In this issue of Blood, Cooley et al challenge the assumption that the plasma half-life of factor IX (FIX) is a surrogate marker for the duration of hemostatic efficacy in the management of individuals with hemophilia B. They provide evidence that the size of an extravascular pool of FIX bound to collagen IV is the true pharmacodynamic predictor.1
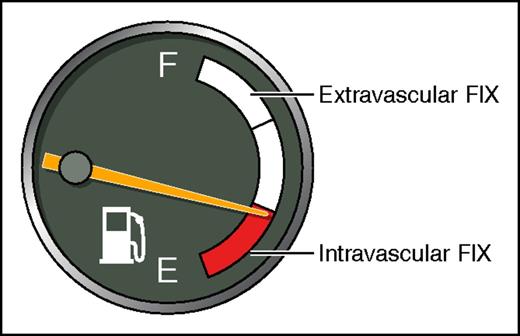
In the conventional view, adequate levels of intravascular FIX (red) are necessary and sufficient for normal hemostasis. Cooley et al propose that two-thirds of total body FIX is in an extravascular compartment bound to collagen IV (white), where it is hemostatically active. Consequently, pharmacokinetic parameters (eg, plasma half-life), which are a mainstay in conventional therapy, are not predictive in their model. Professional illustration by Patrick Lane, ScEYEnce Studios.
In the conventional view, adequate levels of intravascular FIX (red) are necessary and sufficient for normal hemostasis. Cooley et al propose that two-thirds of total body FIX is in an extravascular compartment bound to collagen IV (white), where it is hemostatically active. Consequently, pharmacokinetic parameters (eg, plasma half-life), which are a mainstay in conventional therapy, are not predictive in their model. Professional illustration by Patrick Lane, ScEYEnce Studios.
FIX is a vitamin K–dependent protein that is absent or deficient in hemophilia B. Individuals with hemophilia B are treated with periodic IV infusions of recombinant or plasma-derived FIX on demand to treat bleeding episodes, or prophylactically, to prevent bleeding. Recently, 2 extended half-life FIX products, eftrenonacog alfa (rFIXFc, Alprolix) and albutrepenonacog alfa (rIX-FP, Idelvion), have been approved for use by the US Food and Drug Administration. rFIXFc consists of FIX fused to the Fc region of immunoglobulin G1. Fc fusion proteins bind to the neonatal Fc receptor, which leads to cellular uptake and recycling back into the circulation, thereby prolonging the plasma half-life. The mean terminal plasma half-life of rFIXFc is increased 2.4-fold relative to recombinant human FIX (nonacog alfa, BeneFIX).2 rIX-FP consists of FIX fused to albumin and has a reported 5.3-fold increased plasma half-life by virtue of the relatively long plasma half-life of albumin.3 The differences between the reported improvements in plasma half-lives of these products may be due to differences in the pharmacokinetic methods that were used. Under the assumption that plasma half-life is a surrogate marker for the duration of hemostatic efficacy, these prolonged half-life agents carry the promise of improving the lives of patients with hemophilia B by decreasing the required frequency of infusions of FIX.
Enter Cooley, Stafford, and coworkers. The Stafford group has made seminal contributions to the study of vitamin K–dependent proteins and the pathophysiology of hemophilia B, having produced the widely used hemophilia B mouse4 and cloned, expressed, and characterized the vitamin K–dependent carboxylase and vitamin K epoxide reductase.5,6 Particularly relevant to the current study is the identification by the Stafford group of collagen IV as a FIX ligand that removes FIX from the circulation, producing a large extravascular pool of FIX.7,8 In the current study, they measured the dose-dependent hemostatic efficacy of wild-type FIX (nonacog alfa) and FIXFc using a saphenous vein bleeding model in hemophilia B mice. They found no difference in hemostatic efficacy between the 2 products 7 days after infusion, a time when plasma levels of wild-type FIX were undetectable.
Hemostatic efficacy of the 2 products increased linearly with dose and saturated at ∼150 international units (IU)/kg. The plasma volumes per body mass of humans and mice are similar (∼50 mL/kg). Thus, to produce the normal plasma level of 1 IU/mL, a dose of ∼50 IU/kg is required to fully correct either human or murine hemophilia B plasma. The authors propose that 150 IU/kg was necessary for optimal hemostatic efficacy to saturate a large, hemostatically active, extravascular compartment consisting of FIX bound to collagen IV. They provided evidence for this hypothesis by showing that human K5A FIX, which binds poorly to collagen IV but has normal in vitro clotting activity, demonstrated decreased hemostatic efficacy in the hemophilia B mouse model. They also identified extravascular FIX histochemically in regions of human liver and skeletal muscle that costained with collagen. They noted that their results are consistent with an interesting experiment published nearly 30 years ago by Stern et al.9 In that study, infusion of bovine FIX into baboons produced a large increase in the plasma concentration of baboon FIX, consistent with displacement of a large pool of noncirculating FIX into plasma.
Cooley et al propose that the hemostatically relevant FIX molecule is the one that is bound to extravascular collagen IV, not the one circulating in plasma, because after all, normal hemostasis is an extravascular event. In their view, FIX, like tissue factor, is present in the extravascular space, poised to participate in the early events of hemostasis. This reinterpretation of FIX biology, if correct, has radical implications for the management of individuals with hemophilia B. First, pharmacokinetics does not equal pharmacodynamics. Targeting plasma half-life or other pharmacokinetic parameters of FIX is not an accurate predictor of the duration of hemostatic efficacy. This is consistent with the observation that the authors found no difference in the duration of hemostatic efficacy between wild-type and rFIXFc. Second, the size of the FIX “gas tank,” conventionally taught to be 50 IU/kg, is 3 times larger than that (see figure). Thus, the dose required for full hemostatic efficacy in a true FIX null subject, like the hemophilia B mouse in the current study, is 150 IU/kg. Recent clinical studies indicate that once-weekly prophylaxis of 100 IU/kg is associated with a lower annualized bleeding rate compared with on-demand treatment in individuals with hemophilia B.10 The motivation for this “high-dose” FIX therapy was not to fill an extravascular compartment, but rather to produce hemostatically effective trough levels of plasma FIX. Nonetheless, these studies indicate that high-dose FIX therapy is effective and well tolerated, and, combined with results of the present study, they suggest that 150 IU/kg once weekly may be even better. Some individuals with hemophilia B due to FIX missense mutations may produce hemostatically defective molecules that are produced in normal amounts, bind to collagen IV, and inhibit the binding of wild-type FIX. In this situation, even larger doses of FIX may be required to displace mutant FIX and produce adequate hemostasis.
The results of this study constitute a challenge to clinical investigators. Are “long-acting” FIX products superior to wild-type FIX when the dose and dose frequency of the latter are optimized? If the pharmacokinetic properties of FIX products are an unreliable guide to the duration of hemostatic efficacy, can clinical studies be designed to accurately measure pharmacodynamics?
Conflict-of-interest disclosure: The author declares no competing financial interests.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal