Abstract
Introduction: Risk-adapted therapy in curable hematologic malignancies is commonly applied: low-risk patients (pts) may be cured with less intensive treatment, avoiding excessive toxicity, whereas high-riskpts require more intensive and toxic regimens. In multiple myeloma (MM), this model may not apply, since the disease is incurable. In recent years, there has been a marked improvement in patient outcome, due to the introduction of novel agents and optimized treatment strategies, including the use of transplant and maintenance. A better evaluation ofpts prognosis based on the new revised international staging system (R-ISS) has been also introduced in clinical practice. The objective of this analysis was to evaluate the impact of treatment intensification (specifically autologous stem cell transplantation [ASCT] and maintenance) inpts with different prognostic features.
Methods: Data from 3 phase III randomized trials in newly diagnosed MMpts (RV-MM-209; EMN441; GIMEMA-MM0305) were pooled together and analyzed. Baseline patient risk assessment was estimated using R-ISS. We evaluated: 1) the impact of treatment intensification with high-dose therapy followed by ASCTvs no-ASCT inpts with R-ISS Stage Ivs Stage II/III; 2) the impact of treatment intensification with maintenancevs no maintenance inpts with R-ISS Stage Ivs Stage II/III. RV-MM-209 and EMN441 studies randomizedpts to ASCTvs no-ASCT; allpts in the GIMEMA-MM0305 trial did not receive ASCT and were excluded from the first comparison; RV-MM-209 and GIMEMA-MM0305 studies randomizedpts to maintenance or no maintenance after induction/consolidation; allpts in the EMN441 trial received maintenance and were excluded from the second comparison. We evaluated progression free survival-1 (PFS1), PFS2 and overall survival (OS). Cox proportional hazards models were used to estimate hazard ratios (HRs). To account for potential confounders, the comparisons between ASCTvs no-ASCT and maintenancevs no maintenance were adjusted for the trial effect and the main prognostic features.
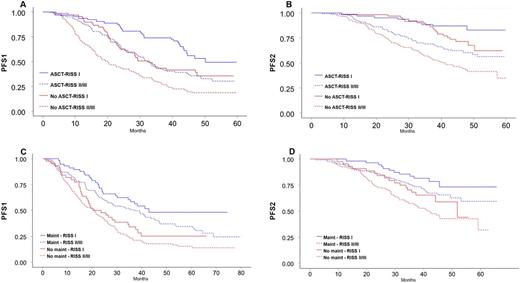
Results: Overall, 1302 pts were enrolled in the 3 trials. Median follow-up was 4 years.Comparison ASCTvs no-ASCT: 791pts were enrolled in the 2 trials, 529 were eligible for the ASCTvs no ASCT comparison. R-ISS Stage data were available for 419 pts. There was an overall advantage for ASCTvs no-ASCT in PFS1 (0.53; p<0.001), PFS2 (HR 0.53; p<0.001) and OS (HR 0.51; p<0.001). The 4-year PFS1 was 53% inpts with R-ISS Stage I randomized to ASCT, 35% inpts with R-ISS Stage II/III randomized to ASCT, 36% inpts with R-ISS Stage I randomized to no-ASCT and 19% in those with R-ISS Stage II/III randomized to no-ASCT (p<0.001); the 4-year PFS2 was 83%, 60%, 71% and 43% in the 4 subgroups, respectively (p<0.001) (Figure 1A, B); the4-year OS was 95%, 75%, 88% and 61%(p<0.001). Comparison maintenancevs no maintenance: 913pts were enrolled in the 2 trials, 550 could be eligible for maintenance. R-ISS data were available in 403 pts. Maintenance significantly improved PFS (HR 0.54, p<0.001), PFS2 (HR 0.52, p<0.001) and OS (HR 0.69, p=0.027) in comparison with no maintenance. The 4-year PFS was 48% forpts with R-ISS Stage-I assigned to maintenance, 37% forpts with R-ISS Stage II/III assigned to maintenance, 25% forpts with R-ISS Stage-I assigned to no maintenance and 18% forpts with R-ISS Stage II/III assigned to no maintenance (p<0.001); the 4-year PFS2 was 73%, 66%, 59% and 43% in the 4 subgroups, respectively (p<0.001) (Figure 1C, D); the 4-year OS was 80%, 73%, 77% and 63% (p<0.001).
Conclusions: Both ASCT and maintenance improved PFS1, PFS2 and OS in MM pts. The highest survival was reported in patients with R-ISS Stage I receiving ASCT and/or maintenance. Low-riskpts (R-ISS Stage I) not undergoing intensification with ASCT or maintenance lose their prognostic advantage over high-risk patients receiving the same intensification.
Gay:Janssen-Cilag: Other: Advisory Board; Celgene: Honoraria; Amgen: Honoraria; BMS: Honoraria; Takeda: Honoraria, Other: Advisory Board; Mundipharma: Other: Advisory Board. Hajek:Novartis: Research Funding; Takeda: Consultancy, Honoraria, Research Funding; Onyx: Consultancy; BMS: Honoraria; Amgen: Consultancy, Honoraria, Research Funding. Bringhen:Mundipharma: Other: Advisory Board; Karyopharm: Other: Advisory Board; BMS: Honoraria; Janssen-Cilag: Honoraria; Amgen: Other: Advisory Board; Celgene: Honoraria. Gaidano:Gilead: Consultancy, Honoraria, Speakers Bureau; Morphosys: Consultancy, Honoraria; Roche: Consultancy, Honoraria, Speakers Bureau; Karyopharm: Consultancy, Honoraria; Janssen: Consultancy, Honoraria, Speakers Bureau; Novartis: Consultancy, Honoraria, Speakers Bureau. Caravita:Janssen-Cilag: Honoraria. Cavo:Millennium: Consultancy, Honoraria; Janssen-Cilag: Consultancy, Honoraria; Celgene: Consultancy, Honoraria; Bristol-Myers Squibb: Consultancy, Honoraria; Amgen: Consultancy, Honoraria. Foà:Pfizer: Speakers Bureau; Ariad: Speakers Bureau; BMS: Consultancy; Celgene: Consultancy, Speakers Bureau; Amgen: Consultancy, Speakers Bureau; Gilead: Consultancy, Speakers Bureau; Janssen-Cilag: Consultancy, Speakers Bureau; Genetech: Consultancy; Roche: Consultancy, Speakers Bureau. Patriarca:Bristol-Myers Squibb: Other: Advisory board; Mundipharma: Other: Advisory board; Janssen-Cilag: Other: Advisory board; MSD: Consultancy; Celgene: Consultancy. Ria:Italfarmaco: Consultancy, Speakers Bureau; Janssen-Cilag: Other: Advisory Board, Speakers Bureau; CSL Behring: Consultancy, Research Funding, Speakers Bureau; Binding Site: Speakers Bureau; BMS: Speakers Bureau; BMS: Speakers Bureau. Palumbo:Janssen Cilag: Honoraria; Takeda: Employment, Honoraria. Boccadoro:Novartis: Honoraria, Research Funding; Mundipharma: Research Funding; SANOFI: Honoraria, Research Funding; Janssen: Honoraria, Research Funding; Abbivie: Honoraria; Amgen: Honoraria, Research Funding; CELGENE: Honoraria, Research Funding; BMS: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal