Abstract
Introduction. Autologous Bone Marrow Transplantation (Auto-BMT) is currently rarely used in the treatment of Acute Myeloid Leukemia (AML). However, it may represent a good therapeutic option in a specific subset of patients, mainly in consolidation of both low risk (LR) and MRD negative AML without an available HLA matched donor.
Aims. To review our database of AML patients who received Auto-BMT from 2005 to 2014 and who were referred to Bologna Institution, in order to assess the efficacy of the procedure in terms of Overall Survival (OS) and Disease Free Survival (DFS).
Patients and methods: From 2005 to 2014, 98 AML patients underwent Auto-BMT in several Italian Institutions. 89/98 patients are evaluable for survival and outcome data. The 89 patients considered (42 female, 47 male), had a median age of 49 years (range 15-70). Cytogenetics was performed in all patients by conventional karyotype (22 patients were also analyzed by Single Nucleotide Polymorphisms Array); molecular analysis (FLT3 TKD and ITD, and NPM1 mutational analysis) was available for 51/89 patients. Molecular monitoring by specific fusion transcripts (CBF-MYH11 and AML1-ETO) was performed in CBF positive leukemias (inv(16) and t(8;21)) at the time of diagnosis, after induction, consolidation courses, and every 3 months in the first 2 years of follow-up. Based on this data, and according to ELN guidelines, a risk stratification identified 41 patients with a LR AML (t(8:21), inv(16) or NPM1+/FLT3- with normal karyotype), 4 patients with a high risk (HR) AML (complex karyotype or FLT3 ITD mutated or inv(3) or t(6;9)) and 44 patients with a standard risk (SR) AML (normal karyotype, other alterations).
Results. All the patients received an induction chemotherapy treatment, as follows: a "3+7-like" course in 48 cases, a Fludarabine-based regimen in 20 patients and a Gemtuzumab-ozogamicin (GO)-based regimen in 21. 83/89 (93.3%) patients received a median of 2 consolidation courses of chemotherapy (range 1-4) before proceeding to Auto-BMT, performed in 1st CR. 6/89 (6.7%) patients received Auto-BMT in first relapse.
41 patients relapsed after auto-BMT and were treated with a re-induction chemotherapy, or were enrolled in clinical trials. 24 patients reached a 2nd complete remission, and 12 patients underwent an allogeneic BMT in 2nd CR.
With a median follow up of 6 years, the median Overall Survival (OS) of the entire population was 64.3 months (range 5.8-294.2 months); the 1 year OS and the 5 years OS were, 97.1%, and 67.9%, respectively. The median Disease Free Survival (DFS) of the 83 patients treated with Auto-BMT in 1st CR was 36 months (range 1.3-293 months). The 1-year DFS and the 5-years DFS were 85% and 56.7%, respectively. Transplant related mortality (TRM, death in 100 days after BMT) was 1.2% for auto-BMT and 6.5% for allogeneic BMT.
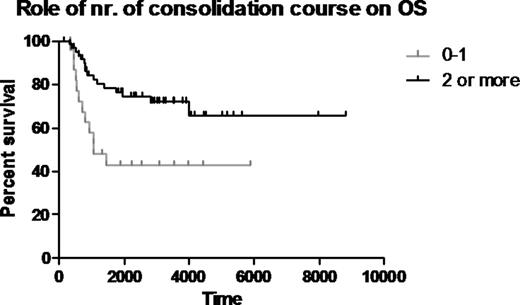
First, to assess the role of the number of consolidation courses we compared patients who received none or 1 consolidation course with patients who received 2 or more cycles, who showed a better OS (p= 0.0061, Figure 1). There was no statistical difference in terms of OS between young and elderly patients (cut off=65 years).
Second, we compared patients who achieved a negative minimal residual disease status before auto-BMT (n=37) with patients who did not (n=9). MRD negativity offered a significantly better outcome in terms of 5-years OS (83.4% and 50% respectively); the median OS of MRD neg was not yet reached; the median OS of MRD pos was 27 months (p= 0.0130) (Figure 2).
Conclusions: Auto-BMT offers a chance to achieve long-term DFS and OS if used as a consolidation therapy both in patients with LR and SR AML. The major role could be played in MRD negative patients, offering the best chances to achieve a long-term OS. Auto-BMT can be also a good choice as consolidation therapy for elderly patients, in which allo-BMT could induce high morbidity and mortality rates. The small patients cohort and the retrospective analysis don't allow us to define the best induction therapy to be used before auto-BMT. However, based on our findings we suggest a therapy schedule including two or more consolidation courses in patients who obtain a first CR, and to proceed then to auto-BMT.
Acknowledgments: work supported by ELN, AIL, AIRC, Progetto Regione-Università 2010-12 (L.Bolondi), Fondazione del Monte di Bologna e Ravenna, FP7 NGS-PTL project.
Soverini:Novartis, Briston-Myers Squibb, ARIAD: Consultancy. Rodeghiero:Celgene Corporation: Honoraria, Research Funding. Cavo:Janssen-Cilag, Celgene, Amgen, BMS: Honoraria. Martinelli:AMGEN: Consultancy; Novartis: Consultancy, Speakers Bureau; Ariad: Consultancy; BMS: Consultancy, Speakers Bureau; ROCHE: Consultancy; Pfizer: Consultancy; MSD: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal