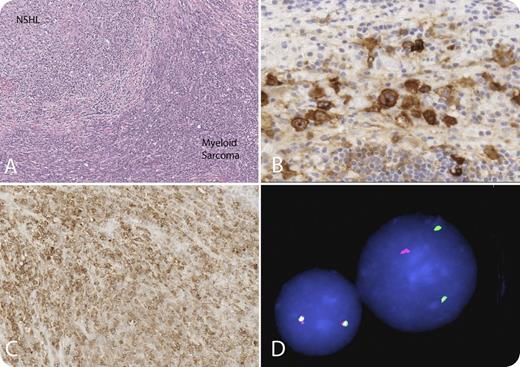
A 19-year-old man with nodular sclerosis Hodgkin lymphoma, diagnosed on mediastinal mass biopsy, was in remission after completing 12 weeks of Stanford V chemotherapy, which includes adriamycin, vincristine, nitrogen mustard, bleomycin, etoposide, and prednisone, followed by radiation to the mediastinum. Two years after diagnosis, the patient was found to have a mediastinal mass and surrounding enlarged lymph nodes. A biopsy demonstrated recurrent Hodgkin lymphoma (panels A-B) and a mononuclear cell infiltrate forming sheets and dissecting between collagen bundles, which immunophenotyped as myeloblasts (panels A-C). Mixed lineage leukemia (MLL) fluorescence in situ hybridization on the paraffin-embedded tissue from the mediastinal mass revealed an MLL rearrangement (panel D). A bone marrow aspirate and biopsy were performed and showed no morphologic evidence of acute myeloid leukemia (AML) or cytogenetic abnormalities, but reverse transcription-polymerase chain reaction for MLL breakpoints t(9;11) was positive in less than 1% of cells. This is an interesting case of nodular sclerosis Hodgkin lymphoma that relapsed after 2 years with concomitant myeloid sarcoma in the same biopsy. Therapy-related AML (TR-AML) with balanced translocations, as seen here t(9;11), is associated with topoisomerase II inhibitors (etoposide) and a short latency period and presents with AML without a preceding myelodysplastic phase, as was the case in this patient.
Although TR-myelodysplastic syndrome/AML has been described in Hodgkin lymphoma, concomitant therapy-related myeloid sarcoma in the same site as recurrence has not been described. Although TR-myelodysplastic syndrome/AML has an overall poor prognosis, the prognosis of a myeloid sarcoma with minimal involvement of the marrow is unclear. At relapse, the patient was treated with 2 cycles of clofarabine, cyclophosphamide, etoposide, and dexamethasone and received a bone marrow transplant.
(A) Hematoxylin and eosin (nodules separated by bands of fibrosis). In the nodules are classic Reed-Sternberg cells. The mononuclear cells forming sheets are the myeloid blasts. (B) CD30 highlights the Reed-Sternberg cells. (C) Myeloperoxidase highlights the myeloid blasts. (D) MLL split apart probe. The yellow signal is normal because they are fused; the red and green signals are separated because there is an MLL rearrangement. Panel D courtesy of Dr Susana Raimondi, St. Jude Children's Research Hospital.
A 19-year-old man with nodular sclerosis Hodgkin lymphoma, diagnosed on mediastinal mass biopsy, was in remission after completing 12 weeks of Stanford V chemotherapy, which includes adriamycin, vincristine, nitrogen mustard, bleomycin, etoposide, and prednisone, followed by radiation to the mediastinum. Two years after diagnosis, the patient was found to have a mediastinal mass and surrounding enlarged lymph nodes. A biopsy demonstrated recurrent Hodgkin lymphoma (panels A-B) and a mononuclear cell infiltrate forming sheets and dissecting between collagen bundles, which immunophenotyped as myeloblasts (panels A-C). Mixed lineage leukemia (MLL) fluorescence in situ hybridization on the paraffin-embedded tissue from the mediastinal mass revealed an MLL rearrangement (panel D). A bone marrow aspirate and biopsy were performed and showed no morphologic evidence of acute myeloid leukemia (AML) or cytogenetic abnormalities, but reverse transcription-polymerase chain reaction for MLL breakpoints t(9;11) was positive in less than 1% of cells. This is an interesting case of nodular sclerosis Hodgkin lymphoma that relapsed after 2 years with concomitant myeloid sarcoma in the same biopsy. Therapy-related AML (TR-AML) with balanced translocations, as seen here t(9;11), is associated with topoisomerase II inhibitors (etoposide) and a short latency period and presents with AML without a preceding myelodysplastic phase, as was the case in this patient.
Although TR-myelodysplastic syndrome/AML has been described in Hodgkin lymphoma, concomitant therapy-related myeloid sarcoma in the same site as recurrence has not been described. Although TR-myelodysplastic syndrome/AML has an overall poor prognosis, the prognosis of a myeloid sarcoma with minimal involvement of the marrow is unclear. At relapse, the patient was treated with 2 cycles of clofarabine, cyclophosphamide, etoposide, and dexamethasone and received a bone marrow transplant.
(A) Hematoxylin and eosin (nodules separated by bands of fibrosis). In the nodules are classic Reed-Sternberg cells. The mononuclear cells forming sheets are the myeloid blasts. (B) CD30 highlights the Reed-Sternberg cells. (C) Myeloperoxidase highlights the myeloid blasts. (D) MLL split apart probe. The yellow signal is normal because they are fused; the red and green signals are separated because there is an MLL rearrangement. Panel D courtesy of Dr Susana Raimondi, St. Jude Children's Research Hospital.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal