Abstract
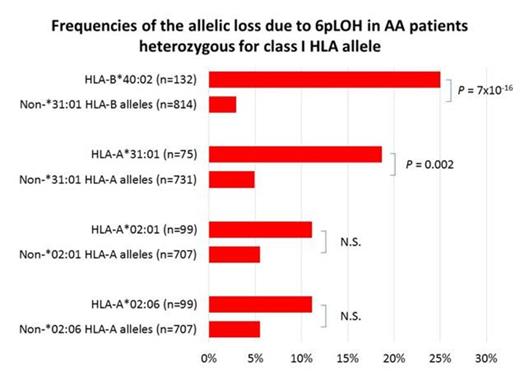
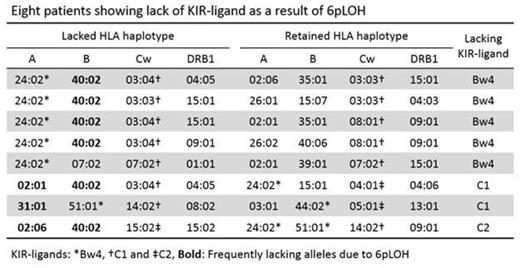
The presence of leukocytes lacking one haplotype of the human leukocyte antigen (HLA) gene as a result of copy-neutral loss of heterozygosity of chromosome 6p (6pLOH) is compelling evidence that cytotoxic T cells (CTLs) have a key role in the development of acquired aplastic anemia (AA). Pathogenic auto-antigens are presumed to be presented by particular HLAs, such as HLA-B*40:02, HLA-A*31:01, HLA-A*02:01 and HLA-A*02:06, all of which are frequently lost due to 6pLOH (Katarigi, Blood 2011). However, this presumption may be incorrect, because the frequency of lacking haplotypes that contain KIR-ligands (KIR-Ls), such as HLA-A*24:02 and HLA-B*52:01, the most frequent alleles of HLA-A and HLA-B, may be underestimated as a result of the killing of 6pLOH(+) leukocytes by NK cells. Indeed, all four frequently missing HLA alleles are non-KIR-Ls. To address these issues, we conducted a mass screening of 6pLOH(+) leukocytes in newly diagnosed AA patients using an assay that allows us to detect 6pLOH(+) cells within one day, and reanalyzed haplotypes that are likely to be lost. The HLA-B and –C allele-specific duplex real time PCR (2qPCR) that we established compared the copy number of heterozygous HLA alleles in a single reaction mixture using two allele-specific TaqMan probes labeled with two different fluorochromes (VIC and FAM) and one primer pair complementary to consensus sequences, which allowed us to detect as small as 5% 6pLOH(+) leukocytes in the total leukocytes. The HLA haplotypes of 6pLOH(+) patients were determined based on the HLA-A antigen expression as demonstrated by flow cytometry and the HLA-B and -C allele data from the 2qPCR, in combination with the haplotype database of the Japanese population available in the HLA laboratory website. A total of 498 patients with AA were subjected to this analysis and 60 6pLOH(+) patients, including 39 6pLOH(+) patients that had been identified by our previous study were used in this analysis. The allelic loss frequencies of HLA-B*40:02 (25%, 33/132) and HLA-A*31:01 (19%, 14/75) were markedly higher than those of the other HLA-B (2.9%, 24/814, P = 7x10-16) and HLA-A (4.9%, 36/731, P = 0.002) alleles, while the frequencies of HLA-A*02:01 (11%, 11/99) and HLA-A*02:06 (11%, 11/99) were similar to those of the other HLA-A alleles. In 41 6pLOH(+) patients possessing either HLA-B*40:02 or HLA-A*31:01, these alleles were all contained in the missing haplotype. On the other hand, four of the 15 patients with HLA-A*02:01(+) haplotypes and two of the 13 patients with HLA-A*02:06(+) haplotypes had these alleles in the retained haplotype. The 6pLOH(+) patients could be divided into three groups according to the status of KIR-Ls (HLA-Bw4 and HLA-C1/C2) of their haplotype; A, the lack of the KIR-L does not occur when either of the two haplotypes is lost; B, the lack of KIR-L occurs when one specific haplotypes is lost; C, the lack of KIR-L occurs when either haplotype is lost. These groups comprised 42%, 53% and 5% of the total. The proportion of group C was much lower than that expected in the general population (16%) and only five (16%) of the 31 group B patients lacked KIR-Ls, thus suggesting that NK cells had an effect on the appearance of 6pLOH(+) leukocytes in AA patients. However, the very high frequency of HLA-loss in the HLA-B*40:02 and HLA-A*31:01 alleles could not be explained by the absence of KIR-Ls in the missing haplotype. Of particular note, the lack of KIR-Ls occurred in eight patients as a result of 6pLOH; six of the eight lost a haplotype containing HLA-B*40:02 and one lost an A*31:01-containing haplotype, suggesting that CTLs specific for autoantigens presented by these class I alleles more dominantly inhibit HSCs than NK cells. Together, these results indicate that HLA-B*40:02 and HLA-A*31:01 have particularly important roles in the presentation of autoantigens to T cells in AA. Studies of T-cell responses to autoantigens restricted by these class I alleles are thus warranted.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal