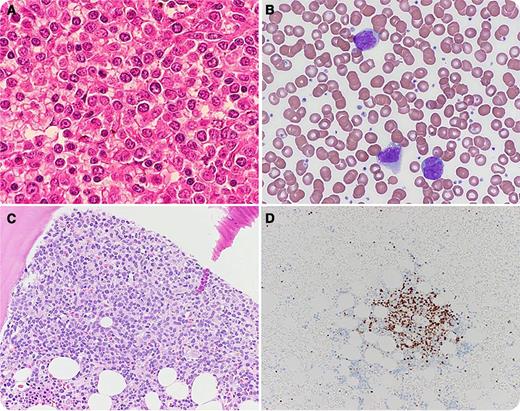
A 56-year-old male presented to the emergency department with acute abdominal pain. Computed tomography scan showed multiple cervical, supraclavicular, periaortic, and mesenteric lymphadenopathy; a ruptured spleen measuring 19 cm; and free intraperitoneal hemorrhage. He underwent an emergent splenectomy and laparotomy. Pathology demonstrated a completely effaced spleen with intermediate- to large-sized lymphocytes with prominent nucleoli admixed with small cleaved lymphocytes (panel A). Neoplastic cells in the spleen were λ light chain restricted and CD5+/CD19+/CD20+ (bright). Fluorescence in situ hybridization results revealed overexpression of CyclinD1 and chromosomal translocation t(11:14)(q13;q32), consistent with mantle cell lymphoma (MCL). Laboratory tests showed white cell count 15.5 × 109/L and 40% lymphocytes. Peripheral smear revealed predominance of large atypical lymphocytes with large nuclei and distinct nucleoli resembling prolymphocytes (panel B). Bone marrow biopsy disclosed paratrabecular and interstitial infiltration of small- to medium-sized abnormal cleaved lymphocytes with large cells with distinct nucleoli (panel C). Immunostaining demonstrated expression of CyclinD1 (panel D) and SOX11, and cytogenetics confirmed chromosomal translocation t(11;14).
Morphology, immunophenotype, and molecular studies are consistent with pleomorphic MCL, previously described as MCL with leukemic variant. Peripheral blood lymphoid cells are similar to prolymphocytes, which may lead to splenic rupture. Thus, it is important to differentiate pleomorphic MCL from prolymphocytic leukemia because the treatments are different.
A 56-year-old male presented to the emergency department with acute abdominal pain. Computed tomography scan showed multiple cervical, supraclavicular, periaortic, and mesenteric lymphadenopathy; a ruptured spleen measuring 19 cm; and free intraperitoneal hemorrhage. He underwent an emergent splenectomy and laparotomy. Pathology demonstrated a completely effaced spleen with intermediate- to large-sized lymphocytes with prominent nucleoli admixed with small cleaved lymphocytes (panel A). Neoplastic cells in the spleen were λ light chain restricted and CD5+/CD19+/CD20+ (bright). Fluorescence in situ hybridization results revealed overexpression of CyclinD1 and chromosomal translocation t(11:14)(q13;q32), consistent with mantle cell lymphoma (MCL). Laboratory tests showed white cell count 15.5 × 109/L and 40% lymphocytes. Peripheral smear revealed predominance of large atypical lymphocytes with large nuclei and distinct nucleoli resembling prolymphocytes (panel B). Bone marrow biopsy disclosed paratrabecular and interstitial infiltration of small- to medium-sized abnormal cleaved lymphocytes with large cells with distinct nucleoli (panel C). Immunostaining demonstrated expression of CyclinD1 (panel D) and SOX11, and cytogenetics confirmed chromosomal translocation t(11;14).
Morphology, immunophenotype, and molecular studies are consistent with pleomorphic MCL, previously described as MCL with leukemic variant. Peripheral blood lymphoid cells are similar to prolymphocytes, which may lead to splenic rupture. Thus, it is important to differentiate pleomorphic MCL from prolymphocytic leukemia because the treatments are different.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal