Abstract
Although chemotherapy regimens induce initial remissions in most acute myeloid leukemia (AML) patients, their long term prognosis is very poor. Novel targeted therapies that effectively eradicate both AML blasts and their progenitors are needed.MCLA-117, a potent human CLEC12AxCD3 bispecific IgG antibody redirects patient's cytotoxic T cells to induce AML tumor lysis. CLEC12A is a myeloid differentiation antigen that is expressed on 90-95% of newly diagnosed and relapsed AML. Moreover, CLEC12A is selectively expressed on leukemic stem cells (LSCs) but not normal early hematopoietic progenitors, including hematopoietic stem cells (HSCs).
MCLA-117 is a full length human bispecific IgG that incorporates CH2 region amino acid substitutions to abrogate Fcγ receptor and C1q interactions while retaining its binding to FcRn. MCLA-117 specifically binds to CLEC12A expressing myeloid cells and CD3 expressing T cells, as evaluated on healthy donor samples by flow cytometry. In line with the CLEC12A expression profile within the hematopoietic progenitor compartment, MCLA-117 did not bind the HSCs, nor the common myeloid progenitor cells. As determined by Surface Plasmon Resonance, MCLA-117 had an affinity of 3 nM for human CLEC12A and 177 nM for human CD3.
The efficacy of MCLA-117 to induce T cell mediated lysis of CLEC12A+ tumor cells was evaluated in cytotoxicity assays. In co-cultures with resting healthy donor T cells and AML tumor cells MCLA-117 efficiently induced CLEC12A antigen dependent T cell activation, T cell proliferation and tumor target cell lysis. MCLA-117 induced tumor target lysis with an EC50 of 66±37 ng/mL. Upregulation of the activation CD69 marker on CD8 T cells was the most sensitive read-out for the activity of MCLA-117 (EC20 of 11±3 ng/mL). Therefore the MABEL (minimum anticipated biological effect level) concentration for MCLA-117 was defined as 10 ng/mL and is used to calculate a safe starting dose in a planned first in human study. MCLA-117 was able to activate and redirect AML patient-derived T cells to CLEC12APOS tumor cells as potently as that of healthy donor-derived T cells.
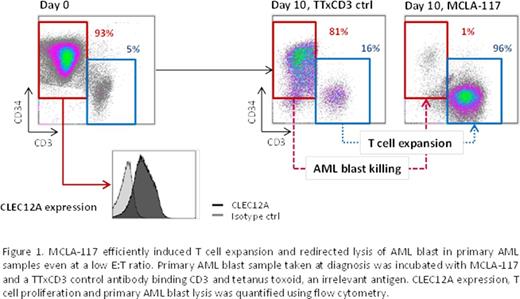
The efficacy of MCLA-117 to induce lysis of AML blasts by autologous T cells in primary AML bone marrow (BM) samples with low T cell to AML blast ratios (E:T ratios of 1:7-1:80) was examined. AML patient BM samples taken at diagnosis were cultured in medium with low amounts of a cytokine cocktail to support in vitro survival of AML blasts. MCLA-117 induced up to 30-fold T cell expansion after 7-10 days. More importantly, MCLA-117 efficiently induced AML blast lysis (up to 88%) in 6/6 tested primary AML patient BM samples, even at very low effector to target ratios (see figure 1).
The cytokine release potential was assessed by incubation of human whole blood and PBMC preparations with MCLA-117. Moderate to strong cytokine release in whole blood was observed (IFNγ, IL-6, IL-8, IL-10 and TNFα) after 24 hours at concentrations of 10,000 and 1,000 ng/mL MCLA-117. At concentration of 100 ng/mL and 10 ng/mL, moderate to low cytokine release and no cytokine release was observed, respectively. In PBMC preparations, moderate to strong IFNγ release was observed after 48 hours at MCLA-117 concentrations of 10,000, 1,000 and 100 ng/mL. At these concentrations, only low release of IL-2, IL-10 and TNFα and no release of IL-1β, IL-6 and IL-8 was observed.
MCLA-117 may provide a novel treatment option for all subtypes of AML with highly specific targeting of myeloid blasts and progenitors and sparing the normal HSCs, as well as eradicating residual LSCs residing in the BM niche compartments. A first clinical study is planned to evaluate the safety and preliminary efficacy of MCLA-117 in adult AML patients.
Van Loo:Merus B.V.: Employment. Doornbos:Merus B.V.: Employment. Shamsili:Merus B.V.: Employment. Bakker:Merus B.V.: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal