Abstract
Introduction: Cytokines play important roles in the activation, proliferation, differentiation and survival of T cells. Previous studies have revealed that individual cytokines selectively activate different T cell populations and also function at specific stages of T cell differentiation. For example, IL-2 supports the development of CD4 regulatory T cells. IL-7 is required for naive conventional CD4 T cell (Tcon) homeostasis, whereas naive CD8 T cell homeostasis requires both IL-7 and IL-15. In contrast, IL-6 promotes Th17 T cell differentiation. The functions of each cytokine are partly defined by the differential expression of specific multi-unit receptors but the selective homeostatic effects of individual cytokines are still incompletely understood.
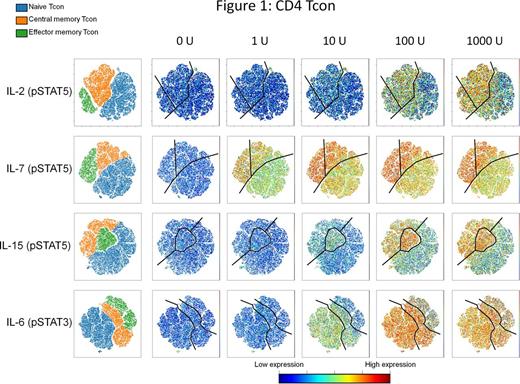
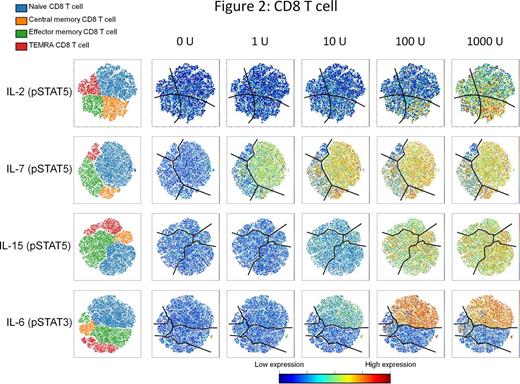
Methods: We stimulated peripheral blood mononuclear cells from healthy donors with varying concentrations of IL-2, IL-7, IL-15 and IL-6 for 15 min in vitro. Single cell mass cytometry (CyTOF) with a panel of 33 markers was used to simultaneously examine signaling pathways activated by each cytokine in distinct T cell subsets. viSNE, a cytometry analysis tool, was used to visualize high-dimensional cytometry data on a two-dimensional map. Expression of pSTAT5 was used to monitor activation induced by IL-2, IL-7 and IL-15; pSTAT3 was used to monitor activation by IL-6.
Results: In CD4 Tcon, relatively high concentrations of IL-2 (100-1000 IU/ml) are required to induce pSTAT5 (Figure 1). However even at high concentrations, IL-2 activation was selective for memory Tcon subsets. In contrast, IL-7 induced pSTAT5 at very low concentrations (1-10 IU/ml). Although all Tcon were affected, activation was more robust in memory than naive Tcon subsets at all IL-7 concentrations. IL-15 activation of pSTAT5 required at least 10 IU/ml and only memory Tcon subsets were activated even at high IL-15 concentrations. Whereas IL-2, IL-7 and IL-15 preferentially activated memory Tcon subsets, IL-6 selectively activated pSTAT3 in naive and central memory (CM) Tcon subsets at low concentrations (10 IU/ml). At high IL-6 concentrations (100-1000 IU/ml) effector memory (EM) Tcon were also activated.
CD8 T cells (Figure 2) are relatively insensitive to IL-2, and only CM CD8 T cells are activated at high IL-2 concentrations (100 IU/ml). Although all CD8 T cell subsets were activated at very high IL-2 concentrations (1000 IU/ml), pSTAT5 activation remained most evident in CM CD8 T cells. Similar to Tcon, IL-7 induced pSTAT5 in CD8 T cells at very low IL-7 concentrations (1-10 IU/ml). However unlike Tcon, pSTAT5 activation was most prominent in naive and CM CD8 T cells. EM CD8 T cells were activated at higher IL-7 concentrations but TEMRA CD8 T cells were resistant to IL-7 stimulation. IL-15 induced pSTAT5 equally in all CD8 T cell subsets but relatively high concentrations (100-1000 IU/ml) were required. Similar to CD4 Tcon, IL-6 induced selective pSTAT3 activation in naive CD8 T cells. Activation of naive CD8 T cells was observed at low concentrations of IL-6 and both EM and TEMRA were resistant to very high IL-6 concentrations (100-1000 IU/ml).
Conclusion: This detailed analysis of cytokine signaling has identified differential effects of IL-2, IL-7, IL-15 and IL-6 on different subsets of CD4 Tcon and CD8 T cells. Whereas CD4 Treg are activated at low IL-2 concentrations, CD4 Tcon and CD8 T cells are relatively resistant to IL-2. At high IL-2 concentrations, activation was most prominent for memory CD4 Tcon and CM CD8 T cells. In contrast, low concentrations of IL-7 are sufficient to activate both CD4 Tcon and CD8 T cells. Within these populations, memory Tcon and naive CD8 cells were preferentially activated at low IL-7 concentrations. Within the CD8 T cell population, IL-15 activated all subsets equally. Within CD4 Tcon, IL-15 preferentially activates memory subsets. IL-6 acts at low concentrations and primarily on naive cells in both CD4 Tcon and CD8 T cells. In all experiments, these effects do not require TCR antigen activation and therefore reflect the potency and differential activity of homeostatic signals supported by these cytokines. Importantly, high concentrations used for in vitro experiments are not likely achieved in vivo but may reflect toxicities of high dose exogenous cytokine therapies or cytokine release syndromes. In contrast, differential effects observed at low concentrations more likely reflect physiologic homeostatic effects of these cytokines in vivo.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal