Abstract

To develop a prognostic scoring system tailored for therapy-related myelodysplastic syndromes (tMDS), we put together a database containing 1933 patients (pts) with tMDS from Spanish, German, Swiss, Austrian, US, Italian, and Dutch centers diagnosed between 1975-2015. Complete data to calculate the IPSS and IPSS-R were available in 1603 pts. Examining different scoring systems, we found that IPSS and IPSS-R do not risk stratify tMDS as well as they do primary MDS (pMDS), thereby supporting the need for a tMDS-specific score (Kuendgen et al., ASH 2015). The current analysis focuses on cytogenetic information as a potential component of a refined tMDS score, based on this large, unique patient cohort.
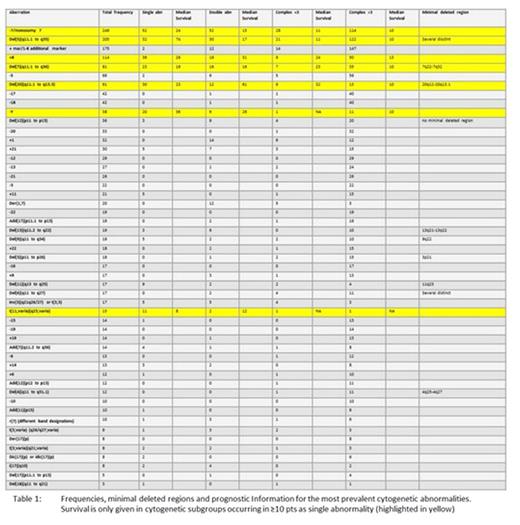
Of the 1933 pts, 477 had normal karyotype (KT), 197 had missing cytogenetics, while 467 had a karyotype not readily interpretable. Incomplete karyotype descriptions will be reedited for the final evaluation. Of the remaining 1269 pts the most frequent cytogenetic abnormalities (abn) were: -7, del(5q), +mar, +8, del(7q), -5, del(20q), -17, -18, -Y, del(12p), -20, and +1 with >30 cases each. Frequencies are shown in Table 1. Some abn were observed mostly or solely within complex KTs, such as monosomies, except -7. Others, like del(20q) or -Y, are mainly seen as single or double abn, while del(5q), -7, or del(7q) are seen in complex as well as non-complex KTs.
The cytogenetic profile overlapped with that of pMDS (most frequent abn: del(5q), -7/del(7q), +8, -18/del(18q), del(20q), -5, -Y, -17/del(17p), +21, and inv(3)/t(3q) (Schanz et al, JCO 2011)), with notable differences including overrepresentation of complete monosomies, a higher frequency of -7 or t(11q23), and a more frequent occurrence of cytogenetic subtypes in complex KTs, which was especially evident in del(5q) occurring as a single abn in 16%, compared to 70% within a complex KT.
IPSS-R cytogenetic groups were distributed as follows: Very Good (2%), Good (35%), Int (17%), Poor (15%), Very Poor (32%). Regarding the number of abn (including incomplete KT descriptions) roughly 30% had a normal KT, 20% 1, 10% 2, and 40% ≥3 abn, compared to pMDS: 55% normal KT, 29% 1, 10% 2, and 6% ≥3 abn.
To be evaluable for prognostic information, abn should occur in a minimum of 10 pts. As a single aberration this was the case for -7, +8, del(5q), del(20q), del(7q), -Y, and t(11;varia) (q23;varia). Of particular interest, there was no apparent prognostic difference between -7 and del(7q); del(5q) as a single abn was associated with a relatively good survival, while the prognosis was poor with the first additional abn; t(11q23) occurred primarily as a single abn and was associated with an extremely poor prognosis, and prognosis of pts with ≥4 abn was dismal independent of composition (Table 1).
To develop a more biologically meaningful scoring system containing homogeneous and prognostically stable groups, we will further combine subgroups with different abn leading to the same cytogenetic consequences. For example, deletions, unbalanced translocations, derivative chromosomes, dicentric chromosomes of 17p, and possibly -17 all lead to a loss of genetic material at the short arm of this respective chromosome affecting TP53.
Further information might be derived from analyses of the minimal common deleted regions. For some abn, like del(11q), del(3p), and del(9q), this can be refined to one chromosome band only (table 1).
Conclusion: Development of a robust scoring system for all subtypes of tMDS is challenging using existing variables. This focused analysis on the cytogenetic score component shows that favorable KTs are evident in a substantial proportion of pts, in contrast to historic data describing unfavorable cytogenetics in the majority of pts. Although complex and monosomal KTs are overrepresented, this suggests the existence of distinct tMDS-subtypes, although some of these cases might not be truly therapy-induced despite a history of cytotoxic treatment. The next steps will be to analyze the prognosis of the different groups, develop a tMDS cytogenetic score, and examine minimal deleted regions to identify candidate genes for development of tMDS, as well as to describe the possible influence of different primary diseases and treatments (radio- vs chemotherapy, different drugs) on induction of cytogenetic subtypes. Our detailed analysis of tMDS cytogenetics should reveal important prognostic information and is likely to help understand mechanisms of MDS development.
Komrokji:Novartis: Consultancy, Speakers Bureau; Celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding. Sole:Celgene: Membership on an entity's Board of Directors or advisory committees. Sekeres:Celgene: Membership on an entity's Board of Directors or advisory committees; Millenium/Takeda: Membership on an entity's Board of Directors or advisory committees. Roboz:Cellectis: Research Funding; Agios, Amgen, Amphivena, Astex, AstraZeneca, Boehringer Ingelheim, Celator, Celgene, Genoptix, Janssen, Juno, MEI Pharma, MedImmune, Novartis, Onconova, Pfizer, Roche/Genentech, Sunesis, Teva: Consultancy. Steensma:Amgen: Consultancy; Genoptix: Consultancy; Janssen: Consultancy; Celgene: Consultancy; Millenium/Takeda: Consultancy; Ariad: Equity Ownership. Schlenk:Pfizer: Honoraria, Research Funding; Amgen: Research Funding. Valent:Amgen: Honoraria; Deciphera Pharmaceuticals: Research Funding; Celgene: Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Ariad: Honoraria, Research Funding; Deciphera Pharmaceuticals: Research Funding. Giagounidis:Celgene Corporation: Consultancy. Giagounidis:Celgene Corporation: Consultancy. Platzbecker:Celgene Corporation: Honoraria, Research Funding; TEVA Pharmaceutical Industries: Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Janssen-Cilag: Honoraria, Research Funding; Amgen: Honoraria, Research Funding. Lübbert:Janssen-Cilag: Other: Travel Funding, Research Funding; Celgene: Other: Travel Funding; Ratiopharm: Other: Study drug valproic acid.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal