | 13/28 (46%) | 5 (63%) | 4 (31%) | .35 |
| Nephrotic syndrome, n (%) | 20/46 (43%) | 14/22 (63%) | 3 (38%) | 3/11 (27%) | .11 |
| 24-h proteinuria, g | 3.15 (0.1-14) | 4 (0.7-14) | 1.7 (0.4-10) | 1.8 (0.1-10) | .06 |
| Hematuria, n (%) | 33/39 (84%) | 19/24 (79%) | 6/6 (100%) | 8/9 (89%) | .41 |
| Renal manifestations at onset of treatment | |||||
| Serum creatinine, mmol/L | — | 202 (68-990) | 198 (70-450) | — | .47 |
| eGFR, ml/min/1.73 m2 | — | 28 (4-100) | 29 (11-100) | — | .32 |
| CKD stage 1-2 | — | 6 (21%) | 0 (0%) | — | .71 |
| CKD stage 3 | — | 9 (31%) | 1 (13%) | — | .76 |
| CKD stage 4-5 | — | 14 (48%) | 7 (87%) | — | 1 |
| Nephrotic syndrome, n (%) | — | 17 (58%) | 5 (65%) | — | .37 |
| 24-h proteinuria, g | — | 3.55 (0.7-13) | 2.91 (0.6-10) | — | .06 |
| Hematological findings | |||||
| Serum monoclonal Ig, n (%) | |||||
| IgG κ | 36 (71%) | 24 (80%) | 5 (67%) | 7 (54%) | .12 |
| IgG λ | 11 (22%) | 3 (10%) | 3 (38%) | 5 (38%) | .06 |
| IgA κ | 1 (2%) | 0 (0%) | 0 (0%) | 1 (8%) | 1 |
| IgA λ | 1 (2%) | 1 (3%) | 0 (0%) | 0 (0%) | 1 |
| λ LC only | 1 (2%) | 1 (3%) | 0 (0%) | 0 (0%) | 1 |
| Abnormal FLC, n (%) | 17/32 (53%) | 12/22 (55%) | 2/3 (67%) | 3/7 (43%) | .76 |
| dFLC, mg/L | 79 (2-20800) | 79 (6-20800) | 114 (15-959) | 22 (2-820) | .55 |
| MIg concentration, g/L | 10.2 (2-38) | 11 (2-38) | 6 (2-15) | 9 (3-30) | |
| Underlying hematological disorder, n (%) | |||||
| MGRS | 30 (60%) | 12 (41%) | 7 (88%) | 11 (84%) | .006 |
| Smoldering MM | 15 (30%) | 13 (43%) | 1 (14%) | 1 (8%) | .02 |
| Symptomatic MM | 2 (4%) | 2 (7%) | 0 (0%) | 0 (0%) | .47 |
| CLL | 3 (6%) | 2 (7%) | 0 (0%) | 1 (8%) | 1 |
| Extra renal manifestations, n (%) | 5 (10%) | 5 (17%)* | 0 (0%) | 0 (0%) | .13 |
| Biological thrombotic microangiopathy, n (%) | 3 (6%) | 3 (10%) | 0 (0%) | 0 (0%) | .31 |
| Immunological findings | |||||
| C3 level, mg/L | 746 (78-1130) | 689 (78-1220) | 866 (410-1120) | 682 (473-1130) | .95 |
| Low C3 level, n (%) | 22 (43%) | 14 (48%) | 3 (38%) | 7 (46%) | .76 |
| C4 level, mg/L | 250 (104-575) | 243 (109-575) | 265 (193-321) | 282 (104-376) | .82 |
| sC5b-9, ng/mL | 734 (164-2370) | 961 (164-2370) | 705 (269-1035) | 535 (266-960) | .17 |
| Elevated sC5b-9, upper 420 ng/mL | 27/34 (79%) | 15/18 (83%) | 6/7 (86%) | 6/9 (67%) | .42 |
| C3Nef, n (%) | 3 (6%) | 1 (3%) | 1 (14%) | 1 (8%) | .6 |
| Anti-FH antibody, n (%) | 9 (19%) | 4 (14%) | 3 (38%) | 2 (15%) | .29 |
| Pattern of glomerular disease by electron microscopy | |||||
| C3GN | 24/25 (96%) | 18/19 (95%) | — | 6/6 (100%) | 1 |
| DDD | 1/25 (4%) | 1/19 (5%) | — | 0 (0%) | 1 |
| . | All patients (N = 50) . | Chemotherapy (N = 29) . | IS therapy (N = 8) . | Conservative treatment (N = 13) . | P value . |
|---|---|---|---|---|---|
| Age, y | 65 (38-82) | 69 (36-83) | 64 (57-70) | 60 (40-77) | .58 |
| Male, n (%) | 33 (66%) | 18 (62%) | 5 (75%) | 10 (77%) | .62 |
| Renal manifestations at diagnosis | |||||
| Serum creatinine, µmol/L | 158 (68-990) | 158 (68-990) | 168 (135-280) | 150 (70-317) | .59 |
| eGFR, ml/min/1.73 m2 | 37 (3-100) | 37 (3-94) | 32 (20-49) | 39 (16-100) | .51 |
| CKD stage 1-2 | 8/49 (16%) | 10/28 (36%) | 0 (0%) | 2 (15%) | .07 |
| CKD stage 3 | 15/49 (31%) | 5 /28 (18%) | 3 (37%) | 7 (54%) | .06 |
| CKD stage 4-5 | 27/49 (55%) | 13/28 (46%) | 5 (63%) | 4 (31%) | .35 |
| Nephrotic syndrome, n (%) | 20/46 (43%) | 14/22 (63%) | 3 (38%) | 3/11 (27%) | .11 |
| 24-h proteinuria, g | 3.15 (0.1-14) | 4 (0.7-14) | 1.7 (0.4-10) | 1.8 (0.1-10) | .06 |
| Hematuria, n (%) | 33/39 (84%) | 19/24 (79%) | 6/6 (100%) | 8/9 (89%) | .41 |
| Renal manifestations at onset of treatment | |||||
| Serum creatinine, mmol/L | — | 202 (68-990) | 198 (70-450) | — | .47 |
| eGFR, ml/min/1.73 m2 | — | 28 (4-100) | 29 (11-100) | — | .32 |
| CKD stage 1-2 | — | 6 (21%) | 0 (0%) | — | .71 |
| CKD stage 3 | — | 9 (31%) | 1 (13%) | — | .76 |
| CKD stage 4-5 | — | 14 (48%) | 7 (87%) | — | 1 |
| Nephrotic syndrome, n (%) | — | 17 (58%) | 5 (65%) | — | .37 |
| 24-h proteinuria, g | — | 3.55 (0.7-13) | 2.91 (0.6-10) | — | .06 |
| Hematological findings | |||||
| Serum monoclonal Ig, n (%) | |||||
| IgG κ | 36 (71%) | 24 (80%) | 5 (67%) | 7 (54%) | .12 |
| IgG λ | 11 (22%) | 3 (10%) | 3 (38%) | 5 (38%) | .06 |
| IgA κ | 1 (2%) | 0 (0%) | 0 (0%) | 1 (8%) | 1 |
| IgA λ | 1 (2%) | 1 (3%) | 0 (0%) | 0 (0%) | 1 |
| λ LC only | 1 (2%) | 1 (3%) | 0 (0%) | 0 (0%) | 1 |
| Abnormal FLC, n (%) | 17/32 (53%) | 12/22 (55%) | 2/3 (67%) | 3/7 (43%) | .76 |
| dFLC, mg/L | 79 (2-20800) | 79 (6-20800) | 114 (15-959) | 22 (2-820) | .55 |
| MIg concentration, g/L | 10.2 (2-38) | 11 (2-38) | 6 (2-15) | 9 (3-30) | |
| Underlying hematological disorder, n (%) | |||||
| MGRS | 30 (60%) | 12 (41%) | 7 (88%) | 11 (84%) | .006 |
| Smoldering MM | 15 (30%) | 13 (43%) | 1 (14%) | 1 (8%) | .02 |
| Symptomatic MM | 2 (4%) | 2 (7%) | 0 (0%) | 0 (0%) | .47 |
| CLL | 3 (6%) | 2 (7%) | 0 (0%) | 1 (8%) | 1 |
| Extra renal manifestations, n (%) | 5 (10%) | 5 (17%)* | 0 (0%) | 0 (0%) | .13 |
| Biological thrombotic microangiopathy, n (%) | 3 (6%) | 3 (10%) | 0 (0%) | 0 (0%) | .31 |
| Immunological findings | |||||
| C3 level, mg/L | 746 (78-1130) | 689 (78-1220) | 866 (410-1120) | 682 (473-1130) | .95 |
| Low C3 level, n (%) | 22 (43%) | 14 (48%) | 3 (38%) | 7 (46%) | .76 |
| C4 level, mg/L | 250 (104-575) | 243 (109-575) | 265 (193-321) | 282 (104-376) | .82 |
| sC5b-9, ng/mL | 734 (164-2370) | 961 (164-2370) | 705 (269-1035) | 535 (266-960) | .17 |
| Elevated sC5b-9, upper 420 ng/mL | 27/34 (79%) | 15/18 (83%) | 6/7 (86%) | 6/9 (67%) | .42 |
| C3Nef, n (%) | 3 (6%) | 1 (3%) | 1 (14%) | 1 (8%) | .6 |
| Anti-FH antibody, n (%) | 9 (19%) | 4 (14%) | 3 (38%) | 2 (15%) | .29 |
| Pattern of glomerular disease by electron microscopy | |||||
| C3GN | 24/25 (96%) | 18/19 (95%) | — | 6/6 (100%) | 1 |
| DDD | 1/25 (4%) | 1/19 (5%) | — | 0 (0%) | 1 |
Values for continuous variables are expressed as median [range], and values for categorical variables, as percentage. Statistical analysis: for contingency, chi2 test, for comparison, Kruskal-Wallis test.
C3Nef, C3 nephritic factor; IS, immunosuppressive.
Diffuse mucinosis (n = 1), digital ischemia (n = 2), skin purpuric lesions (n = 1), and capillary leak syndrome (n = 1).
Median time from diagnosis to treatment initiation was 3 months.1-20 At onset of treatment, in the group of 29 patients treated with chemotherapy, median proteinuria was 3.55 g/day, with median serum creatinine of 202 µmol/L and eGFR of 28 mL/min/1.73 m2, including 6 (21%), 9 (31%), and 14 (48%) with CKD stage 1 to 2, CKD stage 3, and CKD stage 4 to 5, respectively (Table 1). In the 8 patients who received immunosuppressive therapy, at treatment initiation, median proteinuria was 2.9 g/day, with median serum creatinine of 198 µmol/L and eGFR of 29 mL/min/1.73 m2, including 1 (13%) and 7 (87%) patients with CKD stage 3 and CKD stage 4 to 5, respectively. From diagnosis to treatment initiation, 25% or more decrease in eGFR was observed in 8/29 and in 3/8 patients who received chemotherapy or immunosuppressive drugs, respectively.
Five patients had extra renal manifestations, including diffuse mucinosis (n = 1), digital ischemia (n = 2), skin purpuric lesions (n = 1), and capillary leak syndrome (n = 1; Table 1). Renal parameters at diagnosis were similar in C3G patients with MIg and in C3G patients older than 50 years without MIg (supplemental Table 2).
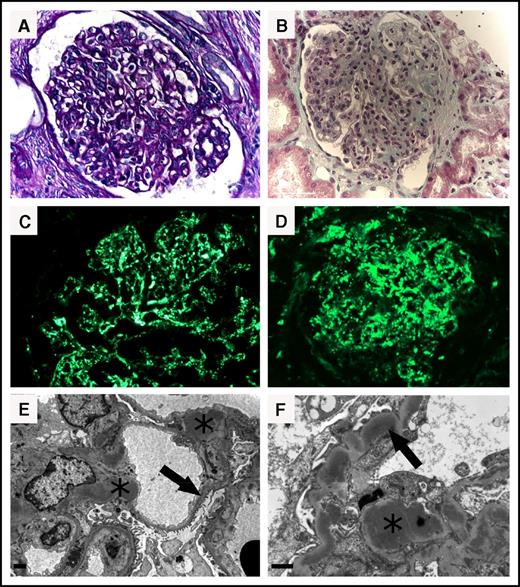
Pathological data
By light microscopy, 27 patients (54%) exhibited mesangial proliferative glomerulonephritis and 23 (46%) had a membranoproliferative pattern (Figure 2A-B). Glomerular crescents were found in 11 patients (22%), diffuse and cellular in 2 cases. Eight (16%) patients had thrombotic microangiopathy-like lesions, with occasional thrombi within glomerular capillaries, mesangiolysis, endothelial swelling and subendothelial lucent deposits. One patient with λ LC MM had concomitant cast nephropathy with numerous fractured polychromatophilic λ LC-positive casts in distal tubule lumens. By immunofluorescence, all patients displayed bright glomerular C3 deposits with prominent mesangial and subendothelial distribution (Figure 2C). Predominant subepithelial C3 deposits were observed in 14 patients (Figure 2D) (Table 1; supplemental Table 3).
Kidney biopsy findings of monoclonal gammopathy–associated C3 glomerulopathy. (A-B) Light microscopy. (A) Section of renal cortex showing mesangial proliferative glomerulonephritis (periodic acid–Schiff staining, ×400). (B) Diffuse membranoproliferative glomerulonephritis with nodular appearance of the mesangium and glomerular capillary wall deposits (light green trichrome, ×400). (C-D) Immunofluorescence microscopy. Diffuse granular capillary wall and mesangial bright deposits (anti-C3 fluorescein isothiocyanate-conjugate, ×400). (E-F) Electron microscopy. (E) Nodular (pseudohumps) electron-dense mesangial deposits (asterisk) and intramembranous dense deposits (arrow). Scale bar, 1 µm (original magnification ×8000). (F) Nodular electron-dense mesangial deposits (asterisk) and interrupted intramembranous dense deposits displaying a sausage-shaped (arrow). Scale bar, 1 µm (original magnification ×15 000).
Kidney biopsy findings of monoclonal gammopathy–associated C3 glomerulopathy. (A-B) Light microscopy. (A) Section of renal cortex showing mesangial proliferative glomerulonephritis (periodic acid–Schiff staining, ×400). (B) Diffuse membranoproliferative glomerulonephritis with nodular appearance of the mesangium and glomerular capillary wall deposits (light green trichrome, ×400). (C-D) Immunofluorescence microscopy. Diffuse granular capillary wall and mesangial bright deposits (anti-C3 fluorescein isothiocyanate-conjugate, ×400). (E-F) Electron microscopy. (E) Nodular (pseudohumps) electron-dense mesangial deposits (asterisk) and intramembranous dense deposits (arrow). Scale bar, 1 µm (original magnification ×8000). (F) Nodular electron-dense mesangial deposits (asterisk) and interrupted intramembranous dense deposits displaying a sausage-shaped (arrow). Scale bar, 1 µm (original magnification ×15 000).
Ultrastructural pattern was consistent with C3GN in 24/25 (96%) patients, with osmiophilic dense deposits located in mesangium (80%) and subendothelial space (76%). Humps were observed in 48% of patients (Figure 2E). Only 1 patient had DDD with typical dense “sausage-shaped” deposits within glomerular basement membranes and less abundant subendothelial osmiophilic deposits (Figure 2F).
Baseline hematological data
A serum monoclonal gammopathy (IgG, n = 47; IgA, n = 2; LC only, n = 1) was detected by immunofixation in all cases. LC isotype was κ in 37/50 patients. By electrophoresis, 47 patients had a detectable monoclonal spike, with a median level of 10 (2-38) g/L. Among 32 patients tested, 17 (53%) had an abnormal κ/λ ratio with median dFLC of 79 (2-20.800) mg/L. In 17 (34%) patients, monoclonal gammopathy had been diagnosed before renal disease, with a median interval of 44 (12-120) months. Bone marrow studies were performed on bone marrow smears (n = 45) or biopsy (n = 5). Seventeen patients (34%) had more than 10% infiltration by dystrophic and clonal plasma cells (as demonstrated by immunofluorescence or flow cytometry). Hematological diagnosis was MGRS (n = 30), smoldering MM (n = 15), symptomatic MM (n = 2), and CLL (n = 3). The prevalence of MM was significantly higher in patients treated with chemotherapy or immunosuppressive drugs compared with untreated patients (P = .03; Table 1).
Complement studies
Plasma C3 and sC5b-9 levels in MIg-C3G patients were compared with those of the 29 C3G patients older than 50 years without MIg (supplemental Table 2). Median C3 level was similar (P = .56), but median sC5b-9 level was significantly higher in patients with MIg-C3G (734 [164-2370] ng/mL vs 498 [215-1501] ng/mL, respectively; P = .03; supplemental Table 2).
Complement studies in patients with MIg-C3G are detailed in Table 1. Before initiation of hematological treatment, baseline complement C3 level was low in 22/50 (43%) patients, without any significant difference among patients treated with chemotherapy, immunosuppressive therapy, or conservative treatment (P = .7; Table 1). C4 level was normal in all patients. Twenty-seven of 34 tested patients had elevated sC5b-9 level without significant difference among the 3 groups of patients (P = .42; Table 1). C3NeF and anti-FH antibodies were found in 3 (6%) and 9 (19%) patients, respectively. Screening of variants in complement genes was performed in 28 patients. Two patients carried a rare variant of undetermined significance (p.D130N in CFH and p.E548Q in CFI).
Treatment
Thirteen patients were given conservative treatment alone with renin-angiotensin system blockers. Eight patients received various immunosuppressive drugs after a median of 4 (1-54) months from diagnosis. Immunosuppressive regimens consisted of steroids alone (n = 4), prednisone combined with rituximab (n = 1), mycophenolate mofetil (n = 1), azathioprine (n = 1), or cyclophosphamide (n = 1). Twenty-nine patients received chemotherapy targeting the associated B-cell clone after a median time from diagnosis of 3 (1-20) months. Chemotherapy was based on alkylating agents (cyclophosphamide, n = 2; melphalan, n = 3) with dexamethasone (DXM) in 5 patients, and on bortezomib in 22 patients (bortezomib-DXM: n = 10; bortezomib-cyclophosphamide-DXM, n = 10; bortezomib-thalidomide-DXM, n = 2). Two patients with CLL received rituximab-based therapy. Patients received a median of 6 (3-9) cycles as first-line treatment (Table 2).
Treatment modalities
| . | Treated patients (N = 37) . |
|---|---|
| Chemotherapy adapted to the clone, n (%) | 29 (78%) |
| Median time to treatment, mo | 3 (1-20) |
| Alkylating agent-dexamethasone* | 5 (17%) |
| Bortezomib based regimen-dexamethasone† | 22 (76%) |
| Prednisone-rituximab‡ | 2 (7%) |
| Immunosuppressive therapy, n | 8 (22%) |
| Median time to treatment, mo | 4 (1-54) |
| Prednisone-dexamethasone | 4 (50%) |
| Prednisone-cyclophosphamide | 1 (12.5%) |
| Prednisone-rituximab | 1 (12.5%) |
| Prednisone-mycophenolate mofetil | 1 (12.5%) |
| Prednisone-azathioprine | 1 (12.5%) |
| . | Treated patients (N = 37) . |
|---|---|
| Chemotherapy adapted to the clone, n (%) | 29 (78%) |
| Median time to treatment, mo | 3 (1-20) |
| Alkylating agent-dexamethasone* | 5 (17%) |
| Bortezomib based regimen-dexamethasone† | 22 (76%) |
| Prednisone-rituximab‡ | 2 (7%) |
| Immunosuppressive therapy, n | 8 (22%) |
| Median time to treatment, mo | 4 (1-54) |
| Prednisone-dexamethasone | 4 (50%) |
| Prednisone-cyclophosphamide | 1 (12.5%) |
| Prednisone-rituximab | 1 (12.5%) |
| Prednisone-mycophenolate mofetil | 1 (12.5%) |
| Prednisone-azathioprine | 1 (12.5%) |
*Cyclophosphamide-dexamethasone (n = 4), Melphalan-dexamethasone (n = 2).
Bortezomib-dexamethasone (n = 10), bortezomib-thalidomide-dexamethasone (n=2), bortezomib-cyclophosphamide-dexamethasone (n = 10).
For treatment of chronic lymphoid leukemia.
Tolerance to chemotherapy
Five of 29 patients who received chemotherapy experienced severe adverse events, including 6 episodes of infectious pneumonitis (bacterial, n = 4; aspergillosis, n = 1; H1N1 virus, n = 1), leading to death in 3 cases. One patient treated with bortezomib developed peripheral neuropathy that required treatment discontinuation.
Hematological and renal response
Hematological response and renal responses were available in 37 treated patients (chemotherapy or immunosuppressive therapy) and 48 patients, respectively (Table 3). After first-line therapy, 18 of 37 treated patients achieved hematological response (assessed on serum monoclonal protein level by electrophoresis in 17 cases and/or FLC criteria in 6 cases). In 1 patient with λ LC myeloma, hematological response was based on FLC criteria only. Of these patients, 15 (83%) had a renal response. In contrast, among 19 patients who did not achieve hematological response after treatment, 5/18 (28%) had a renal response (P = .002). By univariate analysis, predictive factors of renal response were proteinuria at onset of treatment (P = .005), use of chemotherapy (P = .001), use of bortezomib-based regimen (P = .0001), time to treatment initiation (P = .018), and hematological response (P = .0001; Table 4). By multivariate analysis, only hematological response was associated with renal response (odds ratio, 9; 95% confidence interval [CI], 7.98-10.02; P = .035).
Hematological and renal responses
| . | All patients (N = 50) . | Chemotherapy (N = 29) . | Others (IS/conservative) (N = 21) . | P value . |
|---|---|---|---|---|
| Hematological response, n (%) | 18/49 (37%) | 17/29 (59%) | 1 /20 (5%) | .0002* |
| Complete response | 9 (18%) | 8 (28%) | 1 (5%) | .06† |
| Very good partial response | 1 (2%) | 1 (3%) | 0 (0%) | 1‡ |
| Partial response | 8 (16%) | 8 (28%) | 0 (0%) | .01¶ |
| No response | 31 (63%) | 12 (41%) | 19 (95%) | .0002§ |
| NA | 1 (2%) | 1 (%5) | 1 | |
| Severe adverse events | 6 (12%) | 5 (21%) | 1 (5%) | .21 |
| Renal response, n (%) | 20/48 (42%) | 19/27 (74%) | 1/21 (5%) | .0001 |
| Complete response | 6 (13%) | 6 (22%) | 0 (0%) | .001 |
| Partial response | 14 (29%) | 13 (48%) | 1 (5%) | .002 |
| No response | 28 (58%) | 9 (32%) | 19 (90%) | .0001 |
| NA | 2 (4%) | 2 (6%) | 0 (0%) | — |
| Renal parameters after first-line therapy | ||||
| Serum creatinine, µmol/L | 179 (70-450) | 147 (70-450) | 231 (132-400) | .17 |
| eGFR, mL/min/1.73m2 | 34 (16-94) | 37 (16-94) | 24 (16-51) | .1 |
| 24-h Proteinuria, g | 2.4 (0.1-5) | 2.4 (0.1-3) | 2.6 (0.7-5) | .46 |
| ESRD, n (%) | 12 (24%) | 5 (17%) | 7 (33%) | .31 |
| Data at last follow-up | ||||
| Follow-up, mo | 24 (4-104) | 24 (8-104) | 25 (4-69) | .75 |
| Serum creatinine, µmol/L | 144 (68-290) | 135 (68-258) | 249 (135-290) | .2 |
| eGFR, ml/min/1.73 m2 | 38 (18-89) | 38 (18-89) | 21 (19-48) | .16 |
| 24-h proteinuria, g | 1.1 (0.08-6.5) | 0.86 (0.08-17) | 1.2 (0.4-7) | .59 |
| ESRD, n (%) | 25 (50%) | 9 (31%) | 16 (76%) | .003 |
| Renal transplantation, n (%) | 4 (8%) | 0 (0%) | 4 (13%) | — |
| C3G recurrence, n (%) | 4/4 (100%) | — | 4/4 (100%) | — |
| Death, n (%) | 5 (10%) | 3 (10%) | 2 (10%) | 1 |
| . | All patients (N = 50) . | Chemotherapy (N = 29) . | Others (IS/conservative) (N = 21) . | P value . |
|---|---|---|---|---|
| Hematological response, n (%) | 18/49 (37%) | 17/29 (59%) | 1 /20 (5%) | .0002* |
| Complete response | 9 (18%) | 8 (28%) | 1 (5%) | .06† |
| Very good partial response | 1 (2%) | 1 (3%) | 0 (0%) | 1‡ |
| Partial response | 8 (16%) | 8 (28%) | 0 (0%) | .01¶ |
| No response | 31 (63%) | 12 (41%) | 19 (95%) | .0002§ |
| NA | 1 (2%) | 1 (%5) | 1 | |
| Severe adverse events | 6 (12%) | 5 (21%) | 1 (5%) | .21 |
| Renal response, n (%) | 20/48 (42%) | 19/27 (74%) | 1/21 (5%) | .0001 |
| Complete response | 6 (13%) | 6 (22%) | 0 (0%) | .001 |
| Partial response | 14 (29%) | 13 (48%) | 1 (5%) | .002 |
| No response | 28 (58%) | 9 (32%) | 19 (90%) | .0001 |
| NA | 2 (4%) | 2 (6%) | 0 (0%) | — |
| Renal parameters after first-line therapy | ||||
| Serum creatinine, µmol/L | 179 (70-450) | 147 (70-450) | 231 (132-400) | .17 |
| eGFR, mL/min/1.73m2 | 34 (16-94) | 37 (16-94) | 24 (16-51) | .1 |
| 24-h Proteinuria, g | 2.4 (0.1-5) | 2.4 (0.1-3) | 2.6 (0.7-5) | .46 |
| ESRD, n (%) | 12 (24%) | 5 (17%) | 7 (33%) | .31 |
| Data at last follow-up | ||||
| Follow-up, mo | 24 (4-104) | 24 (8-104) | 25 (4-69) | .75 |
| Serum creatinine, µmol/L | 144 (68-290) | 135 (68-258) | 249 (135-290) | .2 |
| eGFR, ml/min/1.73 m2 | 38 (18-89) | 38 (18-89) | 21 (19-48) | .16 |
| 24-h proteinuria, g | 1.1 (0.08-6.5) | 0.86 (0.08-17) | 1.2 (0.4-7) | .59 |
| ESRD, n (%) | 25 (50%) | 9 (31%) | 16 (76%) | .003 |
| Renal transplantation, n (%) | 4 (8%) | 0 (0%) | 4 (13%) | — |
| C3G recurrence, n (%) | 4/4 (100%) | — | 4/4 (100%) | — |
| Death, n (%) | 5 (10%) | 3 (10%) | 2 (10%) | 1 |
Specific comparison between the group chemotherapy and IS therapy: *P = .08; †P = .65; ‡P = 1; ¶P = .3; and §P = .08.
g, gramme; NA, not available.
Characteristics of renal responders
| . | Renal responders (n = 20) . | Nonrenal responders (n = 28) . | P value . |
|---|---|---|---|
| Age, y | 62 (38-83) | 67 (40-80) | .16 |
| Baseline eGFR, mL/min/1.73 m2 | 54 (3-94) | 34 (6-100) | .1 |
| CKD 1-2 at diagnosis, n (%) | 10/20 (50%) | 3/28 (11%) | .003 |
| 24h-proteinuria at onset, g | 4.4 (0.9-12.8) | 2.5 (0.4-5.9) | .005 |
| M-spike g/L | 8 (2-38) | 11 (4-30) | .54 |
| Normal C3 level, n (%) | 11 (52%) | 19 (68%) | .33 |
| MGRS, n (%) | 9 (45%) | 20 (71%) | .12 |
| Specific chemotherapy, n (%) | 19 (95%) | 8 (29%) | .001 |
| Bortezomib -based regimen, n (%) | 17 (85%) | 5 (18%) | .0001 |
| Time from diagnosis to treatment, mo | 3.5 (1-19) | 14 (1-48) | .018 |
| Hematological response, n (%) | 15 (75%) | 2/26 (8%) | .0001 |
| . | Renal responders (n = 20) . | Nonrenal responders (n = 28) . | P value . |
|---|---|---|---|
| Age, y | 62 (38-83) | 67 (40-80) | .16 |
| Baseline eGFR, mL/min/1.73 m2 | 54 (3-94) | 34 (6-100) | .1 |
| CKD 1-2 at diagnosis, n (%) | 10/20 (50%) | 3/28 (11%) | .003 |
| 24h-proteinuria at onset, g | 4.4 (0.9-12.8) | 2.5 (0.4-5.9) | .005 |
| M-spike g/L | 8 (2-38) | 11 (4-30) | .54 |
| Normal C3 level, n (%) | 11 (52%) | 19 (68%) | .33 |
| MGRS, n (%) | 9 (45%) | 20 (71%) | .12 |
| Specific chemotherapy, n (%) | 19 (95%) | 8 (29%) | .001 |
| Bortezomib -based regimen, n (%) | 17 (85%) | 5 (18%) | .0001 |
| Time from diagnosis to treatment, mo | 3.5 (1-19) | 14 (1-48) | .018 |
| Hematological response, n (%) | 15 (75%) | 2/26 (8%) | .0001 |
M-spike, monoclonal spike.
Patient and renal survival
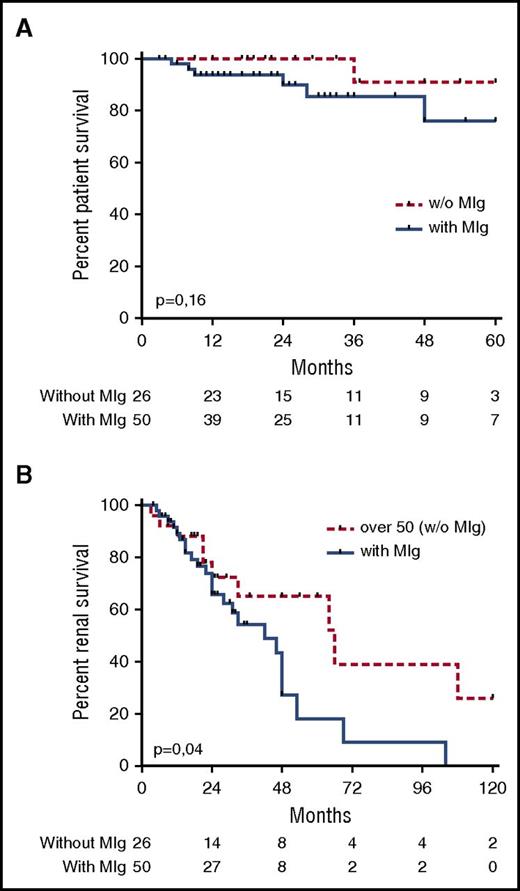
At last follow-up, 5 patients had died. Causes of death were cardiac (n = 1), neurological (n = 1), and infectious complications after chemotherapy (n = 3). Overall survival of patients with MIg-associated C3G was not significantly different from that of patients older than 50 years without MIg (P = .16; Figure 3A). One patient treated with corticosteroids alone developed hepatocellular carcinoma 3 years after diagnosis.
Renal and patient survival. (A) Kaplan-Meier patient survival analysis comparing C3G patients with or without MIg older than 50 years. (B) Kaplan-Meier renal survival analysis comparing patients with MIg-C3G and patients with C3G without MIg older than 50 years.
Renal and patient survival. (A) Kaplan-Meier patient survival analysis comparing C3G patients with or without MIg older than 50 years. (B) Kaplan-Meier renal survival analysis comparing patients with MIg-C3G and patients with C3G without MIg older than 50 years.
The median renal survival of MIg-C3G patients was significantly lower compared with that of C3G patients older than 50 years without monoclonal gammopathy (P < .003; hazard ratio [HR], 2.915; 95% CI, 1.41-6.01; Figure 3B). Among C3G patients under conservative treatment alone, median renal survival was also significantly higher in those without MIg (P = .02; supplemental Figure 1). After a median follow-up of 24 (4-104) months, 25 patients (50%) with MIg C3G had reached ESRD.
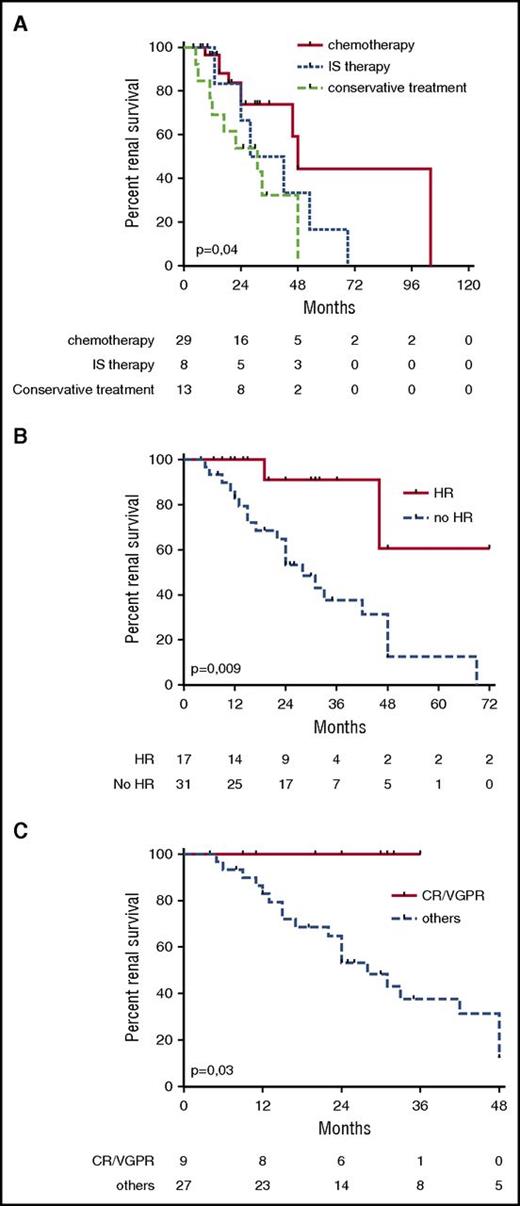
Median renal survival was higher in patients who had received chemotherapy compared with in those given conservative treatment (48 vs 31 months, respectively; P = .01; HR, 0.27; 95% CI, 0.09-0.77), but was not significantly different from that of patients receiving immunosuppressive therapy (28 months; P = .18; HR, 0.41; 95% CI, 0.11-1.51; Figure 4A). Median renal survival in patients who received chemotherapy was similar to that in C3G patients older than 50 years without MIg (data not shown). Renal survival was higher in patients who achieved a hematological response compared with those who did not (P = .009; HR, 0.17; 95% CI, 0.12-0.66; Figure 4B). Moreover, renal survival was higher in patients who reached complete hematological response or very good partial response compared with in patients who did not respond or achieved PR only (P = .05; Figure 4C). In patients who received chemotherapy, renal survival was significantly higher in patients with hematological response compared with in nonresponders (P = .04; supplemental Figure 3).
Renal survival. (A) Kaplan-Meier renal survival analysis comparing MIg-C3G patients who received chemotherapy, immunosuppressive therapy, or conservative therapy. (B) Kaplan-Meier renal survival analysis comparing MIg-C3G patients who achieved or did not achieve hematological response. (C) Kaplan-Meier renal survival analysis comparing MIg-C3G patients with or without hematological response (complete response or very good partial response) in 37 patients who received treatment (immunosuppressive therapy or chemotherapy). Data regarding the hematological response were available in 36 of the 37 patients. CR, complete hematological response; HR, hematological response; IS, immunosuppressive; VGPR, very good partial response.
Renal survival. (A) Kaplan-Meier renal survival analysis comparing MIg-C3G patients who received chemotherapy, immunosuppressive therapy, or conservative therapy. (B) Kaplan-Meier renal survival analysis comparing MIg-C3G patients who achieved or did not achieve hematological response. (C) Kaplan-Meier renal survival analysis comparing MIg-C3G patients with or without hematological response (complete response or very good partial response) in 37 patients who received treatment (immunosuppressive therapy or chemotherapy). Data regarding the hematological response were available in 36 of the 37 patients. CR, complete hematological response; HR, hematological response; IS, immunosuppressive; VGPR, very good partial response.
We performed Cox proportional hazards model analysis regarding progression to ESRD. By univariate analysis, renal response, hematological response and hematological treatment were predictive of renal survival (P = .048, P = .028, and P = .022, respectively; supplemental Figure 4). In 2 different models, by multivariate analysis, only the absence of renal response was independently associated with ESRD (P = .0006 and P = .008, respectively; supplemental Table 4).
Four patients, including 3 patients in the conservative treatment group and 1 treated with rituximab-prednisone, received a renal allograft. At the time of transplantation, none had achieved hematological response, and all showed disease recurrence after 3 to 12 months that resulted in graft loss in 1 case.
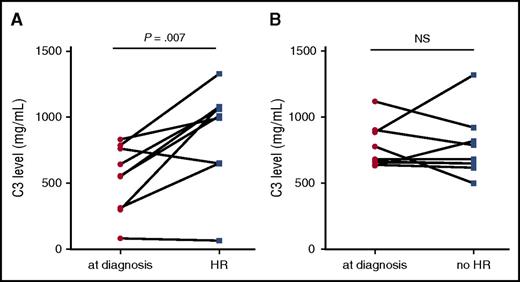
Complement assays after treatment
Posttreatment complement studies were available in 18 patients, including 9 patients with HR after chemotherapy. Plasma C3 level normalized in 6 patients, 5 of whom had achieved HR. C3 level in the 9 patients with HR was significantly higher after treatment compared with pretreatment C3 level (P = .007; Figure 5A). In contrast, C3 levels in 9 patients who did not achieve HR were unchanged after treatment (Figure 5B).
C3 level before and after treatment. (A) In 9 patients who reached hematological response. (B) In 9 patients without evidence of hematological response.
C3 level before and after treatment. (A) In 9 patients who reached hematological response. (B) In 9 patients without evidence of hematological response.
Discussion
In this study, we analyzed the effect of chemotherapy targeting the underlying B-cell clone in a large cohort of patients with MIg-C3G. We showed that efficient chemotherapy resulted in higher renal response rate and longer renal survival than conservative or immunosuppressive therapy.
C3G is a rare glomerular disease associated with dysregulation of the complement AP. The severity is variable, with one third of patients initially presenting with nephrotic range proteinuria and/or renal impairment.7 Renal prognosis of C3G remains poor, as 40% of patients progress to ESRD 8 to 10 years after diagnosis,7 and treatment is ill defined. In addition to nonspecific nephroprotective drugs such as renin-angiotensin system blockers, several observations suggest some efficacy of immunosuppressive therapies, including eculizumab, a monoclonal anti-C5 antibody targeting the final step of complement pathway, and agents targeting T and/or B cells with a potential effect on glomerular inflammation and production of auto-antibodies activating complement AP.24-27 In a recent study, it has been suggested that mycophenolate mofetil may improve renal survival in C3G.28
C3G associated with monoclonal gammopathy remains poorly described. The high prevalence of monoclonal gammopathy in C3G patients older than 50 years, reaching 30% to 71% in 2 small series and 65% in the French C3G national cohort, strongly suggests a pathogenic link between the 2 conditions, even in the absence of MIg deposits on glomeruli.11,13 In the series from Zand et al, 56% of patients presented with nephrotic syndrome and 81% with renal failure at diagnosis.13 In our study, 43% of patients had nephrotic syndrome and 84% showed significant renal impairment at diagnosis. Of note, severe extra renal manifestations characterized by skin necrotic lesions were present in 3 patients, none of whom had evidence of cryoglobulinemia, despite repeated tests. Although drüsen and lipodystrophy may occur in patients with C3G, distal ischemic symptoms have not been described outside the context of monoclonal gammopathy.9 Whether overactivation of complement AP may be involved in severe skin involvement in MIg-C3G remains to be determined. MIg-C3G appears to be associated with shorter renal survival compared with C3G in patients older than 50 years without MIg. Moreover, in our study, median renal survival was 31 months in patients receiving immunosuppressive therapy, similar to that observed in patients receiving conservative therapy. This result suggests that targeting intraglomerular inflammation is not sufficient to improve renal prognosis in MIg-C3G. Renal response rate and renal survival were significantly higher in patients who rapidly achieved complete hematological response or very good partial response with chemotherapy, suggesting a pathogenic role for MIg in glomerular C3 deposition.
In our study, 90% of patients had an indolent clonal disorder, consistent with MGRS. As in other types of renal diseases in MGRS, it is likely that physicochemical peculiarities of MIg, rather than tumor mass, govern nephrotoxicity. The International Kidney and Monoclonal Gammopathy Research Group proposed to adapt treatment strategy to both the origin (plasmacytic or lymphocytic) of the causal clone and the severity of renal disease.2 On the basis of these recommendations, 29 patients received chemotherapy, including bortezomib-based regimens in 22 patients. Our results suggest that the use of novel antimyeloma agents, such as bortezomib, represent a valuable therapeutic option in MIg-C3G. Because 5 patients treated with chemotherapy had severe adverse events, leading to death in 3 cases, therapeutic choices should take into account renal elimination of antineoplastic drugs to limit their adverse effects. The absence or insufficient suppression of the underlying clonal disorder resulted in early C3G recurrence after transplantation in 4 patients. Achieving sustained hematological remission before transplantation should be considered to limit recurrence and to avoid the use of chemotherapy in immunosuppressed patients.
Despite being the largest series to report renal outcomes after chemotherapy, this study has several limitations. It was a retrospective multicenter study, including different treatment regimens. Moreover, it only provides indirect arguments in favor of a pathophysiological link among MIg, AP dysregulation, and renal lesions. AP abnormalities identified in C3G patients are acquired in most cases. Indeed, C3NeF, an autoantibody that stabilizes the AP C3 convertase, or anti-FH antibodies are identified in more than 50% of patients.7-9,29 In our study, C3NeF and anti-FH antibodies were detected in only 6% and 19% of patients, respectively. In 1999, it was demonstrated that a circulating monoclonal λ LC, identified in a patient with MPGN, was able to activate the AP in vitro in a manner different from C3NeF. Indeed, this dimeric LC behaved as a mini autoantibody against FH, leading to uncontrolled AP activation and C3 glomerular deposition.30 As the anti-FH antibodies were not isotype-restricted to the monoclonal LC identified in our patients in most cases (data not shown), they were likely to be distinct from the circulating MIg. The main biomarker associated with C3G is plasma C3 level, which is decreased in 50% to 80% of patients.7 Elevated soluble C5b-9 has recently been described as a new biomarker of C5 convertase activity, mainly associated with C3GN pattern.31 In MIg-C3G, 40% of patients had low C3 level. Interestingly, hematological response was associated with a significant increase in C3 level, suggesting C3 level may serve as biomarker of treatment efficacy. This finding is of particular interest for the evaluation of response to treatment in patients with normal FLC ratio and a small monoclonal spike on serum electrophoresis. Elevated soluble C5b-9 was found in 80% of tested MIg-C3GN patients, with significantly higher levels compared with C3G patients without monoclonal gammopathy. AP dysregulation is associated with another rare renal disease, atypical hemolytic uremic syndrome, characterized by thrombotic microangiopathy. In our series, 16% of patients had lesions of thrombotic microangiopathy likely to result from local AP activation. Eculizumab is currently recommended for the treatment of atypical hemolytic uremic syndrome. Whether its use, combined with chemotherapy, might be beneficial in MIg-C3G patients, particularly those with concomitant renal thrombotic microangiopathy, remains to be evaluated.
In conclusion, to the best of our knowledge, this study is the first to report epidemiological data and renal outcomes after chemotherapy in patients with MIg-C3G. On the basis of our results, we recommend careful hematological workup in patients older than 50 years with a diagnosis of C3G. Our results indicate that achievement of clonal response may favorably influence renal outcomes. Chemotherapy adapted to the origin of the underlying B-cell clonal disorder and to renal function should be considered early in the disease course. The efficacy and tolerance of chemotherapy regimens, such as bortezomib combinations, remains to be established in patients with C3G and monoclonal gammopathy. Finally, experimental studies are required to unravel the link between monoclonal Ig and AP dysregulation in C3G.
Portions of this work were presented at the 15th Réunion Commune de la Société de Néphrologie et de La Société Francophone de Dialyse, Nantes, France, 8-11 October 2013.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors acknowledge M. Mignotet for technical support and all colleagues who participated in this study: R. Boudet (Department of Nephrology, Brives), P. Daugas (Department of Nephrology, Bichat, AP-HP), F. Fakhouri (Department of Nephrology, Nantes), F. Gallen Labbe (Department of Nephrology, Valence), P. Gobert (Department of Nephrology, Avignon), M. Hazzan (Department of Nephrology, Lille), L. Mercadal (Department of Nephrology, Pitié Salpétrière, AP-HP), M. Nouvier (Department of Nephrology, Lyon), N. Martin Silva (Department of Medicine, Caen), F. Merabet (Department of Hematology, Versailles), E. Renaudineau (Department of Nephrology, Saint Malo), J. B. Philit (Department of Nephrology, Chambery), D. Sarret (Department of Nephrology, Val de Grâce, Paris), A. Servais (Department of Nephrology, Necker, AP-HP), L. Taghipour (Department of Nephrology, Armentières), A. Tiple (Department of Nephrology, Clermont-Ferrand).
This work was supported by grants from the Délégation Régionale à la Recherche Clinique, AP-HP (V.F.-B.), such as Programme Hospitalier de Recherche Clinique (AOM08198), by grants from the Fondation Pour La Recherche Medicale (FDM 20130727355) and the Association pour l’Information et la Recherche dans les maladies Rénales génétiques, by grants from European Community (FP7 Grant 2012-305608 EURenOmics), and by the Fondation du Rein (FRM, prix, 2012 Fondation pour la Recherche Médicale to V.F.-B.).
Authorship
Contribution: The study was conceived and designed by S.C., V.F.-B., and F.B.; S.C. conducted the analysis; V.F.-B., and F.B. reviewed the data analysis; S.C., V.F.-B., and F.B. were involved in the writing of the manuscript; and all other authors contributed to the conduct of the trial, recruited patients, and were involved in the review of results and final approval of the manuscript.
Conflict-of-interest disclosure: V.F.-B. received fees for participation in advisory boards, experts meetings, and/or teaching courses from Alexion Pharmaceutical. The remaining authors declare no competing financial interests.
Correspondence: Sophie Chauvet, Department of Nephrology, European Hospital Georges Pompidou, AP-HP, 20 Rue Leblanc, 75908 Paris Cedex 15, France; e-mail: sophie.chauvet@aphp.fr.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal