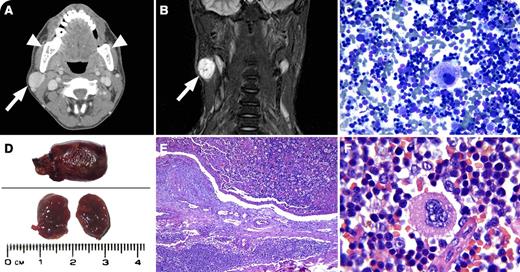
A 24-year-old regularly transfused patient with β-thalassemia major presented with a lateral neck mass. Computed tomography and magnetic resonance imaging showed an enhanced mass 2.3 × 2 × 2.2 cm in the right parotid gland (panels A-B, arrows) with expansion and coarsening of the bony parts (panel A, arrowheads). Differential diagnosis included salivary gland tumors, metastases, hematomas, hemangioma, and extramedullary hematopoiesis (EMH). Fine-needle aspiration of the mass showed normal bone marrow elements (panel C), and EMH was suggested. Pathology showed a soft, dark red, clot-like mass (panel D) that was confirmed as nodal EMH (panels E-F).
EMH and bone changes are well established in β-thalassemia. EMH is primarily seen in untreated or inadequately treated patients with thalassemia major or thalassemia intermedia and may not be prevented even by hypertransfusion regimens,whereas it is very rare in patients with thalassemia major who have received the appropriate treatment. Although EMH is usually primarily restricted to the liver or spleen, soft-tissue masses of EMH are rare. Biopsy is indicated when EMH occurs in very rare and unusual locations to exclude other differential diagnoses. If EMH is in a typical location and is not causing clinical problems, close monitoring without biopsy, in addition to attempts to suppress ineffective erythropoiesis or increase its efficacy, may suffice.
A 24-year-old regularly transfused patient with β-thalassemia major presented with a lateral neck mass. Computed tomography and magnetic resonance imaging showed an enhanced mass 2.3 × 2 × 2.2 cm in the right parotid gland (panels A-B, arrows) with expansion and coarsening of the bony parts (panel A, arrowheads). Differential diagnosis included salivary gland tumors, metastases, hematomas, hemangioma, and extramedullary hematopoiesis (EMH). Fine-needle aspiration of the mass showed normal bone marrow elements (panel C), and EMH was suggested. Pathology showed a soft, dark red, clot-like mass (panel D) that was confirmed as nodal EMH (panels E-F).
EMH and bone changes are well established in β-thalassemia. EMH is primarily seen in untreated or inadequately treated patients with thalassemia major or thalassemia intermedia and may not be prevented even by hypertransfusion regimens,whereas it is very rare in patients with thalassemia major who have received the appropriate treatment. Although EMH is usually primarily restricted to the liver or spleen, soft-tissue masses of EMH are rare. Biopsy is indicated when EMH occurs in very rare and unusual locations to exclude other differential diagnoses. If EMH is in a typical location and is not causing clinical problems, close monitoring without biopsy, in addition to attempts to suppress ineffective erythropoiesis or increase its efficacy, may suffice.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal