Key Points
rIX-FP maintains mean trough of 20 and 12 IU/dL FIX activity with 40 IU/kg weekly and 75 IU/kg every 2 weeks prophylaxis, respectively.
Weekly and 14-day prophylaxis regimens with rIX-FP were well tolerated and provided low bleeding rates and target joint improvement.
Abstract
A global phase 3 study evaluated the pharmacokinetics, efficacy, and safety of recombinant fusion protein linking coagulation factor IX with albumin (rIX-FP) in 63 previously treated male patients (12-61 years) with severe hemophilia B (factor IX [FIX] activity ≤2%). The study included 2 groups: group 1 patients received routine prophylaxis once every 7 days for 26 weeks, followed by either 7-, 10-, or 14-day prophylaxis regimen for a mean of 50, 38, or 51 weeks, respectively; group 2 patients received on-demand treatment of bleeding episodes for 26 weeks and then switched to a 7-day prophylaxis regimen for a mean of 45 weeks. The mean terminal half-life of rIX-FP was 102 hours, 4.3-fold longer than previous FIX treatment. Patients maintained a mean trough of 20 and 12 IU/dL FIX activity on prophylaxis with rIX-FP 40 IU/kg weekly and 75 IU/kg every 2 weeks, respectively. There was 100% reduction in median annualized spontaneous bleeding rate (AsBR) and 100% resolution of target joints when subjects switched from on-demand to prophylaxis treatment with rIX-FP (P < .0001). The median AsBR was 0.00 for all prophylaxis regimens. Overall, 98.6% of bleeding episodes were treated successfully, including 93.6% that were treated with a single injection. No patient developed an inhibitor, and no safety concerns were identified. These results indicate rIX-FP is safe and effective for preventing and treating bleeding episodes in patients with hemophilia B at dosing regimens of 40 IU/kg weekly and 75 IU/kg every 2 weeks. This trial was registered at www.clinicaltrials.gov as #NCT0101496274.
Introduction
Hemophilia B, particularly moderate and severe forms (≤5% factor IX [FIX] activity), is associated with spontaneous bleeding into joints, muscles, and soft tissues that may lead to crippling arthropathy, and bleeding in the intracranial, neck/throat, or gastrointestinal spaces may be life threatening. The prevention of recurrent bleeding and joint deterioration in order to preserve normal musculoskeletal function is the goal of routine prophylaxis treatment.1 Current prophylaxis therapy requires frequent intravenous injections of FIX replacement product, maintaining appropriate FIX trough levels to effectively reduce the incidence of hemarthroses and other bleeding episodes. Currently available standard half-life FIX replacement products require intravenous injections twice per week.2,3 Recombinant FIX Fc fusion protein (rFIXFc; Alprolix, Biogen/Idec), recently licensed in the United States, has an extended half-life compared with standard FIX products,4 so that time to 3 IU/dL FIX activity is 5.8 days with a dose of 50 IU/kg.5 The necessity of frequent injections creates a burden for both patients and caregivers, impacting long-term compliance.6
Recombinant fusion protein linking recombinant coagulation factor IX with recombinant albumin (rIX-FP) is produced as a single protein with a cleavable linker between FIX and albumin that is derived from the endogenous activation peptide in native FIX. Because albumin is protected from degradation by pH-dependent binding to the neonatal Fc receptor,7,8 rIX-FP has an increased circulating half-life compared with recombinant FIX (rFIX).
rIX-FP has demonstrated improved pharmacokinetics (PK) and prolonged pharmacodynamic activity, when compared with rFIX in preclinical studies9-11 and in earlier clinical trials.12,13 The improved PK profile of rIX-FP may allow patients to be injected less frequently while maintaining a circulating FIX level high enough to minimize the occurrence of spontaneous bleeding episodes.
The aim of this study was to evaluate PK, efficacy, and safety of rIX-FP administered for the treatment and prevention of bleeding episodes in previously treated adolescent and adult patients with severe or moderately severe hemophilia B (FIX activity ≤2 IU/dL). We present the results of a single-sequence crossover study that compared the efficacy of different regimens, including on-demand vs prophylaxis treatment and 7-day vs 14-day prophylaxis regimens, in patients with hemophilia B.
Methods
Study conduct
The study was approved by the institutional review board/ethics committee at each participating center, registered at www.clinicaltrials.gov (#NCT0101496274), and performed in accordance with good clinical practice,14 the Declaration of Helsinki, and local regulatory requirements. Written informed consent was obtained from all patients or their legal guardians.
Study patients
The main criteria for subject selection were based on the Guideline on the Clinical Investigation of Recombinant and Human Plasma-Derived Factor IX Products by the Committee for Medicinal Products for Human Use.15 Male patients, 12 to 65 years of age, with hemophilia B (FIX activity ≤2 IU/dL), at least 150 exposure days (EDs) with previous FIX replacement products, and no detectable inhibitor to FIX or inhibitor history were eligible for enrollment. Patients with a known hypersensitivity to any FIX product or hamster protein or on immunomodulating treatment or having CD4 cell count <200/mm3 were excluded. Patients with serum aspartate aminotransferase or alanine aminotransferase >5 times the upper limit of normal were also excluded. Patients enrolled in the on-demand treatment group had a minimum of 2 nontrauma-induced bleeding episodes treated per month (any type or location), in the 3 to 6 months preceding study entry.
Trial design
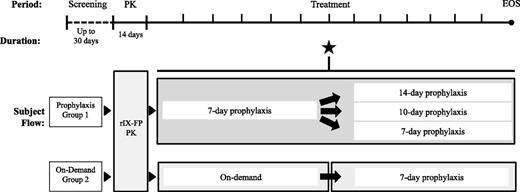
This was a prospective, nonrandomized, multinational, open-label phase 3 study, with patients assigned to either a prophylaxis group 1 (prophylaxis/prophylaxis) or an on-demand group 2 (on-demand/prophylaxis) (Figure 1). Only patients who were previously receiving on-demand treatment were eligible for group 2 assignment. The study consisted of a 1-month screening period to determine eligibility for the study, followed by an active rIX-FP treatment period of at least 12 months. In addition, all subjects who had not previously undergone PK analysis of rIX-FP in a previous study participated in a 14-day PK evaluation of 25 or 50 IU/kg rIX-FP at the start of the study. A subset of patients in group 1 (the first 15 rIX-FP-naïve patients enrolled) underwent both a PK evaluation of their previous FIX product and a second PK evaluation of 50 IU/kg rIX-FP after 26 weeks of 7-day prophylaxis treatment.
Study design. The study consisted of a 1-month screening period, 14-day PK assessment, followed by active treatment of at least 12 months. Patients were assigned to either prophylaxis treatment (group 1) or on-demand treatment (group 2) based on previous treatment regimen. Group 1 patients received weekly prophylaxis for 26 weeks and then were evaluated for eligibility to switch to a longer treatment interval (star). Group 2 received on-demand treatment of the first 26 weeks followed by weekly rIX-FP prophylaxis for an additional 26 weeks or longer. Subjects were required to have no spontaneous bleeds for at least 1 month and be on a stable dose of ≤40 IU/kg or ≤50 IU/kg rIX-FP to switch to a 14-day or 10-day treatment interval, respectively. Subjects continued on 7-, 10-, or 14-day prophylaxis for the remaining treatment period. A subset of subjects in group 1 (the first 15 patients naïve to rIX-FP to enroll) repeated the PK assessment of 50 IU/kg rIX-FP at approximately week 26, prior to switching to a longer treatment interval. EOS, end of study.
Study design. The study consisted of a 1-month screening period, 14-day PK assessment, followed by active treatment of at least 12 months. Patients were assigned to either prophylaxis treatment (group 1) or on-demand treatment (group 2) based on previous treatment regimen. Group 1 patients received weekly prophylaxis for 26 weeks and then were evaluated for eligibility to switch to a longer treatment interval (star). Group 2 received on-demand treatment of the first 26 weeks followed by weekly rIX-FP prophylaxis for an additional 26 weeks or longer. Subjects were required to have no spontaneous bleeds for at least 1 month and be on a stable dose of ≤40 IU/kg or ≤50 IU/kg rIX-FP to switch to a 14-day or 10-day treatment interval, respectively. Subjects continued on 7-, 10-, or 14-day prophylaxis for the remaining treatment period. A subset of subjects in group 1 (the first 15 patients naïve to rIX-FP to enroll) repeated the PK assessment of 50 IU/kg rIX-FP at approximately week 26, prior to switching to a longer treatment interval. EOS, end of study.
Group 1 received rIX-FP once every 7 days as routine prophylaxis during the first 26 weeks with starting dose of 35 to 50 IU/kg rIX-FP, as decided by the treating physician. After 26 weeks, patients were allowed to switch to prophylaxis treatment intervals of 10 or 14 days with 75 IU/kg rIX-FP after meeting the following switching criteria: no spontaneous bleeds for at least 4 weeks before switching and receiving ≤40 IU/kg rIX-FP in order to switch to the 14-day interval or ≤50 IU/kg rIX-FP to switch to the 10-day interval. The dose could be adjusted up or down based on the treating physician’s assessment of bleeding phenotype, physical activity level, or clinical outcome.
Group 2 received on-demand (episodic) treatment with rIX-FP for bleeding episodes during the first 26 weeks followed by 7-day prophylaxis for approximately ≥26 weeks with a fixed dose between 35 and 50 IU/kg, determined by the physician.
All bleeding episodes were treated with rIX-FP, at doses between 35 and 50 IU/kg, as decided by the physician. Patients self-administered rIX-FP for both routine prophylaxis and on-demand treatment of bleeding episodes; all home administrations were recorded in an electronic diary. A second dose of rIX-FP was administered at least 24 hours after the first injection, if needed, to achieve hemostatsis, as determined by the judgment of the patient and/or provider. Efficacy and safety assessments were performed at study sites on a monthly basis. Any patient requiring surgery during the course of the study could participate in a surgical substudy.
The study was considered completed when 50 patients achieved ≥50 EDs in the rIX-FP clinical program, including previous studies. However, the active treatment period for the evaluation of safety and efficacy was extended up to 27 months to allow subjects to receive continuous treatment with rIX-FP until enrollment in the subsequent extension study.
Trial objectives and outcome measures
The primary efficacy objective of the study was to evaluate the efficacy of rIX-FP to prevent bleeding episodes, as assessed by an intraindividual comparison of the annualized spontaneous bleeding rate (AsBR) during 7-day prophylaxis with the AsBR during the on-demand treatment period in group 2. The primary safety objective of the study was to evaluate the safety of rIX-FP, as assessed by the occurrence of inhibitors against FIX in all patients who received dose(s) of rIX-FP.
The secondary objectives of the study were to evaluate the PK, the hemostatic efficacy of rIX-FP for the prevention and treatment of bleeding episodes, and the overall clinical safety of repeated dosing of rIX-FP. The secondary efficacy end points included the annualized bleeding rates (ABRs) in all prophylaxis regimens (once every 7, 10, and 14 days), the number of rIX-FP injections required to achieve hemostasis when treating bleeding episodes, and the investigator’s assessment based on a 4-point scale (see footnote of Table 4 for details). Safety was determined by evaluating the frequency, severity, and relatedness of adverse events (AEs), development of noninhibitory antibodies against rIX-FP and Chinese hamster ovary (CHO) cell proteins, local tolerability, laboratory safety parameters, physical exam, and vital signs.
Analytical methods
FIX activity was measured using a validated 1-stage clotting method using Pathromtin SL (Siemens Healthcare Diagnostics, Marburg, Germany) as an activator reagent; rIX-FP activity determination was performed using the Behring Coagulation System.12 The results were interpreted using a reference curve, prepared from standard human plasma calibrated to the World Health Organization standard for FIX, and reported in International Units. This assay was used to measure FIX activity for PK assessment of both rIX-FP and the patients’ previous FIX product (plasma-derived FIX [pdFIX] or rFIX).
Inhibitors were titrated by the Bethesda method according to the Nijmegen modification,16 and a titer ≥0.6 Bethesda units was defined as a positive result.
A tiered approach to immunogenicity testing for rIX-FP was employed during the study. A direct binding enzyme-linked immunosorbent assay was performed to detect antibodies against rIX-FP; if a positive signal was obtained, the sample was retested to confirm the specific antibody signal and to discriminate between antibodies against rFIX, pdFIX, and albumin. A second enzyme-linked immunosorbent assay was performed to test for antibodies against CHO cell proteins; if a positive signal was obtained, the sample was retested by surface plasmon resonance to confirm the specific antibody signal. All assays were performed in the central laboratory at CSL Behring, Marburg, Germany.
Statistical analysis
The efficacy and safety populations consisted of all patients who received at least 1 dose of rIX-FP. The sample size of the study was based on the recommendations from regulatory agencies because of the rarity of the disease. For the primary safety end point of incidence of anti-FIX inhibitors, a sample size of 50 was considered sufficient to rule out an estimated incidence of inhibitor development of 10.65%. The primary efficacy end point, the AsBR, was analyzed using the Wilcoxon signed-rank test in the primary efficacy population, which consisted of all patients assigned to group 2 who received at least 1 dose of rIX-FP for prophylaxis after completing a 26-week period of on-demand treatment. The null hypothesis was that the ratio of AsBR (prophylaxis/on-demand) was ≥0.50; the test was conducted at the 1-sided 0.025 level. In addition, the estimated AsBR (model-based AsBR) with 95% confidence interval (CI) based on a Poisson distribution was presented for all treatment regimens.
The efficacy of the 10-day and 14-day prophylaxis regimens was determined by comparing the model-based ABR with that obtained in the 7-day prophylaxis regimen. In addition, ABRs were also calculated as matched pairs and compared using a Student t test in patients who received both the 7-day and 14-day prophylaxis regimens for a minimum of 12 weeks each.
Treatment of minor or moderate bleeding episodes was considered successful if hemostasis was achieved with 1 or 2 injections. The proportion of bleeds treated successfully was reported with a 95% CI. In order to consider on demand treatment satisfactorily effective, one would expect to observe that 85% of bleeding episodes are treated with 1 or 2 infusions.17 As an acceptance criterion, therefore, the lower limit of the 2-sided 95% CI was set to exceed 80%.
The PK analysis was performed by standard noncompartmental analysis using Phoenix WinNonlin software version 6.2 (Pharsight). Four main PK parameters (incremental recovery, terminal half-life, area under the curve (AUC), and total body clearance normalized to body weight) were calculated using the actual collection times, according to International Society on Thrombosis and Haemostasis recommendations.18,19
Normally or approximately distributed data are reported as mean and standard deviation (SD); nonnormally distributed data, such as ABR, are reported as median and interquartile range (IQR).
Drug product
rIX-FP was produced by expression in CHO cells and supplied as freeze-dried powder in single-use vials with a nominal content of 500, 1000, or 2000 IU per vial. The 500 and 1000 IU vials were reconstituted with 2.5 mL, and the 2000 IU vial with 5.0 mL of water for intravenous injection.
Results
Patient characteristics
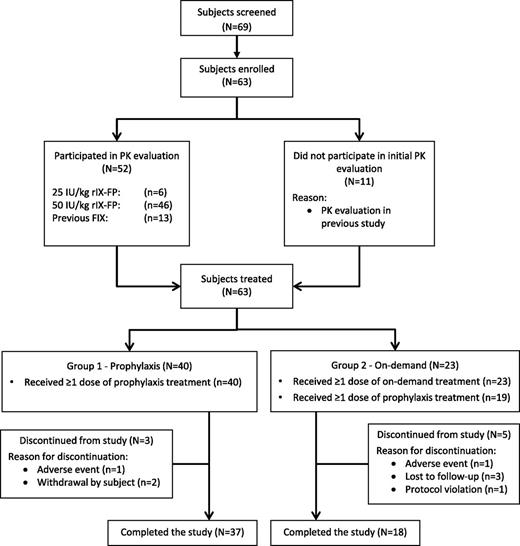
Overall, 63 male patients with hemophilia B (FIX activity ≤2 IU/dL) from 32 sites in 10 countries provided informed consent and were enrolled and treated with rIX-FP between February 2012 and July 2014. Patients were between 12 and 61 years of age (mean 33.0 years); 7 patients were younger than 18 years. The patient population was geographically diverse and included patients from North America, Europe, Asia, and the Middle East (Table 1). More than half of the patients in both groups 1 and 2 reported chronic hemarthrosis or a target joint at the start of the study (see footnote of Table 1 for details20 ). Group 2 patients (on-demand prior to study entry) reported a higher median nontrauma-induced bleeding rate than group 1 patients during the 12 months prior to study entry (21.0 vs 1.0). Patient enrollment and a study flow diagram are presented in Figure 2.
Baseline demographics and patient characteristics
| Characteristics . | Prophylaxis (N = 40) . | On-demand (N = 23) . | Overall (N = 63) . |
|---|---|---|---|
| Age, y | |||
| Mean (SD) | 31.6 (15.2) | 35.3 (11.1) | 33.0 (13.9) |
| Adolescents (12-17 y), n | 7 | 0 | 7 |
| Race, n (%) | |||
| White | 33 (82.5) | 19 (82.6) | 52 (82.5) |
| Asian | 6 (15.0) | 4 (17.4) | 10 (15.9) |
| Black/African American | 1 (2.5) | 0 | 1 (1.6) |
| Weight, kg | |||
| Mean (SD) | 69.6 (14.4) | 75.1 (20.7) | 71.6 (17.0) |
| Geographic location, n (%) | |||
| Asia | 6 (15.0) | 4 (17.4) | 10 (15.9) |
| Europe | 21 (52.5) | 15 (65.2) | 36 (57.1) |
| Middle East | 11 (27.5) | 0 | 11 (17.5) |
| North America | 2 (5.0) | 4 (17.4) | 6 (9.5) |
| Previous treatment regimen | |||
| On-demand | 0 | 23 (100.0) | 23 (36.5) |
| Prophylaxis | 40 (100.0) | 0 | 40 (63.5) |
| Previous FIX product | |||
| rFIX | 20 (50.0) | 7 (30.4)* | 27 (42.8) |
| pdFIX | 9 (22.5) | 12 (52.2) | 21 (33.3) |
| rIX-FP† | 11 (27.5) | 4 (17.4) | 15 (23.8) |
| Classification of hemophilia‡, n(%) | |||
| ≤1 IU/dL | 35 (87.5) | 20 (87.0) | |
| ≤2 IU/dL | 40 (100.0) | 23 (100.0) | 63 (100.0) |
| HIV positive | 7 (17.5) | 5 (21.7) | 12 (19.0) |
| HBV positive | 1 (2.5) | 1 (4.3) | 2 (3.2) |
| HCV positive | 10 (25.0) | 13 (56.5) | 23 (36.5) |
| Chronic hemarthrosis/target joint§, n (%) | 21 (52.5) | 14 (60.9) | 35 (55.6) |
| Total ABR|| | |||
| Mean (SD) | 3.4 (3.8) | 24.3 (7.3) | |
| Median (IQR) | 2.0 (0, 4.5) | 23.5 (22, 28) | |
| Spontaneous ABR|| | |||
| Mean (SD) | 1.5 (2.2) | 16.6 (8.6) | |
| Median (IQR) | 0 (0, 2) | 17.0 (10, 24) | |
| Nontrauma ABR||¶ | |||
| Mean (SD) | 1.7 (2.5) | 18.3 (6.7) | |
| Median (IQR) | 1.0 (0, 2) | 21.0 (12, 24) |
| Characteristics . | Prophylaxis (N = 40) . | On-demand (N = 23) . | Overall (N = 63) . |
|---|---|---|---|
| Age, y | |||
| Mean (SD) | 31.6 (15.2) | 35.3 (11.1) | 33.0 (13.9) |
| Adolescents (12-17 y), n | 7 | 0 | 7 |
| Race, n (%) | |||
| White | 33 (82.5) | 19 (82.6) | 52 (82.5) |
| Asian | 6 (15.0) | 4 (17.4) | 10 (15.9) |
| Black/African American | 1 (2.5) | 0 | 1 (1.6) |
| Weight, kg | |||
| Mean (SD) | 69.6 (14.4) | 75.1 (20.7) | 71.6 (17.0) |
| Geographic location, n (%) | |||
| Asia | 6 (15.0) | 4 (17.4) | 10 (15.9) |
| Europe | 21 (52.5) | 15 (65.2) | 36 (57.1) |
| Middle East | 11 (27.5) | 0 | 11 (17.5) |
| North America | 2 (5.0) | 4 (17.4) | 6 (9.5) |
| Previous treatment regimen | |||
| On-demand | 0 | 23 (100.0) | 23 (36.5) |
| Prophylaxis | 40 (100.0) | 0 | 40 (63.5) |
| Previous FIX product | |||
| rFIX | 20 (50.0) | 7 (30.4)* | 27 (42.8) |
| pdFIX | 9 (22.5) | 12 (52.2) | 21 (33.3) |
| rIX-FP† | 11 (27.5) | 4 (17.4) | 15 (23.8) |
| Classification of hemophilia‡, n(%) | |||
| ≤1 IU/dL | 35 (87.5) | 20 (87.0) | |
| ≤2 IU/dL | 40 (100.0) | 23 (100.0) | 63 (100.0) |
| HIV positive | 7 (17.5) | 5 (21.7) | 12 (19.0) |
| HBV positive | 1 (2.5) | 1 (4.3) | 2 (3.2) |
| HCV positive | 10 (25.0) | 13 (56.5) | 23 (36.5) |
| Chronic hemarthrosis/target joint§, n (%) | 21 (52.5) | 14 (60.9) | 35 (55.6) |
| Total ABR|| | |||
| Mean (SD) | 3.4 (3.8) | 24.3 (7.3) | |
| Median (IQR) | 2.0 (0, 4.5) | 23.5 (22, 28) | |
| Spontaneous ABR|| | |||
| Mean (SD) | 1.5 (2.2) | 16.6 (8.6) | |
| Median (IQR) | 0 (0, 2) | 17.0 (10, 24) | |
| Nontrauma ABR||¶ | |||
| Mean (SD) | 1.7 (2.5) | 18.3 (6.7) | |
| Median (IQR) | 1.0 (0, 2) | 21.0 (12, 24) |
HBV, hepatitis B virus; HCV, hepatitis C virus.
Includes 1 subject previously on an investigational rFIX product.
Patients previously enrolled in phase 2 study with rIX-FP.13
FIX activity level (IU/dL) as recorded in subject medical records or measured at screening. All subjects had FIX activity ≤2 IU/dL in order to be eligible for the study.
Percentages are based on the number of patients with chronic hemarthrosis in at least 1 major joint (ankle, knee, or elbow) or a target joint, defined as at least 3 spontaneous bleeding episodes in the same joint in a 6-month period.20
Bleeding episodes in the 12 months prior to study entry.
Nontrauma defined as spontaneous and unknown cause bleeding episodes.
Patient enrollment and study flow diagram. The diagram shows the flow and disposition of patients in the trial. Following screening, 63 subjects were enrolled in the study. All subjects who had not previously undergone PK analysis of rIX-FP in a previous study participated in PK evaluation of 25 IU/kg (n = 6) or 50 IU/kg rIX-FP (n = 46). A subset of subjects (n = 13) also participated in a PK evaluation of their previous FIX product (pdFIX or rFIX). A subset of subjects (n = 15) repeated PK analysis of 50 IU/kg rIX-FP at approximately week 26. Subjects were assigned either weekly prophylaxis (group 1) or on-demand treatment (group 2) with rIX-FP, based on their prior treatment regimen. Eight subjects discontinued from the study for the following reasons: AEs (n = 2), subject decision (n = 2), lost to follow-up (n = 3), and protocol violation (n = 1, unwillingness to switch to prophylaxis after on-demand treatment).
Patient enrollment and study flow diagram. The diagram shows the flow and disposition of patients in the trial. Following screening, 63 subjects were enrolled in the study. All subjects who had not previously undergone PK analysis of rIX-FP in a previous study participated in PK evaluation of 25 IU/kg (n = 6) or 50 IU/kg rIX-FP (n = 46). A subset of subjects (n = 13) also participated in a PK evaluation of their previous FIX product (pdFIX or rFIX). A subset of subjects (n = 15) repeated PK analysis of 50 IU/kg rIX-FP at approximately week 26. Subjects were assigned either weekly prophylaxis (group 1) or on-demand treatment (group 2) with rIX-FP, based on their prior treatment regimen. Eight subjects discontinued from the study for the following reasons: AEs (n = 2), subject decision (n = 2), lost to follow-up (n = 3), and protocol violation (n = 1, unwillingness to switch to prophylaxis after on-demand treatment).
PK
All patients who had not been enrolled in a previous study of rIX-FP participated in a PK assessment at the start of the study, and a subset of patients participated in repeat PK assessment after 26 weeks of prophylaxis treatment. Overall, rIX-FP demonstrated an improved PK profile compared with standard FIX products, with an incremental recovery of 1.27 (IU/dL)/(IU/kg), half-life of 101.7 hours, AUC of 7176 h × IU/dL and clearance of 0.769 mL/h per kg, similar to that previously reported.12 After repeat dosing, PK results of 50 IU/kg rIX-FP were similar to initial results and did not show time dependence or accumulation.
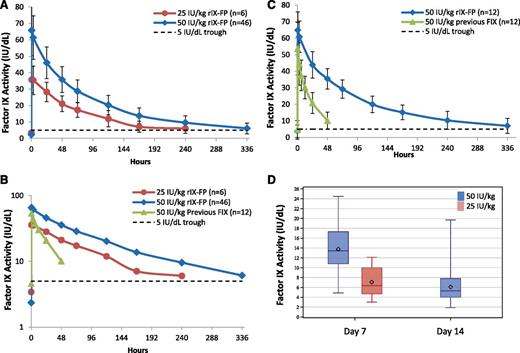
After administration of a single intravenous dose of rIX-FP, mean FIX activity remained >5 IU/dL through day 10 following a dose of 25 IU/kg and through day 14 following a dose of 50 IU/kg (Figure 3).
FIX activity after injection of a single dose of rIX-FP or previous FIX product (PK population). Mean baseline-uncorrected plasma FIX activity after administration of a single infusion of 25 or 50 IU/kg of rIX-FP or 50 IU/kg previous FIX product (pdFIX or rFIX). Linear (A) and semilog (B) plots of rIX-FP over time. (C) Matched-pair plot patients who participated in both 50 IU/kg rIX-FP and 50 IU/kg previous FIX product. FIX activity was measured in international units per deciliter. Vertical bars represent SD. A horizontal dotted line represents the 5 IU/dL FIX activity level. (D) Box plot of FIX activity of rIX-FP at day 7 and day 14; the bar within the box represents the median, diamond represents the mean, the ends of the box are the IQR, and whiskers represent minimum and maximum values. FIX activity levels are not available for a dose of 25 IU/kg rIX-FP at day 14.
FIX activity after injection of a single dose of rIX-FP or previous FIX product (PK population). Mean baseline-uncorrected plasma FIX activity after administration of a single infusion of 25 or 50 IU/kg of rIX-FP or 50 IU/kg previous FIX product (pdFIX or rFIX). Linear (A) and semilog (B) plots of rIX-FP over time. (C) Matched-pair plot patients who participated in both 50 IU/kg rIX-FP and 50 IU/kg previous FIX product. FIX activity was measured in international units per deciliter. Vertical bars represent SD. A horizontal dotted line represents the 5 IU/dL FIX activity level. (D) Box plot of FIX activity of rIX-FP at day 7 and day 14; the bar within the box represents the median, diamond represents the mean, the ends of the box are the IQR, and whiskers represent minimum and maximum values. FIX activity levels are not available for a dose of 25 IU/kg rIX-FP at day 14.
Efficacy
Once weekly prophylaxis after switching from on-demand treatment with rIX-FP.
The primary analysis was performed on the primary efficacy population (n = 19), which included group 2 patients who received rIX-FP on-demand treatment during the first 26 weeks (median, 26.7; IQR, 26.0-27.4 weeks) and then switched to a once weekly prophylaxis regimen for the remaining weeks on study (median, 45.1; IQR, 17.3-74 weeks). The AsBR was significantly reduced following prophylaxis treatment with rIX-FP compared with on-demand treatment (median AsBR of 0.00 and 15.43, respectively; P < .0001; Table 2). The median rIX-FP dose during the once weekly prophylaxis regimen was 40.3 IU/kg (IQR, 37.6-50.6). Overall, there was a 100% reduction in AsBR and 90% reduction in total ABR for patients switching from on-demand to weekly prophylaxis with rIX-FP.
ABRs of group 2 switching from on-demand treatment to once weekly prophylaxis with rIX-FP
| . | On-demand regimen (N = 19) . | Prophylaxis regimen (N = 19) . | Prophylaxis/on-demand . |
|---|---|---|---|
| Number of subjects with at least 1 spontaneous bleeding episode, n (%) | 19 (100.0) | 9 (47.4) | |
| AsBR* | |||
| Median (IQR) | 15.43 (7.98, 17.96) | 0.00 (0.00, 0.96) | |
| Estimated rate (95% CI)† | 13.62 (11.001, 16.868) | 0.55 (0.233, 1.322) | 0.04 (0.019, 0.089) |
| Reduction in AsBR with prophylaxis treatment (%) | |||
| Median (IQR) | 100.00 (90.53, 100.00) | ||
| P‡ | <.0001 | ||
| Total ABR* | |||
| Median (IQR) | 19.22 (16.70, 25.84) | 1.58 (0.00, 4.06) | |
| Estimated rate (95% CI)† | 20.09 (16.808, 24.003) | 2.22 (0.942, 5.243) | 0.11 (0.051, 0.238) |
| Reduction in total ABR with prophylaxis treatment (%) | |||
| Median (IQR) | 90.94 (81.19, 100.00) | ||
| P‡ | <.0001 |
| . | On-demand regimen (N = 19) . | Prophylaxis regimen (N = 19) . | Prophylaxis/on-demand . |
|---|---|---|---|
| Number of subjects with at least 1 spontaneous bleeding episode, n (%) | 19 (100.0) | 9 (47.4) | |
| AsBR* | |||
| Median (IQR) | 15.43 (7.98, 17.96) | 0.00 (0.00, 0.96) | |
| Estimated rate (95% CI)† | 13.62 (11.001, 16.868) | 0.55 (0.233, 1.322) | 0.04 (0.019, 0.089) |
| Reduction in AsBR with prophylaxis treatment (%) | |||
| Median (IQR) | 100.00 (90.53, 100.00) | ||
| P‡ | <.0001 | ||
| Total ABR* | |||
| Median (IQR) | 19.22 (16.70, 25.84) | 1.58 (0.00, 4.06) | |
| Estimated rate (95% CI)† | 20.09 (16.808, 24.003) | 2.22 (0.942, 5.243) | 0.11 (0.051, 0.238) |
| Reduction in total ABR with prophylaxis treatment (%) | |||
| Median (IQR) | 90.94 (81.19, 100.00) | ||
| P‡ | <.0001 |
The median rIX-FP dose during the once weekly prophylaxis regimen was 40.3 IU/kg (IQR, 37.6-50.6).
The ABR was defined as: 365.25 × (number of bleeding episodes)/(number of days in the observed treatment period of interest).
The estimated rate was calculated assuming a Poisson distribution.
P values are based on Wilcoxon Signed-rank test, with a hypothesis of H0: AsBR ratio (prophylaxis/on-demand) ≥0.50.
Group 2 patients showed a slight decrease in total ABR (median, 19.2; Table 2) during on-demand treatment with rIX-FP as compared with the rate reported in the 12 months prior to study entry (median, 23.5; Table 1); nontrauma ABR decreased from a median of 21 (IQR, 12-24; Table 1) to 13.3 (IQR, 7.7-17), respectively. There were 14 patients who reported chronic hemarthrosis or at least 1 target joint at screening (Table 1), and target joints were observed in 10 patients during the on-demand treatment period in the study. After switching to the once weekly prophylaxis regimen, target joints were resolved in all 10 patients: 7 patients had no joint bleeds, and 3 patients had only a single bleeding episode in the previously affected joints.
Prophylaxis regimens every 10 or 14 days after switching from once weekly schedule.
After completing at least 26 weeks on 7-day prophylaxis with a median dose of 40 IU/kg rIX-FP, 28 (70%) patients met the switching criteria (Figure 1) and switched to the 14-day prophylaxis regimen with 75 IU/kg (21 patients) or to the 10-day regimen with 75 IU/kg (7 patients). The median AsBR was 0.00 for all prophylaxis regimens tested in group 1, and the estimated mean AsBR was 0.83, 0.56, and 0.65 in the 14-, 10-, and 7-day prophylaxis regimens, respectively (Table 3). Results for total ABR and joint ABR were similar across treatment regimens, as shown in Table 3. An intraindividual comparison of AsBR between the 7- and 14-day regimens showed that the 14-day regimen was noninferior to the 7-day regimen, with a mean difference of −0.79 (95% CI, −1.780 to 0.197).
ABRs of 7-, 10-, and 14-d prophylaxis regimens
| . | Prophylaxis (group 1) across-treatment regimens . | Prophylaxis (group 1)* within-subject comparison . | ||||
|---|---|---|---|---|---|---|
| 7-d Regimen (N = 40) . | 10-d Regimen (N = 7) . | 14-d Regimen (N = 21) . | 7-d Regimen (N = 21) . | 14-d Regimen (N = 21) . | 7-d vs 14-d Regimen . | |
| AsBR | ||||||
| Median (IQR) | 0 (0, 0) | 0 (0, 0) | 0 (0, 1.0) | 0 (0, 0) | 0 (0, 1.0) | |
| Estimated rate† | 0.65 | 0.56 | 0.83 | 0.29 | 0.83 | 0.35 |
| 95% CI† | 0.37, 1.13 | 0.27, 1.17 | 0.38, 1.77 | 0.068, 1.198 | 0.385, 1.771 | 0.076, 1.575 |
| Mean difference (95% CI)‡ | −0.79 (−1.780, 0.197) | |||||
| Total ABR | ||||||
| Median (IQR) | 0 (0, 1.87) | 0 (0, 1.78) | 1.08 (0, 2.7) | 0 (0, 1.53) | 1.08 (0, 2.70) | |
| Estimated rate† | 1.58 | 1.69 | 1.61 | 0.69 | 1.61 | 0.43 |
| 95% CI† | 1.02, 2.44 | 0.87, 3.28 | 0.93, 2.80 | 0.296, 1.626 | 0.930, 2.801 | 0.162, 1.138 |
| Mean difference (95% CI)‡ | −1.25 (−2.562, 0.070) | |||||
| Joint ABR | ||||||
| Median (IQR) | 0 (0, 1.53) | 0 (0, 0.88) | 0 (0, 1.04) | 0 (0, 0) | 0 (0, 1.04) | |
| Estimated rate† | 1.13 | 0.92 | 1.11 | 0.41 | 1.11 | 0.36 |
| 95% CI† | 0.70, 1.84 | 0.41, 2.04 | 0.51, 2.41 | 0.141, 1.161 | 0.513, 2.414 | 0.111, 1.199 |
| Mean difference (95% CI)‡ | −0.97 (−2.197, 0.249) | |||||
| Treatment duration, wk | ||||||
| Median (IQR) | 38.4 (30.0, 82.3) | 34.3 (21.3, 58.6) | 55.1 (37.0, 63.6) | |||
| . | Prophylaxis (group 1) across-treatment regimens . | Prophylaxis (group 1)* within-subject comparison . | ||||
|---|---|---|---|---|---|---|
| 7-d Regimen (N = 40) . | 10-d Regimen (N = 7) . | 14-d Regimen (N = 21) . | 7-d Regimen (N = 21) . | 14-d Regimen (N = 21) . | 7-d vs 14-d Regimen . | |
| AsBR | ||||||
| Median (IQR) | 0 (0, 0) | 0 (0, 0) | 0 (0, 1.0) | 0 (0, 0) | 0 (0, 1.0) | |
| Estimated rate† | 0.65 | 0.56 | 0.83 | 0.29 | 0.83 | 0.35 |
| 95% CI† | 0.37, 1.13 | 0.27, 1.17 | 0.38, 1.77 | 0.068, 1.198 | 0.385, 1.771 | 0.076, 1.575 |
| Mean difference (95% CI)‡ | −0.79 (−1.780, 0.197) | |||||
| Total ABR | ||||||
| Median (IQR) | 0 (0, 1.87) | 0 (0, 1.78) | 1.08 (0, 2.7) | 0 (0, 1.53) | 1.08 (0, 2.70) | |
| Estimated rate† | 1.58 | 1.69 | 1.61 | 0.69 | 1.61 | 0.43 |
| 95% CI† | 1.02, 2.44 | 0.87, 3.28 | 0.93, 2.80 | 0.296, 1.626 | 0.930, 2.801 | 0.162, 1.138 |
| Mean difference (95% CI)‡ | −1.25 (−2.562, 0.070) | |||||
| Joint ABR | ||||||
| Median (IQR) | 0 (0, 1.53) | 0 (0, 0.88) | 0 (0, 1.04) | 0 (0, 0) | 0 (0, 1.04) | |
| Estimated rate† | 1.13 | 0.92 | 1.11 | 0.41 | 1.11 | 0.36 |
| 95% CI† | 0.70, 1.84 | 0.41, 2.04 | 0.51, 2.41 | 0.141, 1.161 | 0.513, 2.414 | 0.111, 1.199 |
| Mean difference (95% CI)‡ | −0.97 (−2.197, 0.249) | |||||
| Treatment duration, wk | ||||||
| Median (IQR) | 38.4 (30.0, 82.3) | 34.3 (21.3, 58.6) | 55.1 (37.0, 63.6) | |||
The median assigned doses for the 7-, 10-, and 14-d prophylaxis regimens were 40, 75, and 75 IU/kg, respectively.
Includes subjects with a minimum of 12 wk of treatment on both 7-d and 14-d prophylaxis.
The estimated rate was calculated assuming a Poisson distribution.
95% CI based on Student t test from matched pairs design.
FIX trough levels and rIX-FP consumption during prophylaxis regimens.
At day 7 during once weekly prophylaxis with 40 IU/kg and day 14 during 14-day prophylaxis with 75 IU/kg, the mean trough FIX activity was 20.0 IU/dL (IQR, 17-26 IU/dL; range, 2.5-36.2 IU/dL) and 12.4 IU/dL (IQR, 10-14 IU/dL; range, 3.1-25.4 IU/dL), respectively. Patients receiving 14-day and 7-day prophylaxis with rIX-FP had a median consumption of 162.3 IU/kg per month (IQR, 158.6-164.2) and 194.7 IU/kg per month (IQR, 167.4-215.0), respectively. Prior to study entry, the median consumption on prophylaxis with standard FIX products was 256.6 IU/kg per month (IQR, 208.7-365.3).
Treatment of bleeding episodes.
A total of 358 bleeding episodes were treated with rIX-FP; 93.6% and 98.6% of these episodes were successfully treated with 1 or ≤2 infusions of rIX-FP, respectively (Table 4). The probability of success, defined as requiring ≤2 infusions to achieve hemostasis, was 98.6% (95% CI, 96.2-99.5). Patients redosed if needed, at a mean of 49 hours following the first infusion (IQR, 31-65 hours), based on the clinical judgment of patient or physician. Similar treatment efficacy was observed in patients receiving prophylaxis and on-demand treatment, regardless of the cause (spontaneous, trauma induced, or unknown) or location (joint, muscle, or other) of the bleeding episodes. Hemostatic efficacy of rIX-FP in the treatment of bleeding episodes was rated by investigators as excellent or good for 94.1% of bleeding episodes. There were no life-threatening bleeding episodes during the study. The majority of total and spontaneous bleeding episodes (58.7% and 66.2%, respectively) occurred in the elbow, knee, and ankle joints. There were 5 iliopsoas bleeds in 4 patients; 80% were successfully treated with 1 infusion.
Summary of bleeding episodes and hemostatic response to rIX-FP
| . | Prophylaxis (group 1) . | On-demand (group 2) . | Overall . | |
|---|---|---|---|---|
| On-demand regimen . | Prophylaxis regimen . | |||
| Number of patients | 40 | 23 | 19 | 63 |
| Number of patients with bleeding episodes requiring treatment | 30 | 23 | 11 | 53 |
| Number of bleeding episodes requiring treatment | 101 | 220 | 37 | 358 |
| Type of bleeding episode, n (%) | ||||
| Spontaneous | 48 (47.5) | 145 (65.9) | 11 (29.7) | 204 (57.0) |
| Traumatic | 48 (47.5) | 67 (30.5) | 25 (67.6) | 140 (39.1) |
| Postsurgery | 0 | 0 | 0 | 0 |
| Unknown | 5 (5.0) | 8 (3.6) | 1 (2.7) | 14 (3.9) |
| Injections to treat a bleeding episode, n (%) | ||||
| 1 Injection | 93 (92.1) | 208 (94.5) | 34 (91.9) | 335 (93.6) |
| 2 Injections | 8 (7.9) | 9 (4.1) | 1 (2.7) | 18 (5.0) |
| >2 Injections | 0 | 3 (1.4) | 2 (5.4) | 5 (1.4) |
| 1 or 2 Injections | 101 (100.0) | 217 (98.6) | 35 (94.6) | 353 (98.6) |
| Probability of success* | NC | 98.6 | 94.6 | 98.6 |
| 95% CI for probability of success | NC | (94.3, 99.7) | (76.9, 98.9) | (96.2, 99.5) |
| . | Prophylaxis (group 1) . | On-demand (group 2) . | Overall . | |
|---|---|---|---|---|
| On-demand regimen . | Prophylaxis regimen . | |||
| Number of patients | 40 | 23 | 19 | 63 |
| Number of patients with bleeding episodes requiring treatment | 30 | 23 | 11 | 53 |
| Number of bleeding episodes requiring treatment | 101 | 220 | 37 | 358 |
| Type of bleeding episode, n (%) | ||||
| Spontaneous | 48 (47.5) | 145 (65.9) | 11 (29.7) | 204 (57.0) |
| Traumatic | 48 (47.5) | 67 (30.5) | 25 (67.6) | 140 (39.1) |
| Postsurgery | 0 | 0 | 0 | 0 |
| Unknown | 5 (5.0) | 8 (3.6) | 1 (2.7) | 14 (3.9) |
| Injections to treat a bleeding episode, n (%) | ||||
| 1 Injection | 93 (92.1) | 208 (94.5) | 34 (91.9) | 335 (93.6) |
| 2 Injections | 8 (7.9) | 9 (4.1) | 1 (2.7) | 18 (5.0) |
| >2 Injections | 0 | 3 (1.4) | 2 (5.4) | 5 (1.4) |
| 1 or 2 Injections | 101 (100.0) | 217 (98.6) | 35 (94.6) | 353 (98.6) |
| Probability of success* | NC | 98.6 | 94.6 | 98.6 |
| 95% CI for probability of success | NC | (94.3, 99.7) | (76.9, 98.9) | (96.2, 99.5) |
| . | Prophylaxis (group 1) . | On-demand (group 2) . | Overall (N = 63) . | |
|---|---|---|---|---|
| Number of bleeding episodes requiring treatment | 101 | 257 | 358 | |
| Hemostatic response,†n (%) | ||||
| Excellent | 72 (71.3) | 225 (87.5) | 297 (83.0) | |
| Good | 21 (20.8) | 19 (7.4) | 40 (11.2) | |
| Moderate | 3 (3.0) | 6 (2.3) | 9 (2.5) | |
| Poor/no response | 0 | 1 (0.4) | 1 (0.3) | |
| Missing | 5 (5.0) | 6 (2.3) | 11 (3.1) | |
| . | Prophylaxis (group 1) . | On-demand (group 2) . | Overall (N = 63) . | |
|---|---|---|---|---|
| Number of bleeding episodes requiring treatment | 101 | 257 | 358 | |
| Hemostatic response,†n (%) | ||||
| Excellent | 72 (71.3) | 225 (87.5) | 297 (83.0) | |
| Good | 21 (20.8) | 19 (7.4) | 40 (11.2) | |
| Moderate | 3 (3.0) | 6 (2.3) | 9 (2.5) | |
| Poor/no response | 0 | 1 (0.4) | 1 (0.3) | |
| Missing | 5 (5.0) | 6 (2.3) | 11 (3.1) | |
A second dose of rIX-FP was administered at least 24 h after the first injection, if needed, to achieve hemostatsis, as determined by the judgment of the patient and/ or provider.
NC, not calculated.
Probability of success is derived from a repeated measures model (expressed as percentages) and is defined as the probability of achieving hemostasis with 1 or 2 infusions.
Hemostatic response was evaluated by the physician. Definitions of hemostatic response: excellent, pain relief and/or unequivocal improvement in objective signs of bleeding at ∼24 h after the first infusion and no additional infusions required in order to achieve hemostasis; good, definite pain relief and/or improvement in signs of bleeding at ∼24 h after the first infusion but required a second infusion in order to achieve hemostasis; moderate, probable or slight beneficial effect at ∼24 h after the first infusion and required >2 infusions to achieve hemostasis; poor/no response, no improvement or worsened at ∼24 h after the first infusion and additional hemostatic intervention required with other FIX product or plasma to achieve hemostasis.
Safety
There were 3907 injections of rIX-FP during the study with a mean of 64.8 EDs per patient (72.4 in group 1 and 51.5 in group 2). No inhibitors against FIX were detected in any patient receiving rIX-FP; thus the primary safety objective was successfully achieved. No nonneutralizing antibodies against rIX-FP or CHO host cell proteins were detected.
A total of 347 treatment-emergent AEs were reported in 54 (85.7%) patients. Most treatment-emergent AEs were of mild or moderate severity (283 mild, 59 moderate, 5 severe). The most frequently reported treatment-emergent AEs were nasopharyngitis (38 events in 16 [25.4%] patients), headache (34 events in 15 [23.8%] patients), arthralgia (19 events in 9 [14.3%] patients), and influenza (10 events in 7 [11.1%] patients). Eleven AEs (all mild or moderate in severity) in 5 (7.9%) patients were considered by the physician to be possibly related to rIX-FP. Two patients chose to discontinue treatment after experiencing an AE (1 with hypersensitivity, 1 with headache). The AE of hypersensitivity was considered likely to be an infusion-related reaction with nausea, mild palpitation, and dysgeusia. The patient’s heart rate slightly increased from 51 to 60 bpm, and blood pressure was stable (134/78 mmHg). All symptoms resolved within 23 minutes without treatment. The patient decided to withdraw from the study and had no detectable inhibitors to FIX 1 month after the last dose of rIX-FP. The AE of headache was reported as moderate in severity and resolved the same day without treatment.
There were a total of 28 (0.7%) injection site reactions reported by 12 patients. Two (3.2%) patients reported serious AEs: 1 patient was hospitalized for treatment of synovitis according to local practice, and 1 patient with a history of epilepsy following head trauma was hospitalized for treatment of an episode of acquired epileptic aphasia, which resolved as expected. Both severe AEs were considered by the treating physician to be unrelated to rIX-FP. There were no reports of thromboembolic events, anaphylaxis, or life-threatening AEs.
Discussion
Results from this prospective phase 3 study demonstrate that rIX-FP is a safe and effective FIX replacement product with an improved PK profile as compared with standard FIX products, supporting a prophylaxis dosing interval up to 14 days while maintaining FIX trough levels above the target of 1 IU/dL commonly recommended for prophylaxis.2
rIX-FP regimens were highly effective in bleeding prevention, as demonstrated by the achievement of a median AsBR of 0.0 across all prophylaxis regimens. The 7-day regimen with 40 IU/kg and the 14-day regimen with 75 IU/kg resulted in similarly low total ABR and AsBR, indicating that rIX-FP given once every 14 days represents an effective and convenient prophylactic option. In addition, overall consumption of rIX-FP for prophylaxis was ∼40% lower than the previous product used prior to study entry. Indeed, the efficacy of rIX-FP over longer treatment intervals translates to a reduced number of injections for patients compared with currently available rFIX and pdFIX products, with a reduction in consumption. Therefore, routine prophylaxis with rIX-FP may reduce the burden of disease management for patients, caregivers, and health care providers.
The efficacy of prophylaxis treatment compared with on-demand treatment was demonstrated by a within-subject comparison of the 2 rIX-FP regimens; this study design controlled for the variability of bleeding frequency within the hemophilia B patient population, as group 2 patients started rIX-FP treatment on-demand and continued on 7-day prophylaxis with a median dose of 40 IU/kg rIX-FP. A drastic reduction of the median AsBR to 0.0 while on 7-day prophylaxis was observed, and, in addition, all target joints resolved in these patients after switching to 7-day prophylaxis regimen.
Measures of hemostatic efficacy indicated that rIX-FP provides rapid and complete control of bleeding episodes, with a success rate of 98.6%. In particular, 93.6% of bleeds were controlled with 1 infusion, which compares favorably to results reported for both pdFIX and rFIX products, including extended half-life FIX products.3,4,21,22
It is intriguing to note that a slight decrease of ABR was observed in group 2 patients during on-demand treatment with rIX-FP as compared with the ABR in the 12-month period preceding study entry. This finding raises the possibility that on-demand treatment with rIX-FP might provide, to a certain extent, some protection against a subsequent bleeding episode. Therefore, patients with a severe bleeding phenotype treated on-demand might experience fewer bleeding episodes if switched to rIX-FP. Furthermore, such on-demand patients who require >1 infusion per month may have the benefit of a reduction of ABR by administering a similar number of infusions according to a 14-day prophylaxis regimen with rIX-FP. This observation may have been affected by the small sample size and differences of care received by patients while on a clinical study; further data are needed to understand if rIX-FP can lower the ABR of patients receiving only on-demand treatment.
The median rIX-FP doses of 40 IU/kg for 7-day and 75 IU/kg for 14-day prophylaxis regimens provided FIX activity troughs of 20.0 IU/dL and 12.4 IU/dL, respectively. Although not tested in this trial, a 7-day prophylaxis regimen of 25 IU/kg and a 14-day prophylaxis regimen of 50 IU/kg are supported by current and previous PK results with rIX-FP,12,13,23 and should allow patients with severe and moderate hemophilia B to experience the benefit of a mild bleeding phenotype.
rIX-FP demonstrated improved PK parameters over all marketed FIX products3,4,24 with an extended terminal half-life of 102 hours. Other PK parameters, such as AUC (7176 h × IU/dL), clearance (0.77 mL/h per kg), and incremental recovery (1.27 IU/dL per IU/kg) are improved as well. Mean FIX activity was >5 IU/dL at day 7 and day 14 following a single dose of 25 or 50 IU/kg rIX-FP, respectively. Although no statistical comparisons have been performed, rFIXFc has reported a faster clearance of 3.304 mL/h per kg, and reached 3 IU/dL FIX activity 5.8 days after administration.5 The median AsBR of 7-day prophylaxis with rIX-FP (median dose 40 IU/kg) was 0.00, lower than the reported AsBR of 1.04 with weekly prophylaxis with rFIXFc (median dose 45.2 IU/kg).4,5 A direct comparison of the efficacy of prophylaxis with rIX-FP and rFIXFc is difficult because of the differences in patient population, study design, and prophylaxis regimens between these trials; however, these findings suggest that a slower clearance may be a factor in the success of prophylaxis regimens rather than half-life alone.
FIX activity levels play a key role in preventing bleeding. Den Uijl et al25 showed that joint bleeding occurs in a relevant proportion of hemophilia A patients with factor levels up to 12 IU/dL. Although no hemophilia B patients were included in that study, it suggests that FIX levels required to prevent bleeding may be higher than currently targeted with standard prophylaxis regimens. Patients on prophylaxis with standard FIX products administered 2 times per week may have an increased risk of bleeding when FIX activity is low, particularly prior to the next scheduled prophylaxis dose. In contrast, the improved PK parameters of rIX-FP offer higher FIX activity for longer durations, reducing the risk of both spontaneous and trauma-related bleeding episodes, in addition to offering a less frequent dosing schedule and potential improvements in adherence.26
In conclusion, rIX-FP is safe and effective in preventing and treating bleeding episodes in previously treated adolescents and adults with hemophilia B. The enhanced PK profile allows for a paradigm shift of routine prophylaxis regimen at dosing intervals of up to 14 days. With a half-life of >100 hours, five- to sevenfold better clearance, and AUC and higher incremental recovery than standard FIX products, rIX-FP will provide prolonged hemostatic coverage. A study is currently underway to evaluate the efficacy of a 21-day prophylaxis regimen with a dose of 100 IU/kg rIX-FP.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank the following individuals for their contributions to the conduct of the trial at the investigative sites: Chantal Rothschild, Thierry Lambert, Reinhard Schneppenheim, Günter Auerswald, Christine Heller, Annarita Tagliaferri, Maria Elisa Mancuso, Aaron Lubetsky, Katsuyuki Fukutake, Masashi Taki, Keiji Nogami, Michio Sakai, Tatiana Chernova, Maria Fernanda López Fernández, Joan C. Gill, Amy Shapiro, and Patrick Fogarty. The authors also thank all the patients and their families who contributed to this study, all the participating research nurses and data coordinators, and the Independent Data Monitoring Committee members: Barbara Konkle (Pugent Sound Blood Center, Seattle, WA), (chairperson) Mike Makris (Royal Hallamshire Hospital, Sheffield, United Kingdom), and Nigel Key (University of North Carolina, Chapel Hill, NC). The authors thank Annette Feussner (CSL Behring/Germany) for central laboratory testing support, Christine Joch and Denise Wolko (CSL Behring/Germany) for data analysis, Grace Cole and Cindy Cochran (CSL Behring/United States) for operational management, Yanyan Li (CSL Behring/United States) for statistical support, and Tharin Limsakun (CSL Behring/United States) for PK review.
This study was sponsored by CSL Behring, Marburg, Germany. The sponsor was responsible for trial operations, including data analysis.
Authorship
Contribution: E.S., U.M., T.L., B.P.-P., H.H., J.O., L.B., C.N., I.P., M.v.D.P., C.A., G.C., K.Y., and M.-T.Á.-R. were principal investigators for the trial; I.J. and C.V. were involved in the design of the trial protocol and authored the manuscript; N.B. was responsible for statistical analysis; and all authors contributed to the interpretation of results and preparation and review of the manuscript
Conflict-of-interest disclosure: E.S., U.M., T.L., B.P.-P., H.H., J.O., L.B., C.N., I.P., M.v.D.P., C.A., G.C., K.Y., and M.-T.Á.-R. received research support from CSL Behring to conduct the study. E.S. received honoraria for speaking and/or for consulting from CSL Behring, Bayer, Baxter/Baxalta, Pfizer, Novo Nordisk, Roche, Sobi/Biogen Idec, Biotest, Kedrion, Octapharma, and Grifols and received unrestricted research grants from Novo Nordisk and Pfizer. H.H. has received honoraria from Baxter, Novo Nordisk, Bayer, Pfizer, Biogen, and Kaketsuken and has served on advisory boards for Baxter, Novo Nordisk, Kaketsuken, and Biogen. J.O. received reimbursement for attending symposia/congresses and/or honoraria for speaking and/or honoraria for consulting and/or funds for research from Baxter, Bayer, Biogen Idec, Biotest, Chugai, CSL-Behring, Grifols, Novo Nordisk, Octapharma, Pfizer, Roche, and Swedish Orphan Biovitrum. The home institution of I.P. received an unrestricted research grant from CSL Behring, and I.P. received fees as speaker and chair in meetings organized by CSL Behring. G.C. has served on advisory boards for Bayer, Baxter, CSL Behring, Pfizer, Kedrion, Novo Nordisk, and Sobi. C.V., N.B., and I.J. were employed at CSL Behring.
A complete list of the members of the PROLONG-9FP Investigators Study Group appears in the supplemental Appendix (available on the Blood Web site).
Correspondence: Elena Santagostino, Angelo Bianchi Bonomi Haemophilia and Thrombosis Centre, Instituto di Ricovero e Cura a Carattere Scientifico Fondazione Ca' Granda, Ospedale Maggiore Policlinico, Via Pace 9, 20122 Milan, Italy; e-mail: elena.santagostino@policlinico.mi.it.