Abstract

Introduction: While the presence of HIV portends a poor prognosis in many malignancies, its clinical association with MDS and AML has not been well studied, and is known primarily from small case reports and case series. We evaluated the prevalence and clinical course of unexplained cytopenias and clinically proven MDS/AML in a large cohort of HIV-positive (HIV+) patients (pts) seen at a single center, and compared their clinical course to MDS/AML in non-HIV (HIV-) pts.
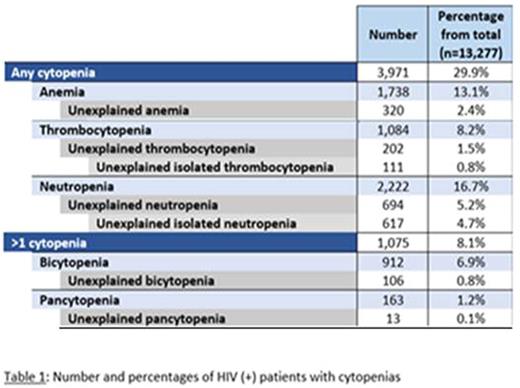
Methods: Data from 15,120 HIV+ pts seen between 1/1/1997 to 6/1/2016 was analyzed for hematologic parameters, HIV status (CD4 count, HIV viral load), chronic disease status and nutrient deficiencies. Anemia was defined as hemoglobin<10, thrombocytopenia as platelets<100 and neutropenia as absolute neutrophil count of <1800, as per the MDS IPSS criteria. Pts with no obvious causes for their cytopenias, such as advanced AIDS, opportunistic infections, chronic kidney disease or nutrient deficiency anemia were determined to have unexplained cytopenias. Furthermore, pts with multiple lineage cytopenias were assessed for evidence of primary bone marrow etiology.
Results: Out of 13,277 HIV+ pts that had evaluable blood counts, 1075 pts (8.1%) had cytopenias affecting more than one lineage. 912 pts had bilineage cytopenias and 163 pts had a pancytopenia. This was significantly higher than the frequency of bi/trilineage cytopenias in a non-HIV elderly population that was recently analyzed; 8.1% in HIV+ pts vs 0.9% in non-HIV pts, p <0.0001. Out of a total of 466 cytopenic pts that had all evaluable blood test results, including HIV parameters and chronic disease labs, 119 pts (25.6%) were found to have unexplained bi/trilineage cytopenias with a CD4 count of >250 and HIV viral load <100. Pts with unexplained bi/trilineage cytopenias also presented at relatively younger age (median age 47 years (yrs) (range 24-70 yrs), than pts presenting with MDS.
We also identified 10 MDS and 9 AML pts in our HIV+ cohort. Mean CD4 count for these cases was 340 cells/mm3, with only 4 pts < 200 cells/mm3. Median time to MDS or AML diagnosis from date of HIV diagnosis was 15.6 and 13.7 yrs respectively. All pts were receiving anti-retroviral therapy at the time of MDS or AML diagnosis. Only 3 MDS pts and 1 AML patient had a history of prior exposure to chemotherapy. Clinical characteristics of the HIV+ MDS pts (n=10) were compared to HIV- MDS pts (n=135) from the same institution diagnosed between 1997-2011. HIV+ MDS pts presented at a younger age (59.5 vs 70.6 yrs, p = 0.001) and also had significantly higher risk (Int-2/High) disease by IPSS (87.5% vs 17.8%, p <0.001). HIV+ AML pts also presented at a younger age compared with known historical data (56 vs 69 yrs, p = 0.002). Cytogenetic abnormalities were found in 6 of 7 (85.7%) evaluable HIV+ MDS pts, with monosomy 7 being the commonest alteration (71.4%). Six (60%) of the HIV+ MDS pts progressed to AML, with a mean time to progression of 10.4 months. Importantly, HIV+ MDS pts had significantly worse overall survival compared to controls (9.6 vs 58.2 mo, p < 0.001, Figure 1.). Univraiate analysis of MDS pts confirmed that HIV+ pts had statistically significant worse OS, higher risk cytogenetics and younger age at presentation. HIV+ AML pts exhibited poor overall survival of 9.5 mo (range 39-73 yrs).
Conclusions: Anemia occurs in most HIV pts at some point in their course, however, bicytopenia and pancytopenia are generally thought to be uncommon, especially in pts with well-controlled disease. We demonstrated in our cohort an unexpectedly high prevalence of unexplained bi/trilieneage cytopenias, not associated with advanced HIV, chronic disease or nutrient deficiencies. This finding suggests the presence of an independent, HIV-specific, mechanism of hematopoietic suppression, acting either at the level of the stem cell, or the bone marrow milieu.
We also report on the largest cohort of HIV+ MDS/AML cases in the literature and demonstrate that HIV+ pts who develop MDS and AML do so at a younger age, present with more advanced disease that is resistant to standard therapy, and have worse overall survival than a control cohort of HIV- pts. These data present evidence that suggests that MDS should be considered as a diagnosis early in HIV. Appropriate risk stratification and new therapeutic approaches are needed.
Kaplan-Meier curve comparing overall survival in HIV infected and non-HIV infected MDS patients.
Kaplan-Meier curve comparing overall survival in HIV infected and non-HIV infected MDS patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal