Abstract

Background: Sickle cell disease (SCD) is caused by polymerization of Hemoglobin S, resulting in red blood cell (RBC) sickling, RBC destruction, vaso-occlusive episodes and end-organ damage. No direct anti-polymerization, mechanism-based, preventive therapy is available. GBT440 is a novel small molecule hemoglobin modifier which increases hemoglobin oxygen affinity. In vitro and in vivo studies have shown it to be a potent and direct anti-sickling agent with high specificity for hemoglobin, and that 10-30% hemoglobin modification could be both safe (not compromising oxygen delivery) and effective (preventing HbS polymerization). We hypothesized that a potent antisickling hemoglobin modifier should rapidly interrupt RBC hemolysis, improve anemia and potentially become a safe and effective long-term disease-modifying therapy. We therefore explored safety, pharmacokinetics and pharmacodynamics and potential efficacy in healthy volunteers and SCD patients.
Methods: This prospective, randomized, placebo-controlled, double blind, parallel group phase I/II study enrolled healthy volunteers (HV) ages 18-55, and homozygous HbSS SCD patients ages 18-60 with baseline Hb levels ³6 g/dL and ²10 g/dL and without vaso-occlusive crisis or transfusion within 30 days of screening. The study was conducted in two parts: part A tested single ascending doses and part B multiple ascending doses of study drug with 6:2 randomization (GBT440:placebo). Doses administered were: part A, HV cohorts 100mg to 2800 mg, SCD cohort 1000 mg; part B, HV cohorts 300 mg to 900 mg once daily for 15 days, SCD cohort 700 mg once daily for 28 days. The primary endpoint was safety. Secondary endpoints included pharmacokinetics (PK) and pharmacodynamics (PD). Clinical indices of hemolysis were prespecified as endpoints and are described for the SCD multiple dose cohort (700 mg QD for 28 days). Descriptive statistics were used to analyze data.
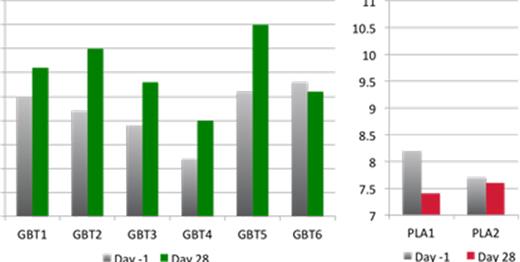
Results: As of July 24 2015, 64 healthy volunteers (HVs) and 16 SCD patients had been enrolled. 54 healthy volunteers had completed the study, 2 were discontinued due to mild-moderate nonserious adverse events (headache, rash) and 8 were in follow-up; 8 SCD patients had completed Part A of the study and 8 were in Part B follow-up. No SCD patients were discontinued; one part B subject had a dose reduction from 700 mg to 400 mg (due to abdominal discomfort). GBT440 was generally well-tolerated, most adverse events were mild, there were no deaths, and there was one serious adverse event (AE) of acute painful crisis in a placebo subject. There were no AEs related to tissue hypoxia. GBT440 showed dose proportional PK, a terminal half-life of 1.5-3 days, high partitioning into RBCs (RBC:Plasma 60-90:1), and a dose dependent increase in hemoglobin oxygen affinity in both HV and SCD patients. In the multiple dose SCD cohort, all patients were evaluable at 28 days (age range 21-52 years; 2 were on hydroxyurea; 3 males/5 females). GBT440-treated patients showed increased hemoglobin, hematocrit and erythrocyte counts with corresponding decreases in LDH, unconjugated bilirubin, reticulocytes and erythropoietin levels with trends evident as early as day 8 compared to no changes in the placebo group (Figure 1 and Table 1). Analysis of peripheral blood smears revealed a marked reduction in sickle cells with GBT440 treatment.
Conclusions: Single, oral, daily dosing with GBT440 was well tolerated across a wide dose range and demonstrated dose proportional and predictable PK and PD. GBT440 demonstrated proof of mechanism with a dose-dependent increase in hemoglobin oxygen affinity without causing tissue hypoxia. GBT440 demonstrated proof of concept in SCD patients with rapid reduction in RBC hemolysis and improved oxygen delivery to tissues as evidenced by reduced erythropoietin level, and a marked reduction in circulating sickle cells. These results support further clinical investigation of GBT440 as a potential disease-modifying therapy for SCD.
| . | Mean change to Day 28 (SEM) . | |
|---|---|---|
| . | GBT440 . | PLA . |
| Hemoglogin (g/dL) | 0.8 (0.2) | -0.5 (0.4) |
| % Sickle cells in peripheral blood (%) | -83 (9) | 19 (4) |
| Erythrocyte count (1012/L) | 0.5 (0.1) | -0.1 (0.2) |
| Reticulocyte count (%) | -2.2 (1) | 0.8 (1.6) |
| LDH (% change from baseline) | -12 (7) | -9 (1) |
| Unconjugated bilirubin (% change from baseline) | -25 (10) | -9.6 (16) |
| Erythropoietin (U/L) | -29 (16) | 21 (33) |
| . | Mean change to Day 28 (SEM) . | |
|---|---|---|
| . | GBT440 . | PLA . |
| Hemoglogin (g/dL) | 0.8 (0.2) | -0.5 (0.4) |
| % Sickle cells in peripheral blood (%) | -83 (9) | 19 (4) |
| Erythrocyte count (1012/L) | 0.5 (0.1) | -0.1 (0.2) |
| Reticulocyte count (%) | -2.2 (1) | 0.8 (1.6) |
| LDH (% change from baseline) | -12 (7) | -9 (1) |
| Unconjugated bilirubin (% change from baseline) | -25 (10) | -9.6 (16) |
| Erythropoietin (U/L) | -29 (16) | 21 (33) |
GBT = GBT440 treated subject; PLA = placebo subject; SEM = standard error of the mean
Lehrer-Graiwer:Global Blood Therapeutics: Employment, Equity Ownership. Howard:Pfizer: Consultancy; Novartis: Consultancy, Other: Travel Grant; Aes-Rx: Consultancy. Layton:Agios: Consultancy; Novartis: Consultancy; Glaxo Smith Kline: Consultancy. Mant:Quintiles: Employment, Equity Ownership. Dufu:Global Blood Therapeutics: Employment, Equity Ownership. Hutchaleelaha:Global Blood Therapeutics: Employment, Equity Ownership. Koller:Global Blood Therapeutics: Employment, Equity Ownership. Oksenberg:Global Blood Therapeutics: Employment, Equity Ownership. Patel:Global Blood Therapeutics: Employment, Equity Ownership. Ramos:Global Blood Therapeutics: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal