Background
Allogeneic stem cell transplantation (HSCT) involves the transfer of healthy donor hematopoietic cells, including hematopoietic stem cells (HSCs) and mature immune effector cells, to recipients with high-risk hematologic malignancies. The success of HSCT is fundamentally dependent on engraftment of normal donor-derived hematopoiesis. Rarely, donor-derived cells undergo transformation to myeloid leukemia as a late complication of HSCT (donor cell leukemia, DCL), a process linked in some cases to pre-existing mutations in donor hematopoietic stem cells (HSCs). In healthy older adults, HSC mutations can cause clonal hematopoiesis of indeterminate potential (CHIP), which is associated with increased risk of hematologic malignancy and an increased risk of all-cause mortality. Among donors over age 40, the frequency of donor CHIP can be estimated to be 5 to 20-fold higher than the frequency of donor cell leukemia, suggesting that non-leukemic endpoints of donor derived clonality may be more prevalent and consequential than previously recognized.
Methods
We performed targeted next generation sequencing in patients who developed peripheral cytopenias or myeloid neoplasms in the context of 100% donor cell chimerism after allogeneic HSCT. We also prospectively sequenced potential donors who had abnormal CBC parameters, including WBC differential and RBC indices. To determine whether the mutations detected in recipients were of donor derivation, and to assess clonal evolution over time, we performed ultra-deep genotyping at 30,000-100,000X or droplet digital PCR (ddPCR) in the donor stem cell product and serial post-SCT samples.
Results
We identified four allogeneic SCT recipients with 100% chimerism who met inclusion criteria, two with late-onset hematologic malignancy (latency 23 and 10 years) and two with progressive cytopenias but no evidence of hematologic malignancy on bone marrow examination (latency 18 and 13 months). In each of these patients, sequencing of bone marrow or peripheral blood specimens revealed at least one somatic mutation (SF3B1 K666Q; U2AF1 S34F; DNMT3A T868N; DNMT3A Q356X) that could be used to assess the possibility of donor derivation.
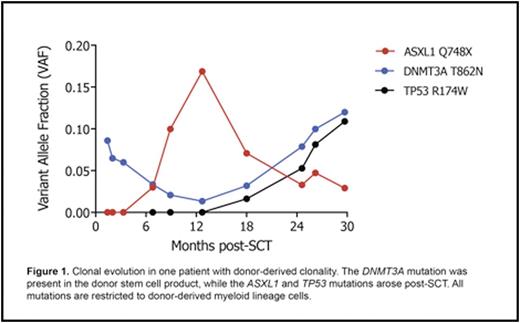
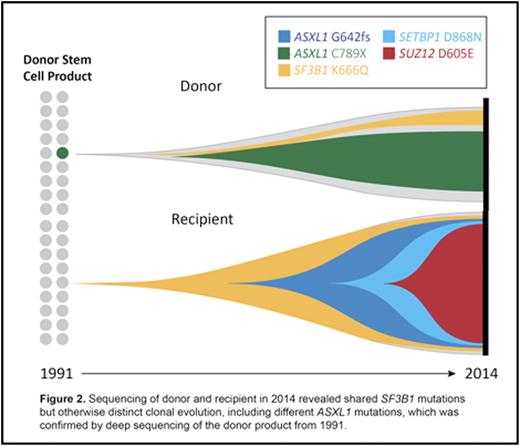
In all patients, we identified at least one mutation present in both the diagnostic post-HSCT recipient sample and the pre-HSCT banked donor stem cell product. Figure 1 shows post-HSCT clonal evolution from one case. In another case, we evaluated contemporaneous samples from the donor and recipient obtained at the time of diagnosis of DCL in the recipient (23 years after HSCT). We identified two key findings: 1) a shared SF3B1 K666 mutation in donor and recipient, and 2) divergent clonal evolution, with ASXL1 C789X in the donor, and ASXL1 G642fs, SETBP1 D868N, and SUZ12 D605E in the recipient (Figure 2). In this context, the recipient had a morphologic diagnosis of MDS/MPN overlap, while the donor had abnormal RBC indices but no cytopenias.
Since CHIP is associated with subtle abnormalities in hematologic parameters even in the absence of overt cytopenias, we evaluated potential donors with non-exclusionary CBC abnormalities, such as abnormal white blood cell differential or elevated MCV. In two cases, we prospectively identified DNMT3A mutations (R736Cand R882H, variant allele fractions 11.5% and 2%, respectively), consistent with donor CHIP. In one case, the donor with CHIP was used for transplantation. At 90 days after HSCT, donor cell chimerism was 99%; sequencing of recipient peripheral blood revealed the donor-derived DNMT3A mutation and the recipient remained persistently anemic, macrocytic, and thrombocytopenic.
Conclusion
We identified healthy stem cell donors with clonal hematopoiesis, marked by mutations in canonical genetic drivers of myeloid malignancies. In each instance, the aberrant clone engrafted in the transplant recipient, underwent selective expansion, and caused development of abnormal hematopoietic function. Our findings suggest that donor-derived clonal hematopoiesis may be common, especially in grafts from older donors, and that donor CHIP may confer an unrecognized and increased risk of leukemic and non-leukemic endpoints. We further demonstrate that donor CHIP can be identified prospectively, thus highlighting an emerging challenge in HSCT that may influence donor selection strategies as the clinical significance of donor CHIP is systematically elucidated.
Ritz:Kiadis: Membership on an entity's Board of Directors or advisory committees. Soiffer:Juno: Membership on an entity's Board of Directors or advisory committees; Kiadis: Membership on an entity's Board of Directors or advisory committees; Jazz Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees. Lindsley:MedImmune: Research Funding; Takeda Pharmaceuticals: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal