Abstract
Introduction. Conventional induction treatment in young non APL-Acute Myeloid Leukemia (AML) patients is still represented by the association of an antracycline and Cytarabine, which offers a complete remission (CR) rate not inferior to 60%. The addition of Gemtuzumab Ozogamicin (GO) as a third or fourth drug, already demonstrated to improve clinical outcome, in terms of CR rates.
Aims of the study. We retrospectively evaluated and compared the efficacy of different induction schedules, in terms of CR rates and Overall Survival (OS), administered to two groups of AML patients. Group 1 (n=139) was treated with a GO containing course (MyFLAI or MyAIE schedules); Group 2 (n=270) received a non-GO based regimen including or not Fludarabine (FLAI, FLAN, FLAG, 3+7 or DAE).
Patients and Methods. From 1997 to 2014,409 newly diagnosed AML patients were treated in 3 Italian Institutions. Their median age was 53 (range 19-74) and 52 (range 17-75) years, respectively.
According to karyotype (performed in 392/409 patients), FLT3 (available for 244/409 patients), and NPM1 mutational status (available for 157/409 patients), based on the NCCN-2013 risk stratification criteria, 35.2% of the patients were considered at High Risk (HR) (31.6% and 36.4% in the two groups, respectively) and 7.6% at low risk (LR) (7.8% and 7.0%, respectively).
Results. The complete remission (CR) rate after induction was 81.4% and 70.4% for Group 1 and 2, respectively (p=0.01). Deaths during induction (DDI), occurring in the first 50 days from 1st line therapy, were 4/139 (2.9%) in Group 1 and 22/270 (8.1%) in Group 2 (p=0.003).
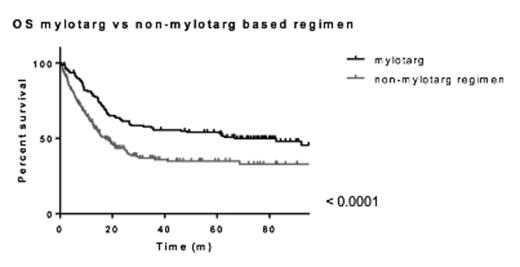
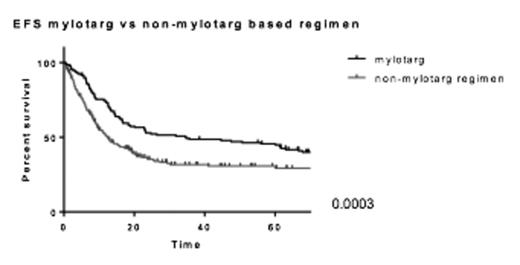
Patients treated with GO showed a better OS than patients of Group 2 (Figure 1); the 5-years OS in the two groups was 54.01% and 34.9%, respectively, and different according to age (54.0% and 34.9% respectively (p=0.0003) in patients <60 years, 30.2% and 13.5% respectively (p=0.001) in patients ³60 years). The 5-years Event Free Survival (EFS) in the two groups was 45.6% and 30.8% respectively (p=0.0003) (Figure 2).
Then, with a logistic univariate regression analysis.,we explored the impact of GO therapy in terms of CR rate. The use of GO was identified as a strong predictor of the achievement of a 1st CR (p=0.008). Moreover, a logistic multivariate regression analysis (risk and age) confirmed the role of the compound as a predictor of higher CR rate (p=0.013).
We also performed a Cox Regression analysis, to investigate the impact of GO therapy, age and risk on OS: the use of GO was confirmed to be an independent predictor of better OS (p<0.0001) with a Hazard Ratio of 1.966 (p<0.0001).
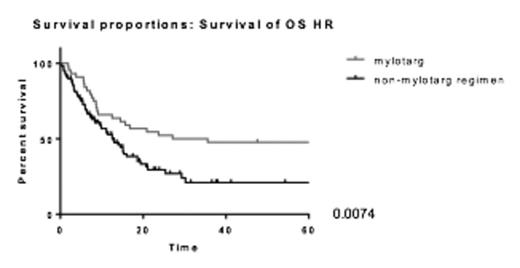
In a sub-analysis performed on HR patients, we observed a significantly better outcome in Group 1 than in Group 2 in terms of OS (p=0.0074, 5-year OS 47.7%; in group 2 OS 21.0% respectively, Figure 3) and EFS (p=0.001). However, there was no difference in terms of CR rate (p=ns). In particular, HR patients with adverse karyotype, may benefit from GO induction therapy in terms of OS (5-years OS 42.9% and 12.8% in Group 1 and 2, respectively, p=0.02); nevertheless FLT3 mutations negative impact canÕt be overcome by the drug administration (5-years OS 66.6% and 61.3% in Group 1 and 2, respectively).
In SR AML, GO offered a better OS (p=0.036, 5-years OS 51.4% and 41.9% respectively).
Comparing with Fisher's exact test the rate of increment in 5-years OS between Group1 and Group2 in HR and SR AML, we demonstrate that treatment with GO gave the higher benefit in HR AML (p=0.0005).
Conclusions. These data showed that a four-drugs intensified induction therapy is a feasible approach in AML patients: adding GO at any induction regimen is an independent and strong predictor of better OS and higher CR rates. In our population, GO was not associated with a higher incidence of DDI.
This approach, could be strongly recommended in SR and HR AML patients, due to karyotype abnormalities, in which showed an advantage in term of OS if compared with other standard regimens. On the contrary, we donÕt suggest the same schedule in FLT3 mutated patients, in which no benefits have been observed.
Acknowledgments Work supported by ELN, AIL, AIRC, Progetto Regione-Universitˆ 2010-12 (L.Bolondi), FP7 NGS-PTL project.
Soverini:Novartis, Briston-Myers Squibb, ARIAD: Consultancy. Fanin:Novartis Farma: Speakers Bureau. Cavo:BMS: Honoraria; Millenium Pharmaceuticals: Honoraria; Jansenn: Consultancy, Honoraria; Sanofi: Consultancy, Honoraria; Onyx: Honoraria; Celgene: Consultancy, Honoraria; Novartis: Consultancy, Honoraria. Martinelli:Pfizer: Consultancy; BMS: Consultancy, Speakers Bureau; Novartis: Consultancy, Speakers Bureau; ROCHE: Consultancy; MSD: Consultancy; AMGEN: Consultancy; Ariad: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal