Abstract
Background: BCR-ABL1-like (Ph-like) B-precursor acute lymphoblastic leukemia (ALL) displays a gene expression profile closely related to B-precursor ALL with t(9;22)(q34;q11). In addition, Ph-like ALL patients (pts) are characterized by distinct genetic alterations and inferior prognosis in pediatric trials. The purpose of this study was the genetic and clinical characterization of Ph-like ALL in adults.
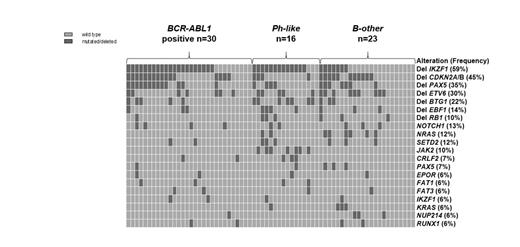
Methods: Affymetrix gene expression profiles (GEP) generated from diagnostic bone marrow samples of 306 adult B-precursor and T-ALL pts (median age 41 years, range 16-84 years) were classified as Ph-like ALL according to published algorithms (Roberts et al., Cancer Cell 2012) and separated from BCR-ABL1-positive and B-other ALL pts (BCR-ABL1-negative; non Ph-like). The incidence and genetic characteristics of the Ph-like subset were analyzed in the overall cohort, whereas clinical and outcome analysis were restricted to B-precursor ALL pts treated within GMALL trials 06/99 and 07/03 (n=107). The median age of this population was 30 (16-64) years. The routine diagnostic work-up included immunophenotyping, fluorescent in situ hybridization (FISH) for BCR-ABL1 and KMT2A (MLL) rearrangements, cytogenetics and molecular analyses of BCR-ABL1 translocations and MLL rearrangements. A subgroup of pts with B-precursor ALL was analyzed for CRLF2 alterations by FISH (n=88) and by RT-PCR for the P2RY8-CRLF2 translocation (n=117). Multiplex ligation-dependent probe amplification (MLPA) for common copy number variations (SALSA MLPA probemix P335-B1) and targeted amplicon sequencing of 131 genes recurrently mutated in ALL were performed in BCR-ABL1 positive (n=30), Ph-like (n=16) and B-other ALL pts (n=23).
Results: Of the 306 pts, we classified 26 pts (9%) as Ph-like ALL based on their GEP and the absence of the BCR-ABL1 translocation, corresponding to an incidence of 13% (26/207) in B-precursor ALL and 24% (26/110) among BCR-ABL1-negative B-precursor ALL.
Nineteen of 107 B-precursor ALL pts treated within the GMALL trials displayed a Ph-like phenotype. There were no significant differences in baseline characteristics like age, sex, white-cell count, hemoglobin or platelet count and risk group in comparison to the B-other subgroup (n=51). All 19 Ph-like pts showed no MLL rearrangement and 58% belonged to the standard risk group. The complete remission rate after induction was similar for Ph-like and B-other pts (96% vs 100%; p>0.05). At 5 years, the Ph-like ALL subgroup had a lower probability of continuous complete remission (RD: 24% vs 63%; p=0.004) and overall survival (OS: 22% vs 56%; p=0.05) compared to B-other ALL pts. After exclusion of pts with MLL rearrangement from the B-other group (n=11), these differences remained significant (RD: 24% vs 62%; p<0.001; OS: 22% vs 64%; p=0.006).
MLPA and amplicon sequencing revealed specific genetic alterations associated with the Ph-like ALL subgroup (Figure 1). All pts with IGH-CRLF2 (n=6) were identified in the Ph-like subgroup, whereas all pts with P2RY8-CRLF2 (n=2) were found in the B-other group (p<0.001 and p>0.05, respectively). Additionally, most pts with high CRLF2 expression clustered in the Ph-like ALL subgroup (13/26, 50% vs 8/79, 10% of B-other; p<0.001). Deletions of IKZF1 were significantly more common in Ph-like ALL (13/16, 81%; p=0.003) and in BCR-ABL1 positive ALL (21/30, 70%; p=0.005) in contrast to B-other ALL (7/21, 30%). Mutations in JAK2 were exclusively found in the Ph-like subgroup (0/53, 0% vs 7/16, 44%; p<0.001). In our data set, FISH for IGH-CRLF2 and sequencing of JAK2 was sufficient to identify Ph-like cases with a sensitivity and specificity of 59% and 100%, respectively.
Conclusion: Ph-like ALL in adults is associated with inferior survival in a homogenously treated group of pts. Additionally, molecular analysis revealed distinct genetic alterations identifying this specific ALL subtype. Since gene expression analysis could be difficult to be implemented in routine diagnostics our data suggest, that testing for JAK2 mutations and the IGH-CRLF2 translocation could be options for the diagnosis of the Ph-like subtype. Future treatment strategies should be explored to improve the dismal prognosis for these high risk pts.
Distribution of common mutations and deletions in adult B-precursor ALL
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal