Abstract
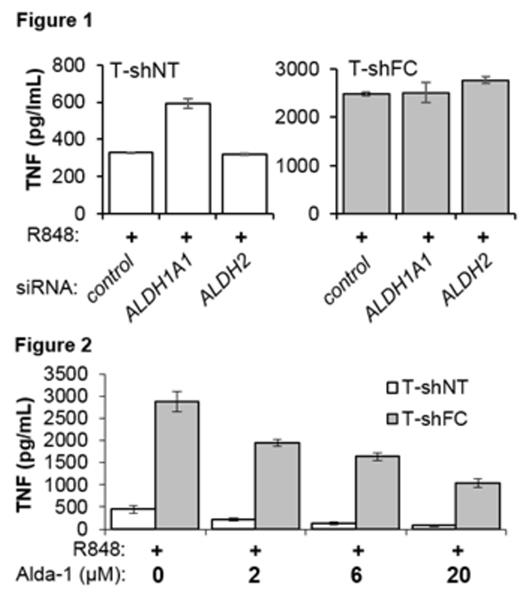
Recent work has clarified a role for aldehyde dehydrogenases in protecting Fanconi anemia (FA) hematopoietic stem cells (HSC) and indicates that the increase in endogenous aldehydes that attends the genetic loss of ALDH function is sufficient to induce bone marrow failure in this disease. Studies in many laboratories have also documented that: (1) exposure of FA HSC to inflammatory cytokines suppresses stem cell self-replication and, in vivo, exhausts the stem cell pool and (2) FA macrophages exposed to specific toll-like receptor (TLR) ligands overproduce the very inflammatory cytokines that suppress the HSC pool. Given that aldehydes form adducts with and, in some cases, activate signaling proteins involved in cytokine production, we tested the hypothesis that overproduction of inflammatory cytokines by FA macrophages results from a loss of FA protein-dependent ALDH function. We treated THP-1 human monocytic leukemia cells expressing shRNA targeting FANCC (T-shFC) or a non-targeted shRNA (T-shNT) with the aldehyde 4-hydroxynonenal (4-HNE) before exposing them to the TLR-7/8 agonist R848. 4-HNE alone did not induce TNF production in either cell line but did enhance TLR-induced TNF overproduction by T-shFC cells (but not T-shNT cells), suggesting that FANCC-deficient macrophages lack factors (e.g., ALDH) that neutralize a signal-enhancing effect of this aldehyde. To directly test the effects of ALDH loss, we pretreated cells with the general ALDH inhibitor diethylaminobenzaldehyde and found that this agent enhanced R848-induced normal production of TNF by approximately 1.6-fold in control cells but did not enhance TNF production in T-shFC cells that were already overproducing TNF. Having determined that ALDH1A1 (but not ALDH2) was highly inducible in both THP-1 cells (by R848) and Lin-Sca-1+Kit+ (by TNF) murine marrow cells, we used siRNA to suppress expression of ALDH2 or ALDH1A1. Knockdown of ALDH1A1 (but not ALDH2) enhanced R848-induced normal production of TNF by approximately 1.8-fold in T-shNT but not TNF overproduction in T-shFC (fig 1) or T-shFA (FANCA knockdown) cells. Our results are consistent with the notion that ALDH1A1 is non-functional in FANCC-deficient macrophages and we confirmed that suspicion in gain-of-function analyses. Specifically, treatment of T-shNT and T-shFC cells with Alda-1 (a small molecule ALDH agonist known to enhance the activity of both ALDH1A1 and ALDH2) suppressed TLR-induced TNF production (fig 2), even in the presence of 4-HNE, by both T-shNT and T-shFC cells. In summary, (1) increasing the aldehyde load in normal macrophages has little influences on the inflammatory response induced by TLR activation but in FANCC-deficient cells aldehydes exacerbate the inflammatory response, (2) suppression of ALDH function with DEAB and specific suppression of ALDH1A1, (but not ALDH2) induces an FA-like phenotype in control macrophages, and (3) pharmacological enhancement of ALDH activity suppresses induced cytokine overproduction by FANCC-deficient macrophages. We conclude that: (1) optimal function of ALDH1A1 is FANCC-dependent in normal macrophages, (2) that the TLR-dependent overproduction of inflammatory cytokines by FANCC-deficient macrophages may result either from an increase in the aldehyde load or the loss of a non-canonical signal-suppressive function of ALDH1A1, and (3) enhancement of ALDH activity using small molecule agonists such as Alda-1 may alleviate the FA macrophage phenotype and may thereby protect HSC from inflammation-induced exhaustion.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal