Abstract
Congenital hypoplasminogenemia (HPG) is characterized by markedly impaired extracellular fibrinolysis leading to the formation of ligneous (woody) pseudomembranes on mucosal surfaces, including the eye, mouth, bronchopulmonary tree, and genitourinary tract. HPG is caused by homozygous or compound-heterozygous mutations in the plasminogen gene (PLG; 6q26).
We present a report of the first therapeutic use of replacement therapy with plasminogen purified from human plasma. A male of Turkish descent was diagnosed at 4 weeks of age with congenital hypoplasminogenemia following presentation with typical ligneous conjunctivitis. The serum plasminogen activity level was < 2% (Reference range 75-140%), and the diagnosis was confirmed by genetic testing showing a novel homozygous splice-site mutation in PLG (c.1587+1 G>A).
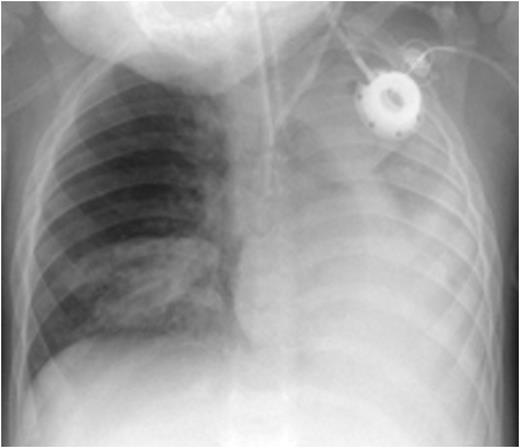
At 2 months of age he suffered a severe respiratory syncytial virus (RSV) infection requiring ventilatory support for 5 days and a 1 month hospitalization. From this time he had recurrent respiratory problems. From 4 months of age he was treated with fresh frozen plasma (FFP) 20 mL/kg/week. At 18 months of age he was found to have exophytic lesions within both the right and left main bronchi. He had one incident of acute severe dyspnea with cyanosis which responded to non- invasive oxygen insufflation. Subsequently he had repeated bronchoscopies with laser removal of bronchial lesions with FFP cover. At 20 months of age during preparation for bronchoscopy he had an episode of acute cyanosis and cardiac arrest with asystole and was resuscitated after 30 minutes. CXR showed atelectasis of the left lung and of the right lower lobe. He was admitted to the ICU and required both ventilatory and circulatory support. Profuse viscous lung secretions were aspirated.
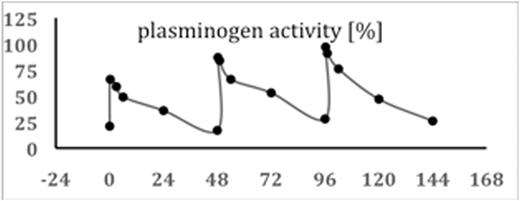
One week later he was given a dose of plasminogen of 4 mg/kg, with a second dose of 6 mg/kg and subsequent doses of 6.5 mg/kg every 48 hours. The pharmacokinetics are shown in the Figure. Note that baseline level before the first dose is 21% due to FFP therapy.
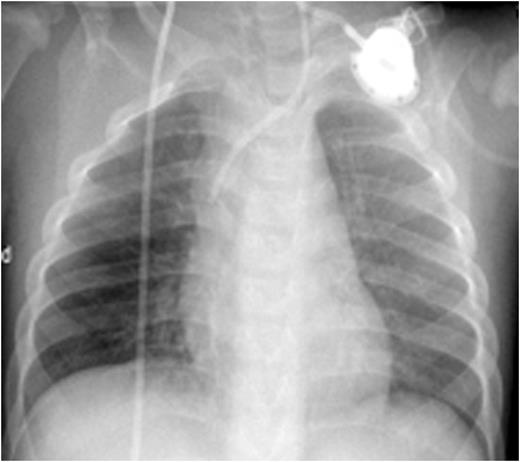
Progressive dissolution of the membranes and exophytic lesions with some blood spotting, was noted, and was associated with decreased oxygen requirements. Improvement in the ligneous eye lesions was also observed. After 4 days he was extubated., but required reintubation after 36 hours due to exhaustion; he was finally extubated 1 week after receiving the first dose of plasminogen. Plasminogen replacement has continued with a regimen of 6.5 mg/kg every second day. There has been progressive dissolution of the membranes with greatly reduced lesions seen after 6 weeks of treatment.
CXR before administration of plasminogen showed atelectasis of the left lung and of the right lower lobe (left panel). Six weeks after initiation of regulalar plasminogen substitution ventilation in both lungs had improved significantly (right panel)
In this patient substitution with plasminogen was effective and showed no significant side effects. Patients with severe plasminogen deficiency might benefit from prophylactic or early treatment to prevent severe complications such as occurred in this patient.
Moran:ProMetic Life Sciences, Inc.: Employment, Equity Ownership, Membership on an entity's Board of Directors or advisory committees. Schneppenheim:Baxalta, now part of Shire: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal