Abstract
Background: Fludarabine and clofarabine are purine nucleoside analogues with established clinical activity in acute myeloid leukemia (AML). We sought to evaluate the relative safety and efficacy of idarubicin and cytarabine with either clofarabine (CIA) or fludarabine (FAI) in adult patients (pts) with newly diagnosed AML.
Methods: Adult pts ≤60 years of age with newly diagnosed non-APL AML were randomized using a Bayesian adaptive design to receive either CIA or FAI. All pts received induction with idarubicin 10 mg/m2 IV daily on days 1-3 and cytarabine 1000 mg/m2 IV daily for on days 1-5. Pts in the CIA arm also received clofarabine 15 mg/m2 IV daily on days 1-5; pts in the FAI arm received fludarabine 30 mg/m2 IV daily on days 1-5. Responding pts could receive up to 6 cycles of consolidation with attenuated doses of the same drug combination. The primary endpoint was to compare the event-free survival (EFS) of CIA and FAI. Secondary endpoints included the CR/CRp rates, overall survival (OS) and the safety of the regimens.
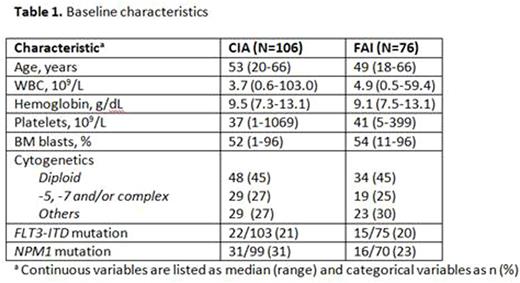
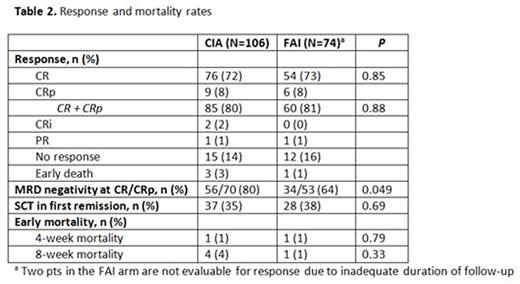
Results: Between 8/2011 and 6/2016, 182 pts have been randomized to receive either CIA (n=106) or FAI (n=76). Baseline characteristics of the 2 arms were well-balanced and are summarized in Table 1. Response rates are summarized in Table 2. Of the 180 pts evaluable for response, the CR/CRp rate was similar in the CIA and FAI arms (80% and 81%, respectively). However, the rate of MRD negativity by multiparameter flow cytometry at the time of CR/CRp was significantly higher in pts who received CIA than in those who received FAI (80% vs. 64%, respectively, P<0.05). Rates of stem cell transplant (SCT) in first remission were similar in the two arms (35% vs. 38%, respectively).
The median duration of follow-up was 27 months. The median EFS and OS for the entire cohort were 12 months and 39 months, respectively. The median EFS was similar in the CIA and FAI arms (13 months and 12 months, respectively, P=0.91). The imbalance in sample size between these two arms was caused by better performance of the CIA arm during the initial period of the trial, although the difference largely disappeared after further follow-up. There was also no difference in OS between the two regimens; the 2-year OS rates were 51% and 57%, respectively (P=0.24). No difference in survival was observed if pts were censored at the time of SCT. Overall, treatment was safe with 8-week mortality rates of 4% in the CIA arm and 1% in the FAI arm.
When compared to a historical cohort of pts treated with idarubicin and cytarabine (IA) alone, the triplet regimen (pooled population of CIA + FAI) resulted in improved EFS and OS among a subgroup of patients <40 years of age. In this group of younger patients, the median EFS for CIA/FAI (n=38) and IA (n=16) were 25 months and 9 months, with a 2-year EFS rate of 52% and 33% respectively (P=0.27). There was also a strong trend towards superior OS in the CIA/FAI compared to the IA groups (median OS: not reached vs. 20 months; 2-year OS rate 68% vs. 47%; P=0.08).
Conclusions: In adult pts with newly diagnosed AML, CIA and FAI resulted in similar rates of CR/CRp and had similar EFS and OS. Compared to a historical cohort of pts treated with IA alone, the addition of a nucleoside analogue appears to result in superior EFS and OS in younger pts.
Cortes:ARIAD: Consultancy, Research Funding; BMS: Consultancy, Research Funding; Novartis: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding; Teva: Research Funding. Daver:Ariad: Research Funding; BMS: Research Funding; Pfizer: Consultancy, Research Funding; Otsuka: Consultancy, Honoraria; Kiromic: Research Funding; Karyopharm: Honoraria, Research Funding; Sunesis: Consultancy, Research Funding. Jain:Novimmune: Consultancy, Honoraria; Infinity: Research Funding; Abbvie: Research Funding; Genentech: Research Funding; Seattle Genetics: Research Funding; Celgene: Research Funding; Servier: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria, Research Funding; BMS: Research Funding; Incyte: Research Funding; Novartis: Consultancy, Honoraria; ADC Therapeutics: Consultancy, Honoraria, Research Funding; Pharmacyclics: Consultancy, Honoraria, Research Funding. Konopleva:Calithera: Research Funding; Cellectis: Research Funding. Wierda:Acerta: Research Funding; Novartis: Research Funding; Gilead: Research Funding; Genentech: Research Funding; Abbvie: Research Funding. DiNardo:Novartis: Other: advisory board, Research Funding; Daiichi Sankyo: Other: advisory board, Research Funding; Agios: Other: advisory board, Research Funding; Abbvie: Research Funding; Celgene: Research Funding. O'Brien:Janssen: Consultancy, Honoraria; Pharmacyclics, LLC, an AbbVie Company: Consultancy, Honoraria, Research Funding. Jabbour:ARIAD: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding; Novartis: Research Funding; BMS: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal