Abstract

Background: PRF-AML is associated with a dismal prognosis. Approximately one third of patients younger than 60 years, and 50 % of older patients, with newly diagnosed AML, fail to achieve complete remission (CR) with standard induction chemotherapy. Allo-SCT in the setting of active disease is an alternative strategy. The increased availability of unrelated donors (UD) together with the use of reduced-intensity conditioning (RIC) regimens have opened the possibility for transplantation to a larger number of patients in comparison to standard myeloablative regimens (MAC). Because of the high risk of allo-SCT in this setting, there are still questions on the patient outcome depending on the donor type.
Aims:
The current study aimed to compare the outcomes of allo-SCT from matched sibling donors (MSD) (n=660) vs UDs (n=381), for patients with PRF AML.
Methods:
The major endpoints were to assess overall survival (OS), leukemia-free survival (LFS), relapse incidence (RI), and non relapse mortality (NRM).
Results:
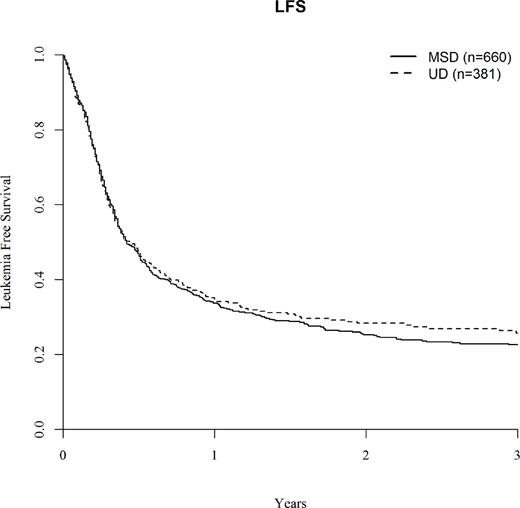
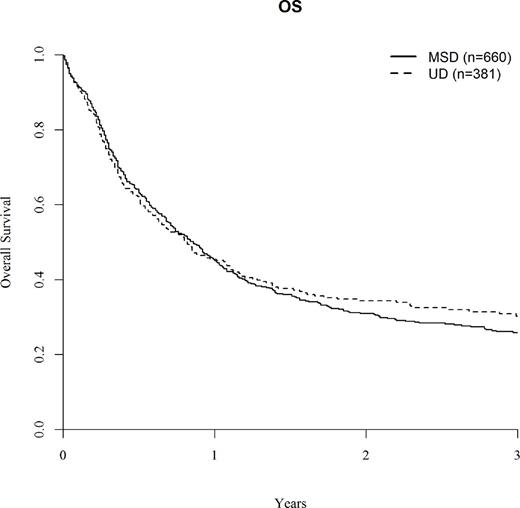
660 patients received a MSD, 296 patients a matched UD (10/10) and 85 a mismatched UD (9/10), respectively. Median age was higher in the UD group (50.5 yrs (18-74) vs 47.7 yrs (18-74), p=0.006). The median time from diagnosis to allo-SCT was similar (110 days [60-180] in the MSD group vs 111days [60-178] in the UD group; p=0.33). In the MSD allo-SCT, 57 % received a MAC regimen, 29% a RIC regimen, and 14% a sequential conditioning regimen; while, in the UD transplants, 44.4 % received a MAC regimen, 24.4% a RIC regimen, and 31.2% a sequential conditioning regimen (p<10-4). Peripheral blood stem cell (PBSC) was the main stem cell source (92% in the MSD allo-SCT vs 94.8% in the UD allo-SCT, p=0.09). Median follow-up was statistically longer in the UD group than in the MSD group (19 months [range, 1.5-143] vs 16 months [2-153], respectively, p=0.04). In univariate analysis, LFS at 2 years was 25.3% in MSD group vs 28.3% in UD group (p=0.56) (Fig.1). In multivariate analysis, 2 predictive factors were associated with lower LFS: cytogenetics (poor vs intermediary; HR=1.61, 95%CI,1.24-2.09, p=0.0004) and time from diagnosis to transplant (above the median 110 days) (HR=1.21, 95%CI,1.02-1.44, p=0.03), whereas Karnofsky status at transplant ≥90% (KS) was associated with better LFS (HR=0.67, 95%CI,0.56-0.80, p=0.0001). In univariate analysis, OS at 2 years was comparable in both groups (30.9% in MSD group vs 34.3% in UD group (p=0.57)) (Fig2). In multivariate analysis, 4 predictive factors were associated with lower OS: age>50 yrs, cytogenetics, time from diagnosis to transplant and CMV positive status whereas Karnofsky status at transplant ≥90% (KS) was associated with better OS. 71% patients with a MSD and 68.6% patents with an UD reached CR after allo-SCT (p=0.73). In univariate analysis, RI at 2 years was 53.7% in MSD group and 56.4% in UD group, respectively (p=0.038). In multivariate analysis for RI, cytogenetics and time from diagnosis to transplant were the only risk factors associated with increased relapse [(HR=1.74, 95%CI,1.30-2.33, p=0.0002) (HR=1.29, 95%CI,1.06-1.58, p=0.01), respectively] whereas KS was a protective factor (HR=0.77, 95%CI,0.62-0.95, p=0.01). The incidence of aGVHD≥2 was higher in UD group (35.5% vs 27.9%, p=0.012). At 2 years, the cumulative incidence of chronic GVHD (cGVHD) was not statistically different between MSD and UD (28.9% and 25.8%, respectively, p=0.56) (univariate analysis). As for, NRM at 2 years, there was not statistical difference between MSD and UD groups (21% vs 25.1%, p=0.112). In multivariate analysis, patient age (>50 yrs) and CMV positive status were factors associated with higher NRM (HR=1.77, 95%CI, 1.27-2.47, p=0.001; HR=1.68, 95%CI, 1.14-2.47, p=0.008), while RIC regimen compared to MAC regimen was the only factor associated with lower NRM (HR=0.59, 95%CI, 0.41-0.85, p=0.005).
Conclusion
Allo-SCT may rescue one third of patients with primary refractory AML. Importantly, the donor type did not have any impact on PRF patients' outcomes. In contrast, time to transplant was a major prognostic factor for LFS and OS. For patients with PRF AML, that do not have a matched sibling donor, allo-HST from UD is a suitable option and thus initiation of an early search and allocating of a suitable donor is therefore indicated.
Finke:Riemser: Research Funding, Speakers Bureau; Neovii, Novartis: Consultancy, Research Funding, Speakers Bureau; Medac: Research Funding. Esteve:Celgene: Consultancy, Honoraria; Janssen: Consultancy, Honoraria. Mohty:Janssen: Honoraria; Celgene: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal