Abstract
T-cell immune reconstitution (IR) after allogeneic hematopoietic cell transplantation (allo-HCT) is highly variable between patients and may take several months to even years. Patients with delayed or unbalanced T-cell IR have a higher probability of developing transplantation-related morbidity, mortality, and relapse of disease. Hence, there is a need for strategies to better predict and improve IR to reduce these limitations of allo-HCT. In this review, we provide an update of current and in-near-future clinically relevant strategies before, during, and after transplantation to achieve successful T-cell IR. Potent strategies are choosing the right HCT source (eg, donor-recipient matching, cell dose, graft manipulation), individualized conditioning and serotherapy (eg, antithymocyte globulin), nutritional status, exercise, home care, modulation of microbiota, enhancing homeostatic peripheral expansion, promoting thymopoiesis, and the use of adjuvant-targeted cellular immunotherapies. Strategies to prevent graft-versus-host disease are important as well because this complication and the subsequent need for immunosuppression affects T-cell IR and function. These options aim for personalized precision transplantation, where allo-HCT therapy is designed to boost a well-balanced T-cell IR and limit complications in individual patients, resulting in overall lower morbidity and higher survival chances.
Introduction
Allogeneic hematopoietic cell transplantation (allo-HCT) nowadays is a widely accepted potentially curative treatment strategy for patients with refractory hematological malignancies and a variety of benign disorders. Immune reconstitution (IR) after allo-HCT, especially of the adaptive immune system, is highly variable between patients and can take several months to even years. A timely and balanced T-cell IR is especially important for sustained graft-versus-leukemia (GVL) effects, protection against opportunistic infections, and survival chances after allo-HCT.1-3
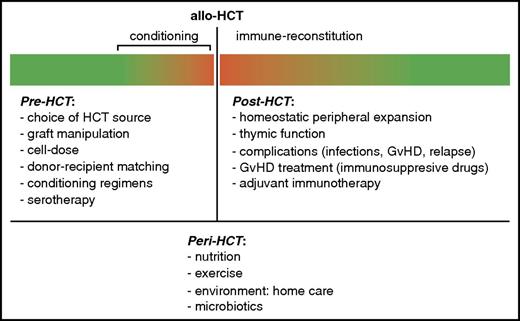
Hence, there is a clear need to develop strategies to better predict and enhance T-cell recovery and function. The choice of the transplantation unit (eg, cell source, cell dose, donor-recipient matching, graft manipulation) and conditioning regimens are important variables pre-HCT that influence T-cell IR and subsequent complications (Figure 1). Also, peritransplantation parameters, such as the nutritional status of the patient and the composition of the gut microbiome, may influence outcome. Posttransplantation, T-cell reconstitution is dependent on 2 mechanisms: homeostatic peripheral expansion (HPE) and thymopoiesis. Therefore, T-cell IR would improve with strategies that stimulate HPE and thymic function. Graft-versus-host disease (GVHD) also is a major factor affecting T-cell IR,4 in part due to the immunosuppression needed to treat this complication after allo-HCT. As the thymus is especially sensitive to damage, such as during GVHD, even minor-grade GVHD might affect thymopoiesis.4-6 Therefore, strategies to prevent GVHD might improve T-cell IR as well.
Pre-, peri-, and post-HCT factors affecting T-cell IR. Depicted in the bars are relative immune cell levels. Red, <reference values; risk for complications. Green, ≥reference values; adequate immunity.
Pre-, peri-, and post-HCT factors affecting T-cell IR. Depicted in the bars are relative immune cell levels. Red, <reference values; risk for complications. Green, ≥reference values; adequate immunity.
In this review, we comprehensively discuss current and in near-future clinically relevant strategies to better predict and improve T-cell IR and function after allo-HCT.
Pretransplantation strategies
Choice of HCT source
Transplantation with bone marrow (BM) or peripheral blood (PB) (stem) cells from a matched family donor is considered the standard for allo-HCT. Alternative choices are BM/PB from a volunteer unrelated matched or mismatched donor, a haploidentical or mismatched family donor, and unrelated cord blood (CB). In addition, in an attempt to lower the risk of GVHD, the physician may choose for different strategies: CD34+ selection, ex vivo T-cell depletion (TCD) using negative selection with CD3+ or CD3αβ+ beads, in vivo TCD using serotherapy (T-cell–binding antibodies) such as antithymocyte globulin (ATG) or alemtuzumab, or for posttransplant cyclophosphamide (in haploidentical setting). The choice of the HCT source and its manipulation are important factors in the probability of T-cell IR, and therefore different HCT sources are associated with different probabilities for various outcomes; for example, probability on GVHD (acute and chronic), relapse,7 and immune recovery. Use of BM/PB grafts from younger donors is shown to improve survival chances,8,9 which may be due to enhanced immune-recovery probability. Overall, all HCT sources have advantages and disadvantages, and no clear superior cell source exists. The donor choice highly depends on institutional practices: some centers are more confident with CB, whereas others prefer BM/PB from matched unrelated donors, or haploidentical transplants.
HLA matching.
The availability of a donor is largely based on matching HLAs between patient and donor. For BM/PB, donor and recipient are typically matched on high resolution for HLA-A, HLA-B, HLA-C, HLA-DRB1, and some centers also match for HLA-DQB1 and HLA-DP. For CB transplantation (CBT), most centers use less stringent HLA-matching criteria: HLA-A, HLA-B (on low resolution), and HLA-DRB1 (on high resolution). This mismatching in CBT is permissive without increasing the probability on GVHD (in particular chronic).10 For BM/PB, mismatching at 1 or more HLA loci (on high resolution) increases the incidence of transplant-related mortality, resulting in lower survival chances. A mismatch of donor-specific antibodies may influence engraftment as well.11 Interestingly, in CBT, a certain degree of mismatching is suggested to be associated with increased GVL whereas GVHD probability is not increased.12,13 Importantly, to influence the probability of finding a (better matched) donor, the following are needed: recruitment of minority BM/PB donors, donor retention, improved efficiency of searches, and, for CB donor selection, a larger global inventory of diverse units in public banks.
Cell dose.
To permit any chance of T-cell recovery, myeloid engraftment needs to occur first. For this, the graft needs to contain a sufficient amount of (nucleated/CD34+) cells as a low cell dose hampers engraftment.14,15 CB units generally contain lower cell numbers than do BM/PB, which may be a problem for transplanting adults or larger children. Therefore, CB units are selected on cell dose, which is disease (malignant/nonmalignant) and HLA-matching dependent. Furthermore, recently, strategies to identify the better cryopreserved CB units have been developed as well, such as selection based on the total colony-forming unit16 or the amount of Aldehyde-dehydrogenase-Bright cells.17 These quality checks suggest better prediction of neutrophil engraftment, and may subsequently enhance the T-cell IR potential after CBT. For BM/PB, cell dose from HCT in adults is usually sufficient (although a minimum number is still required15 ) because an adequate amount of cells can readily be harvested from the donor (BM/apheresis).
For CB grafts that do not contain enough cells for transplantation, ex vivo expansion strategies are available: Delta1 Notch ligand,18 coculture with mesenchymal cells (eg, Mesoblast),19 aryl hydrocarbon receptor antagonist StemRegenin 1 (SR1; eg, HSC835),20 nicotinamide (eg, NiCord),21 and the copper chelator tetraethylenepentamine (TEPA; eg, StemEx).22 These expansion methods were successfully used in various clinical phase 1/2 studies and shown to be safe and effective. Overall, over 95% neutrophil engraftment was noted after a median time of 10 to 15 days. Another approach to overcome low cell dose is the transplantation of 2 CBT units, double CBT. In this, both CB units contribute to engraftment and reconstitution, but only 1 provides durable neutrophil engraftment.23,24 Neutrophil engraftment after double CBT (of usually inadequately dosed units for single-unit CBT) is successful and shows 85% to 100% engraftment at a median time of 24 days, which is comparable to single CBT with sufficient cell dose. Some reports suggested that double CBT is associated with lower relapse probability25 compared with single CBT. However, randomized controlled trials failed to prove this effect on relapse,26,27 and higher GVHD rates are shown after double CBT.28 Coinfusion with CD34+ cells from a haploidentical donor (haplo-cord) can also overcome the lower cell dose for CBT. Compared with double CBT, haplo-cord showed faster neutrophil recovery, lower risk of GVHD, but slower T-cell IR, and is suggested to be associated with lower relapse risk.29 Randomized controlled studies are, however, lacking.
Immune reconstitution.
Differences in IR rates between cell sources and manipulations might also influence the choice of HCT source. In adults, T-cell IR generally is considered most rapid after HCT with PB compared with BM, without ex vivo TCD.30,31 Not surprisingly, T-cell IR is more rapid after PB/BM from a HLA-matched donor compared with haploidentical BM/PB conditioned with ATG.32 Nevertheless, the effect of the nowadays-popular option of post-haplo cyclophosphamide on T-cell IR remains to be investigated. After ex vivo TCD with serotherapy, T-cell IR is similar in recipients of PB or BM.33 Obviously, T-cell reconstitution is severely hampered after HCT with CD34-selected PB/BM.34,35 T-cell IR is prolonged in adult recipients of ex vivo TCD-unrelated BM, compared with pediatric recipients of unrelated BM transplantation (BMT) and adults receiving related BMT.36 In children, data on PB are scarce as BM and CB are most frequently used as graft sources. Without serotherapy, overall T-cell IR is comparable after BMT or CBT in children, although CD8+ T-cell reconstitution is faster after BMT, whereas regulatory T cells (Tregs) and CD4+ T-cell recovery are faster after CBT.37 The use of ATG (aiming for in vivo T-cell depletion) appears to be critical and cell source dependent; T-cell IR after CBT with ATG especially is severely hampered compared with BMT.38
Improving donor-recipient matching
PIRCHE.
Recently, an additional donor-recipient matching strategy was presented based on the probability of indirect HLA-molecule recognition represented by the number of predicted indirectly recognizable HLA epitopes (PIRCHEs).39 The number of PIRCHEs presented on HLA class I and II (PIRCHE-I and -II, respectively) is highly correlated with alloreactivity. For BM/PB donors with low PIRCHE-I and -II, the outcomes were similar to 10 of 10 HLA matching, whereas in CB a high PIRCHE-I is related to higher GVL.40
HLA-KIR matching.
Natural killer (NK) cells are one of the first cells that reconstitute after allo-HCT, making them important for immunity when T-cell counts are still low. NK-cell function is regulated by the balance of activating and inhibitory signals via killer immunoglobulin-like receptors (KIRs), which interact with specific HLA class I ligands. This may have implications for GVL; when inhibitory KIRs are mismatched for HLA type (mainly HLA-C), donor NK cells recognize and kill recipient leukemia cells.41-43 However, KIR mismatching can also lead to GVHD-like syndromes.44 Future prospective trials should assess the effect of HLA-KIR matching on the balance between unwanted effects from mismatching (eg, graft failure and GVHD) and its wanted effects (eg, GVL).
Conditioning prior to HCT
Chemotherapeutics and total body irradiation.
Conditioning prior to HCT includes chemotherapy, such as cyclophosphamide, fludarabine, and busulfan, and/or total body irradiation. In addition, serotherapy, such as ATG or alemtuzumab, is added to reduce the risk of graft rejection and GVHD. Both chemotherapeutics and irradiation may severely affect T-cell IR after HCT,45 mainly due to thymic damage.46 Notably, T-cell IR is delayed with myeloablative conditioning compared with nonmyeloablative conditioning without serotherapy.47 Therefore, T-cell IR could be enhanced by optimizing the dosage of these chemotherapeutics via pharmacokinetic and dynamic modeling, and thymic shielding during irradiation, aiming for minimal thymic damage. Furthermore, some chemotherapy with longer half-life (eg, fludarabine) may still be present during the infusion of the cells and can subsequently deplete T cells in vivo. Also, sex steroid hormone ablation may be applied to prevent thymic damage by chemotherapy/irradiation (described in the paragraph on posttransplantation interventions).
Individualized serotherapy to improve T-cell IR.
ATG was introduced to the conditioning regimen for in vivo TCD to reduce GVHD risk which can reach a cumulative incidence of over 40% to 70% even with a well-matched unrelated donor. A major drawback of conditioning with serotherapy is hampered early T- and B-cell recovery.48,49 This effect is partly through direct binding and killing of T and B cells, and also through “off-target” cytotoxic effects on thymus cells, affecting thymopoiesis.50 However, abandoning ATG from the conditioning is associated with significantly higher incidences of graft rejection and GVHD.51
Recently, high ATG exposure after allo-HCT was associated with detrimental effects on IR.38 The highly variable pharmacokinetics of ATG between patients causes underexposure or overexposure in a significant number of patients.52 CB cells were affected more by ATG compared with BM/PB; the tolerated post-HCT ATG exposure, which does not affect IR, is lower for CBT (<20 active units [AU] × day/mL) compared with BMT/peripheral blood cell transplantation (<50 AU × day/mL).38 CBT without ATG and CBT with very low ATG exposure were associated with excellent IR potential,49,51 stressing the importance for individualization. Interestingly, these studies also suggest that ATG exposure before, but not after, transplantation prevented GVHD (acute and chronic) not only in children, but also in adults (Rick Admiraal, Jurgen Kuball, and J.J.B., unpublished data). Sufficiently high exposure before CBT also prevented rejection. This indicates that there still is an important role for ATG, at least for HCT in nonmalignant diseases for graft rejection prevention, but earlier in the conditioning. In adult BM/PB recipients, this positive effect from conditioning with ATG on lower GVHD risk, but negative effects on T-cell IR, was also found.48,53 In HCT for hematopoietic malignancies, the decreased T-cell IR from posttransplantation ATG should especially be avoided, as this increases relapse risk and decreases survival.54,55 Taken together, these data suggest that personalized ATG dosing impacts T-cell IR potential after HCT, resulting in better survival chances.
Peritransplantation factors
Nutrition and microbiotics
Despite careful assessment and food supplementation, nutritional deficiency is common in allo-HCT patients. Nutritional requirements increase (up to 130%-150% of normal) due to catabolic stress, such as during IR and complications.56-58 Post-HCT calorie intake is directly related to time of neutrophil engraftment,56 and calorie requirements increase to ≥35 kcal/kg per day in addition to 1.5 to 2 g/kg per day of protein in the setting of GVHD.57
To maintain nutritional status during and after allo-HCT treatment, patients often receive enteral nutrition or total parenteral nutrition (TPN).59 Recently, enteral nutrition in the form of an oral elemental diet was shown to be superior to TPN in decreasing the duration and severity of mucositis and duration of hospitalization.60 Even during intestinal GVHD, outcome (eg, diarrhea and time to complete dietary recovery) after enteral nutrition was comparable to TPN.61 TPN, compared with enteral nutrition, resulted in significantly higher morbidity and mortality.58 Therefore, recent studies suggest that enteral nutrition, seems to be the best approach to maintain nutritional status after allo-HCT, even in patients with mucositis or intestinal GVHD.
The composition of nutrients is important for IR after allo-HCT; a lack of zinc, selenium, iron, and antioxidant vitamins can lead to clinically significant immune deficiency and infections.62,63 On the other hand, immune-modifying nutrients like vitamin D could be used to dampen GVHD,64 as it increases Treg numbers.65 Notably, vitamin D supplementation is only beneficial in decreasing GVHD risk for patients with the low active AA or Aa vitamin D receptor (VDR) phenotype.66 Vitamin D increases the risk for GVHD in patients with the active aa VDR phenotype. This poses opportunities to improve allo-HCT outcome using vitamin D supplementation, at least in patients with low VDR activity, which is currently evaluated in prospective trials.
Recent studies investigating the relation between intestinal microbiotics and GVHD in the human HCT setting found that a lower diversity of microbiota relates to a higher risk of GVHD and mortality.67,68 Specifically, a shift toward higher presence of Enterococcus faecium and Enterococcus faecalis was found in GVHD patients,69 whereas genus Blautia bacteria was associated with a lower probability of GVHD.70 Therefore, choosing the right antibiotic regime may be of importance for its effects on microbiome diversity and GVHD probability.71 As prebiotics and probiotics maintain and restore microbiotic diversity, the use of probiotics to reduce GVHD risk is currently under investigation. The first results indicate that probiotic treatment prior to and after allo-HCT is safe,72 and might even reduce GVHD severity associated with better T-cell IR.67
Exercise and home care
Daily exercise before and after HCT may fasten T-cell IR,73 although not all studies found a significant effect.74 Nevertheless, there is evidence indicating beneficial effects of physical exercise in the distribution and function of immune cells in healthy subjects.75 Prospective trials are warranted to prove this.
Some advantageous effects of home care in the neutropenic phase of the treatment are reported. Home care correlated with lower acute GVHD (aGVHD) incidence, and survival was at least as high as historic controls.76,77 Because home care would improve quality of life, reduce costs, and has been shown to be safe, further research on outcome and the effect on IR would be of interest.
Posttransplantation interventions
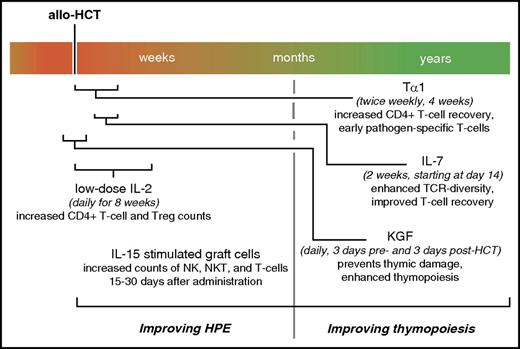
For T-cell recovery, homeostatic peripheral expansion is the most important mechanism in absence of thymopoiesis, which takes at least 6 to 12 months. Improving HPE will, therefore, ultimately improve early T-cell IR. Some cytokine-based therapies for improving IR through HPE are currently under investigation (Figure 2). Nevertheless, early T-cell immunity through HPE is limited due to a limited T-cell receptor (TCR) diversity, as thymopoiesis is needed to provide new TCR clones in naive T cells. Treatment of patients before receiving allo-HCT (eg, conditioning, steroids, chemotherapy) causes damage to the thymus. GVHD after HCT can also significantly damage the thymus,4 whereas, on the other hand, immunosuppressive treatment of GVHD (eg, steroids, cyclosporine, tacrolimus) can hamper thymopoiesis as well. Therefore, thymic damage from GVHD needs to be balanced from that of immunosuppression. Therapeutic drug monitoring, such as for levels of tacrolimus,78 cyclosporine,79 and mycophenolate,80 can reduce the probability of thymic damage by GVHD, while limiting their effects on thymopoiesis by targeting to the appropriate exposure. Furthermore, of interest are several therapies linked to normal thymic function that are currently being investigated to directly promote thymopoiesis after allo-HCT (Figure 2).
Overview on timing of noncellular posttransplantation interventions to improve T-cell IR via HPE and thymopoiesis.
Overview on timing of noncellular posttransplantation interventions to improve T-cell IR via HPE and thymopoiesis.
Improving T-cell IR through HPE
IL-2.
Interleukin-2 (IL-2) was introduced in the HCT setting for its role in the differentiation of T cells into effector cells and promotion of T-, B-, and NK-cell proliferation. Although IL-2 can have severe side effects at higher dosage (eg, capillary leak syndrome), low-dose IL-2 administration after HCT reduced relapse probability, probably due to an increased GVL response.81,82 It also restored homeostasis of CD4+ T cells, and increased Treg counts, associated with clinical improvement of chronic GVHD (cGVHD), whereas no adverse events were noted.83,84 Therefore, low-dose IL-2 therapy may improve T-cell IR, contributing to GVL, without increasing GVHD probability.
IL-15.
IL-15 is another interesting cytokine for improving HPE, as it is important for the expansion of B and T cells and for the survival of NK cells. In a murine HCT model, IL-15, during the first month after HCT, was associated with early T-cell and NK-cell IR.85 In humans, no systemic IL-15 therapy after allo-HCT has been evaluated so far. Only IL-15–stimulated CD3/CD19-depleted graft cells, from part of the HCT graft, or IL-15–activated cytokine-induced killer cells have been studied, albeit in few patients. Interestingly, this therapy increased NK, NKT, and T-cell numbers at 15 to 30 days after receipt, without exacerbating GVHD,86 and showed GVL potential when given at the initiation of relapse.87 IL-15 stimulation of stem cells would, therefore, be interesting to evaluate in future studies.
Improving T-cell IR through thymopoiesis
IL-7.
The administration of IL-7 was investigated in the HCT setting, as it naturally promotes the differentiation and proliferation of naive T cells. Treatment with recombinant IL-7 after HCT enhanced TCR diversity, induced a doubling of (mainly memory) CD4 and CD8 T cells, with no effects on Tregs, NK, or B cells.88 Interestingly, IL-7 also increased the amount of functional T cells, including virus-specific T cells, whereas no significant increase in GVHD or other serious toxicities were seen.88 These first results show promise for IL-7 in enhancing T-cell IR after HCT.
KGF.
Keratinocyte growth factor (KGF) promotes proliferation and maturation of immature T cells and plays a role in postnatal thymic regeneration. KGF, or palifermin, is used as standard-of-care peri-HCT therapy in some centers, and is US Food and Drug Administration (FDA) approved to prevent mucositis. Treatment of HCT patients with KGF, during 3 days before and 3 days after conditioning therapy, indeed not only decreased mucositis, but also prevented damage to the thymus.89,90 Although not all studies found any noteworthy impact of KGF on T-cell IR directly,89 this protection from thymic damage showed enhanced thymopoiesis, with early T-cell recovery probably caused by induction of IL-7, and lower GVHD incidence.90
Sex steroid ablation.
Sex steroids are known to inhibit thymic function. Thus, sex steroid ablation may be applied to improve thymopoiesis. Administration of luteinizing hormone-releasing hormone (LHRH) agonists after HCT showed enhanced TCR excision circle production and T-cell repertoire regeneration, with enhanced total and naive CD4+ T-cell regeneration,91 indicating thymopoiesis. However, a major limitation of this approach is the surge in sex steroid after LHRH-agonist treatment, so a more rational approach could be to use LHRH antagonists.92 Another strategy for sex steroid ablation, leuprolide acetate (Lupron), in combination with KGF, showed increased reconstitution of naive CD4+ and CD8+ T cells, with a more diverse T-cell repertoire, in mice.93 Currently, phase 2 clinical studies are under way evaluating the effect of Lupron in the human allo-HCT setting (clinicaltrials.gov identifier: fNCT01338987).
Thymosin α 1.
Thymosin α 1 (Tα1) has recently been investigated in the HCT setting, as the thymus naturally promotes T-cell development by secreting this hormone. Tα1 (Thymalfasin/Zadaxin) is a FDA approved orphan drug for treatment of chronic hepatitis B, with no adverse effects found in recipients from 13 months to 99 years old.94 In the human HCT setting, Tα1 administration showed encouraging first results on T-cell IR. Subcutaneous administrations of Tα1, twice weekly for 4 weeks after allo-HCT, caused increased CD4+ T-cell recovery and pathogen-specific T cells to appear already at 1 month after HCT, which was earlier and in higher levels compared with controls.95 Additionally, Tα1 lowered the cumulative incidence of nonrelapse mortality (mainly infection-related) and increased event-free survival.94,95 Therefore, Tα1 therapy might be a promising novel therapy to enhance T-cell IR after allo-HCT.
Cellular immunotherapies to improve immunity
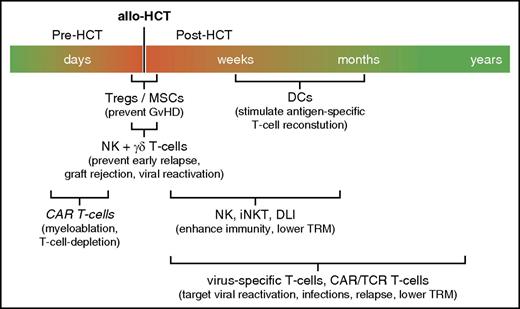
The lack of effector immune cells after allo-HCT may be compensated for with adjuvant cell-based immunotherapies. Due to high costs, regulatory burden, and complicated production, cellular immunotherapies are currently not widely being used in the HCT setting. They mainly have potency to be used to treat life-threatening complications such as relapse, viral reactivations, and GVHD, but could also be used prophylactically. Here, we discuss the most potent cellular immunotherapies currently used to improve immunity after allo-HCT (Figure 3).
Overview on timing of cellular immunotherapies to improve immunity after allo-HCT. iNKT, invariant NKT; TRM, transplantation-related mortality.
Overview on timing of cellular immunotherapies to improve immunity after allo-HCT. iNKT, invariant NKT; TRM, transplantation-related mortality.
DC vaccination.
Dendritic cells (DCs) are highly specialized antigen-presenting cells that regulate the balance between action (relevant for GVL) and suppression of the immune system (relevant for GVHD).96 Therefore, DC vaccination is of major interest as a tool to modulate immune responses after allo-HCT. For BMT/peripheral blood cell transplantation, DCs can either be obtained by culturing monocytes into monocyte-derived DCs, or by directly isolating plasmacytoid DCs or conventional (myeloid) DCs from the peripheral blood of the donor. However, the low number of circulating DCs complicates their clinical application. In the case of CBT, CD34+ stem cells from part of the CB unit can easily be differentiated ex vivo into potent CB-DCs targeting viral and fungal infections after HCT, and even relapse.97,98 In addition, tolerogenic DCs might be a future therapy to suppress GVHD, as shown in a murine HCT model.99
γδ T cells.
Increased numbers of donor γδ T cells early after allo-HCT correlate with better overall survival of leukemia patients, without increased risk of GVHD.100 Therefore, γδ T cells hold promise to improve outcome after allo-HCT. To date, trials using γδ T cells focus only on activated autologous Vγ9Vδ2 γδ T cells, combined with IL-2, or activated and amplified ex vivo.101 This stresses the need for future evaluation of the implementation of these potent cells in the allogeneic HCT setting, as is currently being investigated in a setting that combines γδ T cells and NK cells.102,103
NK cells.
Adoptive NK-cell immunotherapy in the allo-HCT setting is under investigation as well. Results from one of the earliest studies suggest limited adverse events and no induction of GVHD.104 More recently, the combination of NK and γδ T cells was evaluated as a cell-based immunotherapy after allo-HCT. It is suggested that infusion of NK cells and γδ T lymphocytes around the time of HCT may protect the patient from early relapse, viruses (in particular, cytomegalovirus [CMV]), and graft rejection.105 Initial efforts are currently under way using TCR-αβ/CD19-depleted cell populations, which contain CD34+ progenitors, as well as mature NK cells and γδ T cells.102,103
NKT cells.
For their immunomodulatory properties, immunotherapy using NKT cells could be useful in the allo-HCT setting as well. NKT cells play a role in both tumor surveillance and GVHD,106 with early reconstitution suggested to be predictive of lower relapse and GVHD risk and higher survival.107,108 Clinical trials implementing expanded NKT cells in the allo-HCT setting are currently under way.
Engineered T cells.
One method to improve T-cell recovery is donor lymphocyte infusion (DLI). This nonspecific T-cell therapy is, however, associated with increased risk on GVHD.109 Furthermore, because of the low frequency of T cells reactive against many common viruses within the circulation, higher DLI doses may be required to confer clinical benefit against viruses, consequently increasing the risk of GVHD.
A more targeted method to enhance T-cell immunity after allo-HCT is with adoptively transferred antigen-specific T cells. These T cells can be expanded ex vivo after stimulation with antigen-presenting cells presenting specific antigens, such as CMV, Epstein-Barr virus, and adenovirus,110 or against malignant cells to induce GVL.111 A drawback of this therapy is the long time needed for production of specific T cells. γ capture, based on interferon γ production, of functional antigen-specific T cells from a donor is a faster alternative. But for this method, the presence of specific T cells is essential and demands a seropositive donor. This is a challenge when the donor lacks viral immunity, or with CB which generally contains virus-naive immune cells. Nevertheless, virus-specific T cells can also be cultured from naive CB T cells.112
Another way is T-cell gene therapy to produce chimeric antigen receptor (CAR) T cells or engineer T cells to express specific TCRs (TCR-T cells). Based on the chosen CAR or TCR binding domain, these modified T cells can be used to target viruses, and leukemic cells can be used to target relapse (eg, CART19, WT1-TCR-T cells).113-115 But they can potentially also be used as an alternative myeloablative therapy.116 Drawbacks of genetically modified T-cell therapy, however, are possible cytotoxic effects on normal cells that express target antigens.115 Nevertheless, the specificity and potency of this therapy is shown by the finding that donor-derived anti-CD19-CAR T cells induce complete remission in relapsed patients, without exacerbating GVHD.117 In addition, these cells have been shown to persist for over 3 years, providing long-term protection against their target.114
Tregs and MSCs.
Tregs and mesenchymal stromal/stem cells (MSCs) can inhibit immune responses, and have been investigated as adjuvant cell therapies to treat or prevent GVHD. The nonspecific MSC therapy did not prevent GVHD when cotransplanted alongside the HCT graft,118 whereas even increased relapse rates and mortality were noted.119 However, reduced aGVHD risk was seen when given after HCT before GVHD onset.120 Coinfusion of Tregs alongside the HCT graft decreased the occurrence of aGVHD and cGVHD, while maintaining GVL.121,122 This also resulted in high frequencies of pathogen-specific CD4+ and CD8+ T cells already at 2 months after HCT and decreased incidence of CMV disease, showing strong antiviral protection after pandemic influenza vaccination.122 No negative effects due to the Treg infusion were reported. Furthermore, transplantation with CB-derived Tregs directly after CBT showed an increase in viral infections within 30 days of infusion, but lowered the occurrence of GVHD without increased risk of relapse.121,123 This may make Treg immunotherapy a promising strategy to decrease the risk for GVHD associated with better T-cell IR potential.
Concluding remarks and future perspective
We have summarized a broad variety of novel strategies before, during, and after HCT to improve T-cell IR, aiming to decrease the risk of complications and increase survival chances. Selecting the appropriate HCT source and graft manipulations are the first critical factors affecting T-cell IR after transplantation. Individualizing the conditioning regimen is crucial as well, especially for compounds that dramatically influence T-cell IR, such as ATG. Furthermore, enhancing homeostatic peripheral expansion, preventing thymic damage, and promoting thymopoiesis are important in enhancing T-cell IR. Better disease control may be achieved with adjuvant (specific) cellular immunotherapies to prevent GVHD and promote immunity against pathogens and cancer cells. A combination of these pre-, peri-, and post-HCT strategies probably will most potently enable timely and balanced T-cell recovery.
Immunomonitoring will be of major importance to identify patients at risk, which would provide opportunities for early immune interventions. For instance, patients with low T-cell counts early after HCT, and/or low TCR diversity, are at risk for HCT-related complications and could benefit from adjuvant immunotherapies, such as low-dose IL-2, administration of Tregs, or leukemia/virus-specific DCs and/or specific T cells. New functional measures of immune recovery would, therefore, also guide clinicians in the assessment of IR beyond simple absolute lymphocyte counts. In addition, it is important to continue adequate supportive care with continuation of antimicrobial prophylaxis and polymerase chain reaction monitoring for viruses until adequate immune recovery occurs.
Standardization and harmonization of immunomonitoring would enable better comparison between multiple allo-HCT studies, in order to better understand the biology of IR, and find biomarkers.124 These biomarkers will help the physician guide the developing immune system, and anticipate complications in order to avert them. This will pave the path to precision transplantation in the future, in which allo-HCT therapy will be personalized, using a combination of strategies to boost T-cell IR, subsequently resulting in lower morbidity and higher survival after allo-HCT.
Acknowledgments
The authors thank Paul Besseling for his help with searching for recent, relevant literature on strategies to improve IR after HCT.
This work was supported by a Kinderen Kankervrij (KIKA) grant (project 142).
Authorship
Contribution: C.d.K. wrote and edited the report; S.N. and J.J.B. reviewed the manuscript and provided critical comments; and all authors reviewed and approved the final report.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Jaap Jan Boelens, Blood and Marrow Transplantation Program and Laboratory of Translational Immunology, University Medical Center Utrecht, Lundlaan 6: KC 0.30.063.0, 3584 CX Utrecht, The Netherlands; e-mail: j.j.boelens@umcutrecht.nl.